ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 12
Which one is best? platelet/lymphocyte ratio, neutrophil/lymphocyte ratio or both in determining deep venous thrombosis in behcet' s disease?
Fatma Erden1, Hatice Karagoz2, Atil Avci3, Deniz Avci4, Ali Cetinkaya4, Siyar Bahadir5 and Abdulsamet Erden4*
1Department of Dermatology and Venereology, Cubuk State Hospital, Ankara, Turkey
2Department of Internal Medicine, Acıbadem Kayseri Hospital, Kayseri, Turkey
3Department of Dermatology and Venereology, Kayseri Training and Research Hospital, Kayseri, Turkey
4Department of Internal Medicine, Kayseri Training and Research Hospital, Kayseri, Turkey
5Hacettepe University Faculty of Medicine, Ankara, Turkey
- *Corresponding Author:
- Abdulsamet Erden
Department of Internal Medicine
Kayseri Training and Research Hospital, Kayseri, Turkey
Accepted on April 20, 2017
Introduction: Behcet's Disease, described in 1937 by Hulusi Behcet, is characterized by oral and genital ulcers, uveitis, arthritis, and involvement of the gastrointestinal tract, central nervous system, and blood vessels, with an unknown aetiology. Although there are many reports about a high neutrophil/ lymphocyte ratio in Behcet's disease; to our knowledge, there is no research in the literature (PubMed database) that evaluates both neutrophil/lymphocyte ratio and platelet/lymphocyte ratio for the patients with thrombosis in Behcet's disease.
Patients and Methods: Overall 331 patients, 61 Behcet's disease patients with a thrombotic complication and 270 Behcet' s disease patients without a thrombotic complication-as the control group-, were included the study.
Results: Of the 61 patients with thrombosis, there was a very significant difference between the genders; 51 (83.6%) were males while only 10 (16.4%) were females (p<0.0001). The median neutrophil/ lymphocyte ratio of the patients with thrombosis was 2.94 (0.9-26.96) while it was 1.78 (0.14-24.29) in the patients without thrombosis. The median platelet/lymphocyte ratio of the patients with thrombosis was 209.95 (64.84-948.21) while it was 118.06 (54.77-393.33) among the patients without thrombosis. There was a statistically significant difference among the patients with and without thrombosis according to the median neutrophil/lymphocyte ratio and platelet/lymphocyte ratio (p<0.0001).
Discussion: Thrombosis was significantly higher in males and female sex was found to be a negative factor against development of thrombosis in both univariate and multivariate analyses. There was no statistically significant difference among the patients with and without thrombosis by means of age. The mean Platelet count was significantly higher in patients with thrombosis. It was found to be a risk factor in univariate analyses while it had no effect on multivariate analyses. Increased platelet/lymphocyte ratio was found to be the most important factor for predicting thrombosis.
Keywords
Behcet's disease, Deep venous thrombosis, Neutrophil/lymphocyte ratio, Platelet/lymphocyte ratio.
Introduction
Behcet's Disease (BD), described in 1937 by Hulusi Behcet, is charactarized by oral and genital ulcers, uveitis, arthritis, and involvement of the gastrointestinal tract, central nervous system, and blood vessels, with an unknown aetiology [1].
International Study Group (ISG) published a set of diagnostic criteria for the diagnosis of BD in 1990. This group defined oral ulceration as the sine qua non and required two other organ involvements (recurrent genital ulceration, eye lesions,skin lesions and positive pathergy test [2]. Vascular disease affects 10-30% of patients which usually presents as superficial or deep venous thrombosis (DVT) and it has a definite male preponderance [3]. Recently, reports showed that a high neutrophil/lymphocyte ratio (NLR) might be related to endothelial dysfunction and reflects BD activitys but to our knowledge, there is no research in the literature (PubMed database) that evaluates both NLR and platelet/lymphocyte ratio (PLR) for the patients with thrombosis in BD [4].
Patients and Methods
Study population
We evaluated the data of 399 patients retrospectively who presented to dermatology and internal medicine clinics of Kayseri Education and Research Hospital between January, 2002 and January, 2015 and dermatology clinic of Çubuk State Hospital between August and December, 2015 and diagnosed as BD according to ISG criteria by using electronic medical records of the hospitals [2]. In the scanning process, patients who had a diagnosed DVT in BD were included the study.
The platelet (Plt) count, white blood cells (WBC) count, neutrophil count and lymphocyte count used for the study were taken from the hospital data of peripheral blood samples of patients at the time of DVT diagnosis.
The blood sample was collected into the tubes containing EDTA. All the haematological analyses were begun to study in the first 30 minutes after the blood sample was collected. Mindray BC-6800 (Senzhen Mindray Biomedical Electronics, Nanshan, P.R.China) was used for the tests.
The diagnosis of DVT was based on imaging techniques findings including Doppler ultrasound and three-dimensional computed tomography (90 % of patients were diagnosed by Doppler ultrasound and the others by computed tomography).
In total, 68 patients with acute infections, surgery, trauma, use of oral contraceptives, immobilization, malignancy, abnormal kidney and/or liver functions, diabetes mellitus, cardiovascular diseases, hematologic disorders, or already undergoing anticoagulant or antiplatelet treatment were excluded.
Overall 331 patients, 61 BD patients with a thrombotic complication and 270 BD patients without a thrombotic complication-as the control group-, were included the study. The local ethics committee has also approved the study.
Statistical analysis
Statistical analyses were performed by using the Statistical Package for the Social Sciences ([SPSS] v 16; IBM Corporation, Armonk, NY, USA). Continuous variables were tested for normal distribution by the Kolmogorov-Smirnov test. The data of descriptive analysis for normally distributed variables were expressed as mean and standard deviations whereas the minimum, maximum and median values were defined for the variables that do not distribute normally. Mann Whitney U test was used for the comparison of groups that do not distribute normally. In comparison of normally distributed groups, Student's t-test was used. Categorical variables were summarized as percentages and compared with the chi-square test.
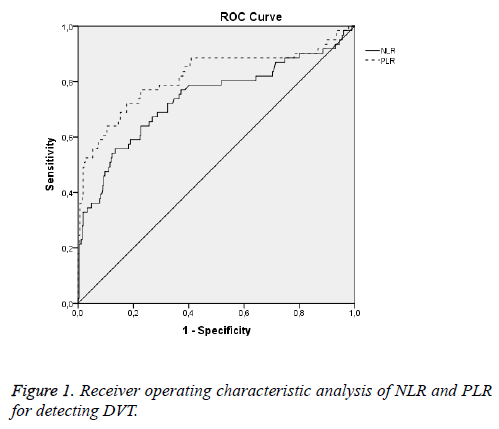
Receiver Operator Characteristic (ROC) curve analysis was used in determining the sensitivity and specify of NLR and PLR in DVT.
The effects of different variables on DVT occurrence in the patients with BD in univariate analysis were analysed for each, and the variables for which the unadjusted p value was <0.10 in logistic regression analysis were identified as potential risk markers and included in the full model. We reduced the model by using backward conditional elimination multivariate logistic regression analyses and eliminated potential risk markers by using likelihood ratio tests. p<0.05 was considered as statistically significant.
Results
In total 331 patients with BD, 177 females (53.5%) and 154 males (46.5%) were included the study. The mean age of the patients was 39.92 ± 11.99 years. Thrombosis was determined in 61 of the patients. Of the 61 patients with thrombosis, there was a very significant difference between the genders; 51 (83.6%) were males while only 10 (16.4%) were females (p<0.0001) (Table 1).
| Thrombosis | p Value | |||
|---|---|---|---|---|
| + | - | |||
| Gender | Male n (%) | 51 (83.6) | 103 (38.1) | 0.0001 |
| Female n (%) | 10 (16.4) | 167 (61.9) | ||
| Total | 61 (100) | 270 (100) | ||
Table 1. The relation of DVT and gender in the patients with BD.
The mean age of the patients with thrombosis was found to be 39.23 ± 10.88 while it was 40.07 ± 12.24 among the patients without thrombosis. There was no statistically significant difference among the patients with and without thrombosis according to the age (p=0.62).
The relation of DVT and BD according to the age, Plt count, WBC count, neutrophil count, lymphocyte count and NLR and PLR have been shown in Table 2.
| Parameters | Thrombosis | p Value | |
|---|---|---|---|
| + | - | ||
| Mean age(± SD) | 39.23 (10.88) | 40.07 (12.24) | 0.62 |
| Mean Plt count/µL (± SD) | 395360 (103724) | 271822 (63544) | <0.0001 |
| Mean HGB g/dL (min/max) | 14.4 (2.06) | 13.67 (1.82) | 0.01 |
| Median WBC/µL (min/max) | 8567 (4500-20360) | 7100 (3100-22590) | <0.0001 |
| Median neutrophil/µL (min/max) | 6000 (2400-15100) | 4000 (340-21130) | <0.0001 |
| Median lymphocyte/µL (min/max) | 2000 (300-5460) | 2200 (870-4670) | 0.024 |
| Median NLR (min/max) | 2.94 (0.9-26.96) | 1.78 (0.14-24.29) | <0.0001 |
| Median PLR (min/max) | 209.95 (64.84-948.21) | 118.06 (54.77-393.33) | <0.0001 |
WBC: White Blood Cells; Plt: Platelet; NLR: Neutrophil/Lymphocyte ratio; PLR: Platelet/Lymphocyte Ratio; SD: Standard Deviation
Table 2. The relation of DVT and BD according to the age, Plt count, WBC count, neutrophil count, lymphocyte count, NLR and PLR.
The mean Plt count of the patients with thrombosis was 395360 ± 103724/μL while it was 271822 ± 63544/μL among the patients without thrombosis. So, there was statistically significant difference among the patients with and without thrombosis according to the Plt count (p<0.0001).
When we investigated the relation between the thrombosis and WBC count; the median value of WBC count was found to be 8567/μL (4500-20360) among the patients with thrombosis while it was 7100/μL (3100-22590) in the patients without thrombosis and this was statistically significant (p<0.0001).
The median neutrophil count of the patients with thrombosis was 6000/μL (2400-15100) while it was 4000/μL (340-21130) in the patients without thrombosis. There was a statistically significant difference among the patients with and without thrombosis according to the median neutrophil count (p<0.0001).
The median lymphocyte count of the patients with thrombosis was 2000/μL (300-5460) while it was 2200/μL (870-4670) in the patients without thrombosis. There was a statistically significant difference among patients with and without thrombosis according to the median lymphocyte count (p<0.0001).
The mean haemoglobin of the patients with thrombosis was 14.4 ± 2.06 g/dL while it was 13.67 ± 1.82 g/dL in the patients without thrombosis and this was statistically significant (p=0.01).
The median NLR of the patients with thrombosis was 2.94 (0.9-26.96) while it was 1.78 (0.14-24.29) in the patients without thrombosis. There was a statistically significant difference among the patients with and without thrombosis according to the median NLR (p<0.0001).
The median PLR of the patients with thrombosis was 209.95 (64.84-948.21) while it was 118.06 (54.77-393.33) in the patients without thrombosis. There was a statistically significant difference among the patients with and without thrombosis according to the median PLR (p<0.0001).
The mean (min-max) erythrocyte sedimentation rate of the patients with thrombosis was 15 (2-120) mm/h while it was 10 (2-47) mm/h in the patients without thrombosis and this was statistically significant (p=0.008.s
The mean (± SD) C-reactive protein of the patients with thrombosis was 9.93 (± 15.11) mg/dL while it was 6.33 (± 15) mg/dL in the patients without thrombosis and this was not statistically significant (p=0.1). The median D-Dimer value of the patients with thrombosis was 290.8 (0.1-1546) ng/mL.
The ROC curves of NLR and PLR for predicting no-reflow are shown in Figure 1. A NLR ≥ 2.12 measured on admission (at the time DVT diagnosed) had a 72.1% sensitivity and 67.7% specificity in predicting no reflow (AUC: 0.739, p<0.0001; [95% CI: 0.658-0.820]). PLR value ≥ 151.63 predicted no reflow with a 77% sensitivity and 77.3% specificity (AUC: 0.817, p<0.0001; [95% CI: 0.744-0.890]).
The association of different variables with DVT in Behcet’s disease was assessed in univariate and multivariate analyses.
Odds ratio (OR) was used for the univariate analyses of patients with DVT in BD. OR for female sex: 0.121 (95% CI: 0.05-0.24, p<0.0001) was found to be a negative factor for the development of thrombosis in the patients with BD, OR for NLR: 1.62 (95% CI: 1.30-2.01, p<0.0001) and OR for PLR 1.023 (95% CI: 1.017-1.030, P<0.0001) were found to be a risk factor alone for the development of thrombosis in patients with BD (Table 3).
| Variables | Univariate Logistic Regression Analysis | Multivariate Logistic Regression Analysis | ||||
|---|---|---|---|---|---|---|
| OR | 95% CI | p value | OR | 95% CI | p value | |
| Age | 0.99 | 0.97-1.01 | 0.619 | - | - | - |
| Female sex | 0.121 | 0.05-0.24 | <0.0001 | 0.103 | 0.037-0.292 | <0.0001 |
| WBC count | 1.000 | 1.000-1.001 | <0.0001 | 1.001 | 1.0-1.0001 | 0.002 |
| Neutrophil count | 1.000 | 1.000-1.000 | <0.0001 | - | - | - |
| Lymphocyte count | 1.000 | 0.99-1.000 | 0.027 | 1.001 | 1.000-1.002 | 0.073 |
| Plt count | 1.000 | 1.000-1.000 | <0.0001 | - | - | - |
| NLR | 1.62 | 1.30-2.01 | <0.0001 | 0.51 | 0.353-0.757 | 0.001 |
| PLR | 1.023 | 1.017-1.030 | <0.0001 | 1.044 | 1.031-1.056 | <0.0001 |
WBC: White Blood Cells; Plt: Platelet; NLR: Neutrophil/Lymphocyte Ratio; PLR: Platelet/Lymphocyte Ratio; OR: Odds Ratio, CI: Confidence Interval
Table 3. Effects of various variables on DVT with Behçet Disease in univariate and multivariate logistic regression analyses.
Multivariate logistic regression model for DVT consisted the variables of female sex, WBC count, Neutrophil count, lymphocyte count, Plt count, NLR and PLR. In the multivariate logistic regression analyses, a PLR value in the highest tertile (OR: 1.044, 95% CI: 1.031-1.056, p<0.0001) was determined as an independent predictor of DVT in BD.
Although the NLR seems to be a risk factor in univarite analyses, it was not found to be an independent predictor of DVT in multivariate analyses (OR 0.51, <95% confidence interval 0.353–0.757; p=0.001) (Table 3).
Discussion
BD is a multisystemic vasculitis of unknown etiology characterized by involvement of both arteries and veins and vessels of all sizes [5]. Thrombosis is the most frequent vascular manifestation in BD patients and DVT and superficial vein thrombophlebitis of lower extremities are the typical manifestations [6].
As expected, thrombosis was significantly higher in males. In our study, female sex was found to be a negative factor for the development of thrombosis in both univariate and multivariate analyses.
There was no statistically significant difference among the patients with and without thrombosis by means of age.
The mean Plt count was significantly higher in the patients with thrombosis. Our finding was similar with the findings of the study performed by Cay et al. In this study they searched platelet activity indices in patients with deep venous thrombosis and they demonstrated the abnormalities of platelet activation in these patients compared to healthy participants. They also suggested that platelet activity indices including mean platelet volume, mean platelet mass and mean platelet component may be used in predicting DVT [7]. In our study, mean Plt count was found to be a risk factor in univariate analyses while it had no effect on multivariate analyses.
The median value of WBC was significantly higher in the patients with thrombosis. In our study, a high median value of WBC was found to be a risk factor in univariate analyses while it had no effect on multivariate analyses. Alan et al. found that WBC, NLR, PLR, neutrophils and platelets were significantly higher in BD patients compared to healthy controls [8]. Also Balta et al. showed high WBC, NLR and C-reactive protein levels in patients with BD compared to controls [9]. A low lymphocyte number was found to be a risk factor for the development of DVT.
Neutrophiles are found to be directly taking roles in the specific lesions of BD and many abnormalities of these cells in BD have been reported in many studies. There are activated and hyperfunctional neutrophiles in BD which have a high phagocytic and chemotactic activity. The oxidative stress caused by chlorinated oxidants derived from these cells may contribute the pathogenesis of BD [10]. Leucocytes and particularly neutrophiles have been shown to play a significant role in atherogenesis and atherothrombosis [11].
NLR is an easy and cheap marker of systemic inflammation and has been investigated in many diseases for years [12]. For example, Yanartas et al. found that NLR can predict postoperative mortality in patients with chronic thromboembolic pulmonary hypertension [13]. Bhatti et al. showed that NLR is a significant independent prognostic indicator in resected pancreatic adenocarcinoma [14]. Ayça et al. found increased NLR predicted stent thrombosis and is associated with higher mortality rates in patients with STsegment elevation myocardial infarction [15]. Recently, reports showed that a high NLR may be related to endothelial dysfunction and reflects BD activity [4]. Ozuguz et al. defined that NLR can be used as an activity marker in patients with BD [16]. Akkurt et al. showed that NLR may be a practical and useful parameter in determining and following disease activity in BD patients with uveitis [17]. Alan et al. found NLR as an associated factor for the presence of BD [8]. Also we found that a high NLR was important for predicting DVT.
Many different cut-off values for NLR have been reported in different studies. In our study, a NLR value higher than 2.12, alone, has 72% sensitivity for predicting thrombosis in univariate analyses; but interestingly, it seems to be a protective factor rather than risk factor in multivariate analyses. Akkurt et al. found that a NLR, at a cut-off value of 1.85 had 62.9% sensitivity and 61.6% specificity in distinguishing the active BD from inactive BD [18]. Alan et al. reported the cut-off value of 2.5 for NLR in their study between the active BD and inactive BD [8]. Conversely, Balkarli et al. stated that NLR didn't statistically differ between active BD subgroups with and without thrombosis [18]. Ozturk et al. suggested that the NLR should be evaluated together with other factors because; the NLR itself alone can't provide enough information about vascular involvement of patients with BD [19].
Although there are many studies about NLR and BD, to our knowledge, there is no research in the literature that evaluates both NLR and PLR for the patients with thrombosis in BD.
Platelets are very important in haemostasis and thrombosis process. They are activated by soluble adhesion molecules and adhere to each other. Following endothelial damage, circulating platelets adhere to the sub endothelial tissue, aggregate and release vasoactive substances and further aggregation occurs. In the end, fibrin production results in thrombotic occlusion. In recent years, various laboratory methods-with different advantages and disadvantages-have been used for the detection of platelet activity. Although considerable amount of research including platelet count and size, aggregates, and released substances from activated platelets has been performed; a practical, reliable and available index of platelet activation has not been discovered yet [7]. We think that PLR can be a useful marker at this point.
PLR is a novel biomarker which can demonstrate the presence and severity of inflammation [20]. Unlike many other inflammatory markers and bioassay, PLR is an inexpensive and readily available marker in predicting thrombosis. It can be calculated easily by the parameters of complete blood count. In recent years, PLR has been investigated in many other conditions. For example, Li et al. reported that a higher PLR is associated with higher stages or tumor recurrence in hepatocelluler carcinoma patients [21]. Racz et al. showed the association of high PLR and reduced recurrence-free survival in patients with gastrointestinal stromal tumors [22]. Smith et al. found that the preoperative PLR was associated with both macroscopic and microscopic features of periampullary tumor invasiveness and it seems to be a more effective marker than CA19.9 in locally advanced disease [23]. Similarly, in another study, Sunbul et al. found that increased PLRs are associated with non-dipper state in hypertensive patients [24]. To our knowledge, this is the first study that shows an association between PLR and DVT in patients with BD.
There are many different cut-off values for different studies in the literature. Ozuguz et al. found PLR value as 133 for active stage in BD patients [16]. Li et al. found that PLR with a cutoff value 111 acts as a prognostic factor for the patients with advanced hepatocellular carcinoma [21]. In our study, a PLR greater than 151 in ROC curve analyses for the patients with thrombosis was significant with 77% sensitivity and 77.3% specificity and it is also important that PLR was the only parameter that predicted thrombosis both in univariate and multivariate analyses.
We also showed that mean platelet volume and mean platelet volume/Plt ratio can also be used as the biomarkers to predict DVT in our previous study in a small number of patient groups (we submitted this manuscript but not published yet).
So we think that, NLR and PLR should be evaluated together for a better result of predicting thrombosis in the patients with BD.
There are some limitations of our study. Firstly, this is a retrospective study. So, the findings of this study did not offer convincing evidence to demonstrate that PLR might be helpful as a biomarker for predicting thrombosis in BD. Second, because of the retrospective nature of the study, we only used spot NLR and PLR values at the time of DVT diagnosis but we couldn' t use follow-up values.
And last there are some limitations about the data. We could not reach any information about the vein thrombosis is either associated with an isolated deep venous thrombosis or another thrombotic area. We also don't know about Behçet’s activity scores of the patients.
These results should be confirmed in larger groups and prospective studies.
Conclusion
The principle findings of this study can be summarised as follows:
• Although ıncreased NLR seems to be a predictive factor for DVT in univariate analyses, this potency disappears in multivariate analyses.
• Increased PLR can predict the risk of DVT development in patients with BD.
Declaration of Conflicting Interest
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- Yurdakul S, Yazıcı H. Behçet's syndrome. Best Pract Res Clin Rheumatol 2008; 22: 793-809
- Seyahi E, Yurdakul S. Behçet's Syndrome and Thrombosis. Mediterr J Hematol Infect Dis 2011; 3: e2011026.
- Mehta P, Laffan M, Haskard DO. Thrombosis and Behçet's syndrome in non-endemic regions. Rheumatology 2010; 49: 2003-2004.
- Balta S, Ozturk C, Balta I, Demirkol S, Demir M, Celik T, Iyisoy A. The Neutrophil-Lymphocyte Ratio and Inflammation. Angiology 2016; 67: 298-299.
- Cebeci F, Onsun N, Ulusal H.A, Inan B. The Relationship between deep vein thrombosis and erythema nodosum in male patients with Behçet' s disease. Eur Rev Med Pharmacol Sci 2014; 18: 3145-3148.
- Emmi G, Silvestri E, Squatrito D, Amedei A, Niccolai E, D'Elios MM, Della Bella C, Grassi A, Becatti M, Fiorillo C, Emmi L, Vaglio A, Prisco D. Thrombosis in vasculitis: from pathogenesis to treatment. Thromb J. 2015; 16: 13:15.
- Cay N, Ipek A, Gumus M, Birkan Z, Ozmen E. Platelet activity indices in patients with deep verin thrombosis. Clin Appl Thromb Hemost 2012; 18: 206-210.
- Alan S, Tuna S, Turkoglu EB. The relation of neutrophil-to-lymphocyte ratio, platelet-to-lymphocyte ratio, and mean platelet volume with the presence and severity of Behcet's syndrome. Kaohsiung J Med Sci 2015; 31: 626-631.
- Balta S, Balta I, Ozturk C, Demirkol S, Koryurek OM, Cakar M, Celik T, Unlu M, Eksioglu M, Demir M, Iyisoy A. Neutrophil lympocyte ratio in patients with Behçet' s disease and its association with carotid intima-media thickness. Am J Card Supplement 2014; 113: 7-11.
- Yazici C, Kose K, Calis M, Demir M, Kirnap M, Ates F. Increased advanced oxidation protein products in Behçet' s disease: a new activity marker? Br J Dermatol 2004; 151: 105-111.
- Horne BD, Anderson JL, John JM, Weaver A, Bair TL, Jensen KR, Renlund DG, Muhlestein JB; Intermountain Heart Collaborative Study Group. Which white blood cell subtypes predict increased cardiovascular risk? J Am Coll Cardiol 2005; 45: 1638-1643.
- Ozturk C, Balta S, Balta I, Demirkol S, Celik T, Turker T, Iyisoy A, Eksioglu M. Neutrophil-lymphocyte ratio and carotid-intima media thickness in patients with behcet disease without cardiovascular involvement. Angiology 2015; 66: 291-296.
- Yanartas M, Kalkan ME, Arslan A, Tas SG, Koksal C, Bekiroglu N, Yildizeli B. Neutrophil/lymphocyte ratio can predict postoperative mortality in patients with chronic thromboembolic pulmonary hypertension. Ann Thorac Cardiovasc Surg 2015; 21: 229-235.
- Bhatti I, Peacock O, Lloyd G, Larvin M, Hall RI. Preoperative hematologic markers as independent predictors of prognosis in resected pancreatic ductal adenocarcinoma: neutrophil-lymphocyte versus platelet-lymphocyte ratio. Am J Surg 2010; 200: 197-203.
- Ayça B, Akin F, Celik O, Sahin I, Yildiz SS, Avci II, Gulsen K, Okuyan E, Dinckal MH. Neutrophil to lymphocyte ratio is related to Stent thrombosis and high mortality in patients with acute myocardial infarction. Angiology 2015; 66: 545-552.
- Ozuguz P, Kacar SD, Akci O, Balta I, Karaca S, Kocak M. Behçet Hastalığının aktivitesini daha pratik ve kolay yöntemlerle belirleyebilir miyiz?. Gulhane Med J 2014; 56: 213-217.
- Akkurt ZM, Turkcu FM, Ucmak D, Yıldırım A, Yüksel H, Yüksel H, Öztürk ZG, Arıca M. The Neutrophil-to-lymphocyte ratio is increased in patients with behçet' s disease. KU Tıp Fak Derg 2014; 16: 4-11.
- Balkarli A, Kucuk A, Babur H, Erbasan F. AB0629 Neutrophil/lymphocyte ratio and mean platelet volume in behçet' s disease. Ann Rheum Dis 2015; 74: 1109.
- Ozturk C, Balta S, Balta I, Celik T. Neutrophil-lymphocyte ratio in behçet disease. Angiology 2015; 66: 695.
- Koseoglu HI, Altunkas F, Doruk S, Etikan I, Demir O, Kanbay A. Platelet-lymphocyte ratio is an independent predictor for cardiovascular disease in obstructive sleep apnea syndrome. J Thromb Thrombolysis 2015; 39: 179-185.
- Li X, Chen ZH, Xing YF, Wang TT, Wu DH, Wen JY, Chen J, Lin Q, Dong M, Wei L, Ruan DY, Lin ZX, Wu XY, Ma XK. Platelet-to-lymphocyte ratio acts as a prognostic factor for patients with advanced hepatocellular carcinoma. Tumour Biol 2015; 36: 2263-2269.
- Racz JM, Cleghorn MC, Jimenez MC, Atenafu EG, Jackson TD, Okrainec A, Venkat Raghavan L, Quereshy FA. Predictive ability of blood neutrophil-to-lymphocyte and platelet-to-lymphocyte ratios in gastrointestinal stromal tumors. Ann Surg Oncol 2014; 22: 2343-2350.
- Smith RA, Bosonnet L, Ghaneh P, Sutton R, Evans J, Healey P, Garvey C, Hughes M, Raraty M, Campbell F, Neoptolemos JP. The platelet-lymphocyte ratio improves the predictive value of serum CA19-9 levels in determining patient selection for staging laparoscopy in suspected periampullary cancer. Surgery 2008; 143: 658-666.
- Sunbul M, Gerin F, Durmus E, Kivrak T, Sari I, Tigen K, Cincin A. Neutrophil to lymphocyte and platelet to lymphocyte ratio in patients with dipper versus non-dipper hypertension. Clin Exp Hypertens 2014; 36: 217-221.