ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 4
Vascular etiology of intracranial hypertension.
1Department of Neurosurgery, “N Oblu” Emergency Hospital Iasi, 2 Ateneului St. Iasi, 700309, Romania
2Department of Neurosurgery, “Gr T Popa” University of Medicine and Pharmacy Iasi, 16 Universitatii St., Iasi, 700115, Romania
3Department of Neurosurgery, “Carol Davila” University of Medicine and Pharmacy Bucharest, 8 Bulevardul Eroii Sanitari , București 050474, Romania
Accepted date: July 17 2014
Intracranial hypertension is an important problem in neurology and neurosurgery. Some authors consider that there are differences between idiopathic intracranial hypertension and intracranial hypertension caused by sinus thrombosis or stenosis, but others consider that intracranial venous sinus thrombosis and stenosis are the main etiological factors for idiopathic intracranial hypertension. The aim of this study was to present the characteristics that differentiate between idiopathic intracranial hypertension and intracranial hypertension caused by intracranial vascular damage. This prospective study included twenty-one patients, 14 women and 7 men of 18 – 61 years old. The main symptoms and the imaging findings diagnosed intracranial hypertension in the absence of an expansive intracranial process, hydrocephalus and intracranial infection. Cerebral angiography with venous phases showed whether there was cerebral vascular disease (cerebral venous thrombosis, venous sinus thrombosis or stenosis). The pressure of the cerebro-spinal fluid was determined by repeated lumbar puncture with manometry after the exclusion of endocranial lesions by cerebral explorations. The analysis of the symptomatology correlated with the values of intracranial pressure, and the imaging findings revealed significant differences between these two types of intracranial hypertension. Vascular intracranial hypertension has a known etiology, such as cerebral vascular illness, and a relatively rapid increase in intracranial pressure of approximately 21 cm H2O. Intracranial hypertension caused by intracranial vascular damage is named vascular intracranial hypertension. The treatment of vascular intracranial hypertension is etiologic, pathogenic and symptomatic, but that of idiopathic intracranial hypertension is only symptomatic.
Keywords
Intracranial hypertension, intracranial venous sinus thrombosis, vascular intracranial hypertension, venous sinus stenosis
Introduction
Intracranial hypertension (ICH) is a common and important problem in neurology and neurosurgery. The symptomatology consisting of vomiting and psychical disorders may be significant for intracranial hypertension and, together with the finding of papillary edema, comprises the pathologic signs for intracranial hypertension. The diagnosis is established by paraclinical investigations (to detect a tumor, traumatic brain injury, obstructive hydrocephalus, meningitis, etc.), but some of the cases are included in the category of idiopathic intracranial hypertension without an identifiable cause [1-3]. Investigators have indicated that intracranial venous sinus thrombosis and stenosis are the main etiological factors for idiopathic intracranial hypertension [4,5]. Others consider that there are differences between idiopathic intracranial hypertension and intracranial hypertension caused by sinus thrombosis or stenosis [6,7]. We believe that venous sinus pathological damage is a vascular cause of intracranial hypertension and that these cases must be included in a vascular etiology of intracranial hypertension, which must be distinguished from idiopathic intracranial hypertension with an unknown cause. The purpose of this study was to identify the differences between the cases of idiopathic intracranial hypertension and cases of intracranial hypertension caused by intracranial vascular damage. This distinction is very important because the therapy is different, either pathogenic and possibly etiologic or only symptomatic.
Materials and Methods
Twenty-one patients (14 women and 7 men) ageing 18 to 61 years were included in a prospective study during the last seven years. Upon admission they presented the clinical symptoms of intracranial hypertension: headache, psychical disorders and papillary edema without the signs of neurological location. The main symptom was diffused cephalous of a progressive nature over a period of several days to several months. The eye fundus examinations showed different aspects, from the incipient aspect of papillary contour blur to the manifestation of papillary edema with venous stasis. The imaging diagnosis involved cranio- cerebral CT and/or cranio-cerebral MRI (with and without contrast), which showed the absence of an expansive intracranial process, hydrocephalus and intracranial infection. Cerebral angio-MRI venous phases showed either there was cerebral vascular disease, such as cerebral venous thrombosis, venous sinus thrombosis or stenosis. In some cases for the diagnosis, angio=CT or cerebral Seldinger angiography was performed. The pressure of the CSF was determined by repeated lumbar puncture with manometry (3 to 4 times), performed after the exclusion of endocranial lesions that produce brain edema by CT or cerebral MRI exploration. In all patients, the following tests were performed: complete blood count, chemistry panel, prothrombin time, activated partial thromboplastin time, the composition of the cerebrospinal fluid with the cerebrospinal fluid proteins and the cellularity. The patients were followed for three months to one year after their diagnosis. All procedures were in agreement with the corresponding guidelines of the European Federation of Neurological Societies (EFNS) [8]. For statistical analysis, we used Mann-Whitney’s U test to compare the cerebrospinal fluid pressure values for patients diagnosed with idiopathic intracranial hypertension and the cerebrospinal fluid pressure values for patients diagnosed with vascular intracranial hypertension. A value of P < 0.05 was considered statistically significant. All the patients gave their written informed consent before the start of the study and the hospital ethics committee approved the study protocol.
Results
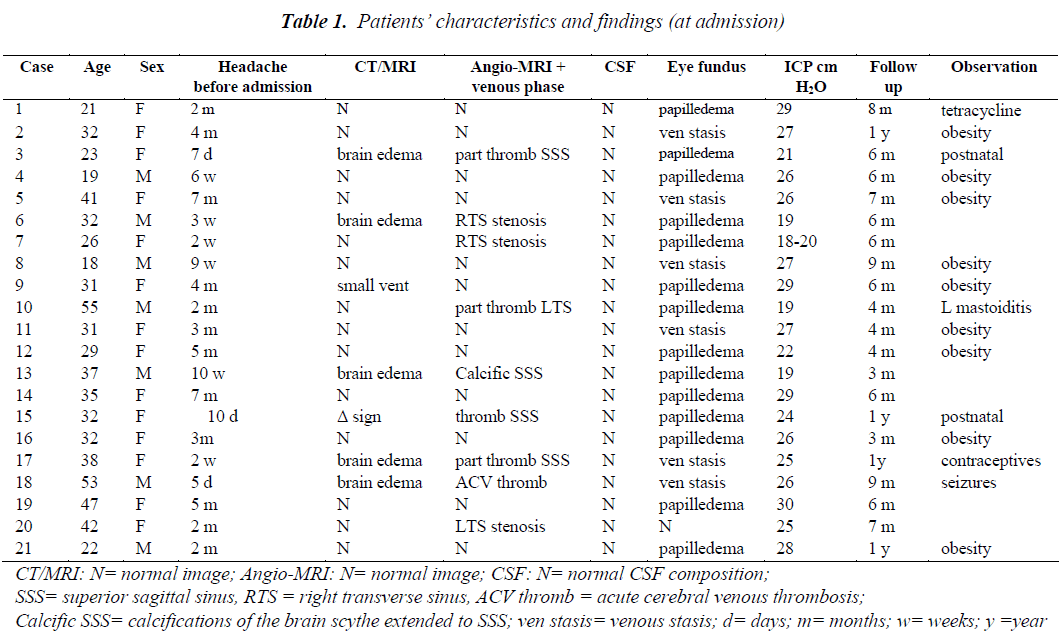
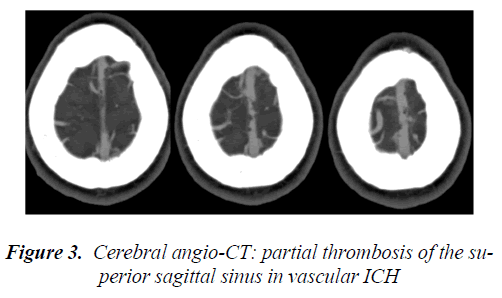
The patients’ characteristics at admission and the findings are presented in Table 1. Patients were grouped into two categories. Twelve patients (3 men and 9 women of 18 – 51 years old) were diagnosed with idiopathic intracranial hypertension based on the clinical symptomatology and the paraclinical investigation results showed normal CT, or only small ventricles (Figure 1), normal MRI and normal angio- MRI including the venous phase. In addition, the cerebrospinal fluid had a normal composition with normal or reduced cerebrospinal fluid proteins and normal cellularity. The pressureof the cerebrospinal fluid was between 22 and 30 cm H2O.
The treatment was individualized for each patient and consisted of the following:
- control of headache with analgesics (e.g., paracetamol and amitriptyline),
- acetazolamide, which reduces cerebrospinal fluid production, with control of the blood electrolyte levels,
- a weight-reduction diet for all patients, especially those who were obese,
- in two cases, only the drainage of cerebrospinal fluid by lumbar puncture was sufficient to control the symptomatology,
- in one patient, progressive visual loss in one eye responded well to oral prednisone.
The treatment during hospitalization spanned between 2 – 4 weeks with clinical improvement, including the resolution of papilledema and the CSF pressure returned to 10 to 12 cm H2O. In addition, the brain MRI was normal. There was no need for surgery to correct the visual function deficit. The patients were observed every 4 weeks after discharge, and follow-ups were conducted from 3 months to 1 year. There were no major complications, and the patients appeared to be stabilized. The visual function of all patients was also normal at the end of the follow-up period.
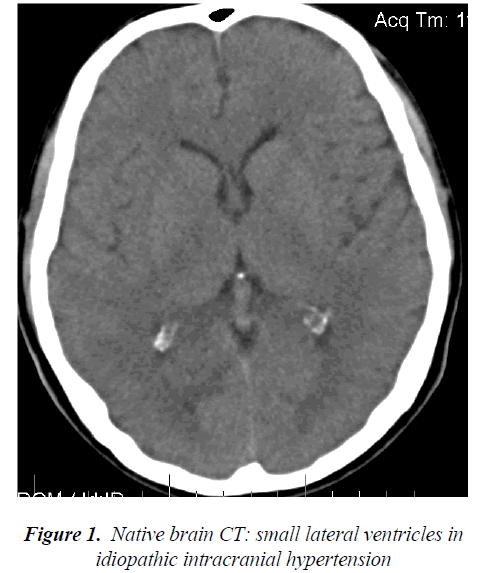
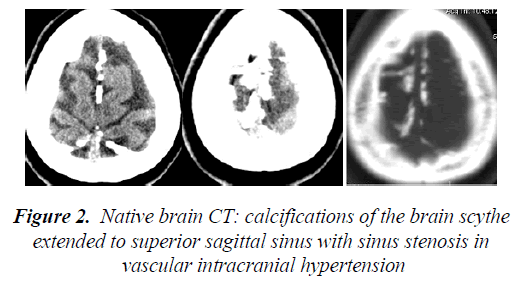
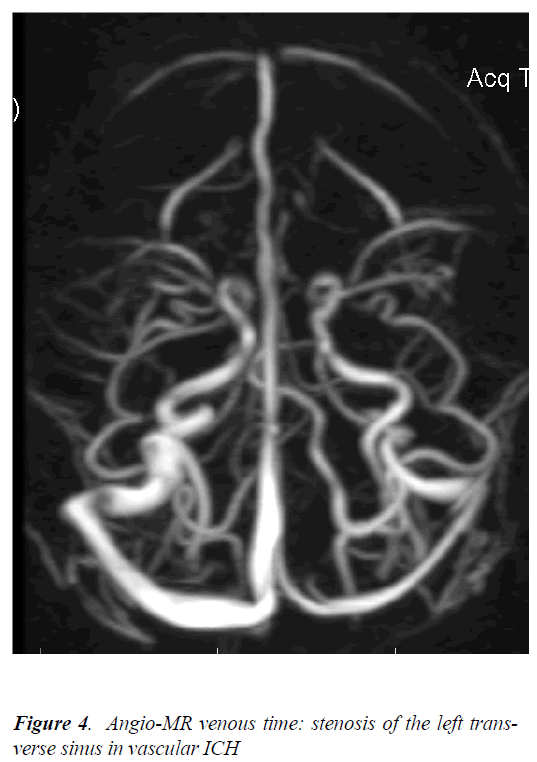
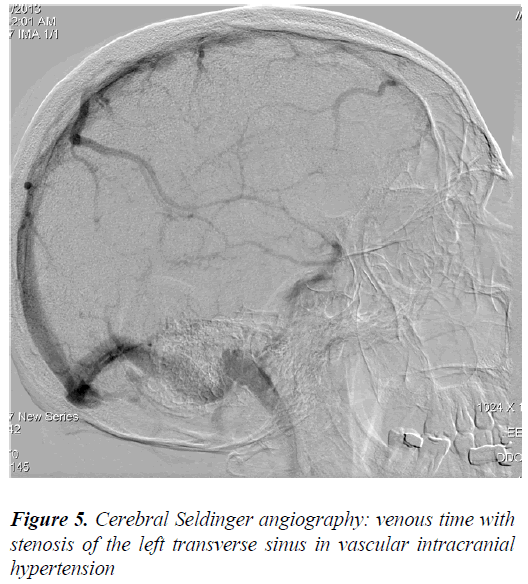
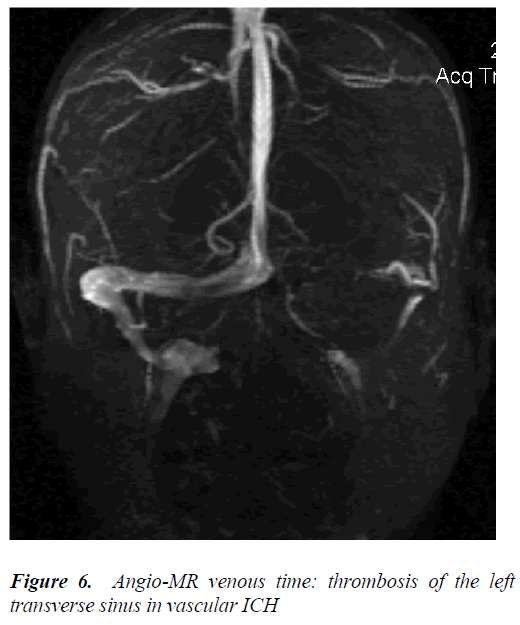
Nine patients (4 men and 5 women of 23 to 61 years old) were diagnosed with intracranial hypertension caused by intracranial vascular damage, such as acute, sub-acute or chronic thrombosis of the superior sagittal sinus, transverse sinus stenosis or acute brain venous thrombosis. The brain CT (native, contrast and angio-CT) showed brain edema in five cases, and the empty Δ sign in one case showed thrombosis of the superior sagittal sinus (Figure 2, 3). The MRI and angio-MRI with venous phase showed characteristic images of thrombosis or partial thrombosis of the intracranial venous sinus in five cases, of stenosis of the transverse sinus in three cases, and of acute cerebral venous thrombosis in one case (Figure 4, 5, 6). The pressure of the cerebrospinal fluid for each patient was between 19 and 26 cm H2O.
The treatment began immediately and mainly consisted of the following:
- anticoagulation to stop blood clot formation in cerebral venous sinus thrombosis,
- which was initially low-molecular-weight heparin and then oral anticoagulation in one case of acute cerebral venous thrombosis and in two cases of women with intracranial hypertension caused by intracranial vascular damage in the postnatal period or only oral anticoagulation in the remaining cases,
- antiepileptic drugs for seizures in the case with acute cerebral venous thrombosis,
- antibiotics in the case with left mastoiditis and partial left transverse sinus thrombosis,
- symptomatic treatment.
Hospitalization of t he patients lasted for 3 – 5 weeks with Clinical improvement after the therapy, including gradual improvement of the papillary edema. The pressure of the cerebrospinal fluid, which was determined before discharge, was between 7 and 11 cm H2O. The MRI after the treatment and before discharge showed partial recanalization of these dural venous sinuses. The follow-up period was 1 month to 1 year.
Discussion
The patients included in this study had headache, different stages of papilledema, elevated CSF pressure on lumbar puncture and normal CSF composition. The cerebral CT and MR images did not show a tumor, hydrocephalus or other etiology, and the diagnosis remained pseudotumor cerebri. According to Foley’s classic definition, Dandy’s diagnosis criteria modified by Wall and Friedman and Jacobson’s diagnosis criteria, one of the diagnostic elements is the non-identification of a cause for the intracranial pressure increase [2,7,9-12]. Idiopathic intracranial hypertension partially corresponds to this historical designation of pseudotumor cerebri, and because of the absence of a clear etiology, idiopathic intracranial hypertension is a diagnosis of exclusion [13].
The group of 12 patients, which we called group A, had all the characteristics to be included in idiopathic intracranial hypertension. The second group of nine patients, which we called group B, also had some of the characteristics of idiopathic intracranial hypertension, but the cerebral CT and MR images showed a cerebral venous sinus thrombosis or stenosis. Therefore, group B was diagnosed with intracranial hypertension caused by intracranial vascular damage [14,15]. The comparison of the characteristics of the two groups revealed differences that enabled a secure diagnosis, which is important because the treatments are different for these two types of intracranial hypertension. The period from the first clinical signs until the complete clinical syndrome in group A was 6 weeks to 7 months. This period was only 5 days to 2 months for group B. The complete clinical syndrome implied an increase in intracranial pressure (ICP), and therefore, this increase in ICP was faster in the cases with a vascular etiology of ICH and slower for idiopathic intracranial hypertension (IdICH). In addition, the values of ICP were higher in the patients with IdICH (group A) over a longer period than in the patients from group B. The increase in ICP was up to 30 cm H2O for group A and only up to 26 cm H2O for group B. Based on all ICP values, the critical ICP values in intracranial hypertension caused by intracranial vascular damage were approximately 21 cm H2O, and the critical ICP values in IdICH were higher, up to 27 cm H2O. This difference indicates that the compensatory mechanisms are not effective due to the faster increase in ICP and that decompensation occurs at a lower ICP value in the cases of intracranial hypertension caused by intracranial vascular damage.
We can designate the intracranial hypertension caused by intracranial vascular damage as vascular intracranial hypertension. The imaging investigations using cerebral CT, cerebral MRI and angio-MRI with the venous phase showed obvious differences between the patients with idiopathic intracranial hypertension and the patients with vascular intracranial hypertension. All patients with IdICH had normal brain CT, brain MRI and angio MRI results or only small ventricles on CT [16,17] (Figure 1). The same investigations showed brain edema and intracranial vascular damage, such as thrombosis, partial thrombosis, stenosis of the intracranial venous sinus or cerebral venous thrombosis, in group B patients (Figure 3 – 6). The presence of brain edema and venous thrombosis may explain the pathogenic mechanisms involved in vascular ICH. Venous sinus outflow obstruction in vascular ICH reduced the venous sinus flow and secondarily decreases the returning venous circulation from the brain, resulting in the appearance of venous stasis and the slowing of brain sanguine circulation. Moreover, the thrombosis or stenosis of the venous sinuses diminished the drainage of the cerebrospinal fluid. The decrease in the venous flux with decrease in the absorption of the CSF caused brain edema. The decreased drainage of the cerebrospinal fluid caused an increased ventricular accumulation of CSF with high intraventricular pressure, and hydrocephalic brain edema. The evolution is progressive, and intracranial hypertension developed [18].
With respect to the etiology, idiopathic intracranial hypertension consists of an intracranial hypertension syndrome without a noticeable etiology. “Associated factors” or “confounding conditions” are the terms used for the different situations under which idiopathic intracranial hypertension occurs without an etiopathogenic relationship, such as metabolic and endocrine disorders, hypovitaminosis A and medications [1,2,4,10,12].
In this study, which included 3 men and 9 women diagnosed with IdICH, the men were young (18,19, and 22 years old) and obese, whereas six women displayed obesity and a young woman of 2-year-old who used oral tetracycline for acne as possible associate factors involved in the development of idiopathic intracranial hypertension. Female sex predominance was evident, and no other factor possibly involved having an etiological relationship with ICH, which is consistent with the data from the literature. The treatment was only symptomatic.
Four men and 5 women, aged between 23 and 61 were diagnosed with vascular ICH, and anamnesis. Imaging findings indicated the cause of the increased intracranial pressure. Two young women presented a clinical syndrome of intracranial hypertension during the postnatal period and were diagnosed with partial thrombosis of the sagittal superior sinus. These two patients displayed good results after the treatment and were followed up for 6 months to one year after their discharge. A 61-year-old man presented with chronic mastoiditis and developed a lateral venous sinus thrombosis on the same side (Figure 6). This patient responded well to antibiotic and anticoagulation therapy.
A 53-year-old man presented with acute intracranial hypertension syndrome of five days duration before admission, and he was diagnosed with acute cerebral venous thrombosis with some characteristics of thrombophlebitis. He also presented with seizures, and the treatment immediately solved the syndrome. He was followed up for nine months with good results. A 47-year-old man had progressive intracranial hypertension syndrome for 10 weeks, and the imaging diagnosis showed calcifications of the brain scythe extending to the superior sagittal sinus, with sinus stenosis (Figure 2) he had only symptomatic therapy. These calcifications obviously occurred over time, with some event triggering the ICH syndrome, which might have been the degree of venous sinus stenosis. The other patients had partial thrombosis of the superior sagittal sinus, and anticoagulation therapy provided good results with partial recanalization of these dural venous sinuses.
There were three cases with venous sinus stenosis and subacute intracranial hypertension syndrome with significant improvement after symptomatic treatment and follow- up for 6 months. Regarding venous sinus stenosis, it has been discussed whether the venous outflow obstruction is the etiology in some cases of intracranial hypertension, and thus, this situation is included in vascular intracranial hypertension. In contrast, some authors allege that venous sinus stenosis is the result of increased intracranial pressure and not the cause of the elevated ICP [19,20]. If the venous sinus stenosis is the cause of the vascular ICH, then the etiologic treatment is therapeutic stent placement in the venous sinuses [21,22]. However, results of stent placement in the venous sinus are inconclusive [23,24]. Karahalios et al. also suggested that increased intracranial venous pressure might be a universal mechanism in pseudotumor cerebri of different etiologies [25], but it seemed that an increased intracranial venous pressure, secondary of venous sinus stenosis or thrombosis possibly resulted in vascular ICH [26]. Therefore, in the cases with a vascular etiology for the intracranial hypertension, we could apply an etiologic treatment and/or a pathogenic treatment as well as the symptomatic therapy.
The presentation and analysis of these cases allowed us to differentiate between the vascular type of intracranial hypertension and idiopathic intracranial hypertension. The name hyperemic intracranial hypertension has been suggested [13], but the designation of vascular intracranial hypertension covers the etiology and pathogenesis better and more completely.
Although the symptoms may be similar in these two diseases, the imaging findings, therapy and evolution are different; therefore, the etiology and pathogenesis are different. Vascular ICH has a known etiology, such as cerebral vascular illness (e.g.,venous sinus thrombosis, venous sinus stenosis and cerebral venous thrombosis), whereas idiopathic ICH has no known etiology or has various nonspecific factors, such as associated factors or confounding conditions (e.g., metabolic and endocrine disorders, hypovitaminosis A and medications). The imaging diagnosis for vascular intracranial hypertension showed a cerebral venous sinus thrombosis or stenosis or a cerebral venous thrombosis in vascular ICH and either normal images or small ventricles in idiopathic ICH. The imaging diagnosis of idiopathic intracranial hypertension excludes other diseases with similar symptoms.
Vascular ICH involves vasogenic brain edema with papillary edema, whereas idiopathic ICH commonly involves papillary edema and diminished visual acuity in some cases. There is also brain edema in idiopathic ICH, but this type of brain edema appears to be balanced by the intraventricular pressure [18].
The increase in intracranial pressure is more rapid in vascular ICH compared with the very slow intracranial pressure increase in idiopathic ICH. In addition, the intracranial pressure values are higher in idiopathic ICH. Therefore, the critical ICP values are smaller in vascular ICH until decompensation of intracranial hypertension. The treatment is symptomatic as well as etiologic and pathogenic in vascular ICH but only symptomatic in idiopathic ICH (including a lumbo-peritoneal shunt or decompression of the optic nerve).
Vascular ICH may potentially include other syndromes, such as hypertensive encephalopathy, but this classification requires further study. In hypertensive encephalopathy, there is a dilatation of brain arteries with increased arterial inflow, increased vascular permeability, and disruption of the blood-brain barrier, which leads to brain edema [27,28].
In conclusion, intracranial hypertension caused by intracranial vascular damage can be called vascular intracranial hypertension. Although it has clinical similarities to idiopathic ICH, there are important differences, such as vascular ICH has a known etiology including cerebral vascular illness, and the increase in intracranial pressure is more rapid in vascular ICH, but the critical ICP values are smaller compared with the idiopathic ICH. The therapy is etiologic, pathogenic and symptomatic in vascular intracranial hypertension, but is only symptomatic in idiopathic intracranial hypertension.
References
- Pearce JM. From pseudotumour cerebri to idiopathic intracranial hypertension. Pract Neurol 2009; 9: 353-356.
- Johnston I. The historical development of the pseudotumor concept. Neurosurgery Focus 2001;11: 1–9.
- Brazis PW. Pseudotumor cerebri. Curr Neurol Neurosci Rep 2004; 4, 111-116.
- Degnan AJ, Levy LM. Pseudotumor cerebri: brief review of clinical syndrome and imaging findings. AJNR Am J Neuroradiol 2011; 32: 1986-1993.
- Farb RI, Vanek I, Scott JN, et al. Idiopathic intracranial hypertension: the prevalence and morphology of sinovenous stenosis. Neurology 2003; 60: 1418-1424 .
- Sylaja PN, Ahsan Moosa NV, Radhakrishnan K, et al. Differential diagnosis of patients with intracranial sinus venous thrombosis-related isolated intracranial hypertension from those with idiopathic intracranial hypertension. J Neurol Sci 2003; 215: 9-12.
- Friedman DI, Jacobson DM. Diagnostic criteria for idiopathic intracranial hypertension. Neurology 2002; 59: 1492-1495.
- Einhäupl K, Stam J, Bousser MG, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol 2010; 17: 1229-1235.
- Wall M. Idiopathic intracranial hypertension. Neurol Clin 2010; 28: 593-617.
- Digre KB, Nakamoto BK, Warner JE, et al. A comparison of idiopathic intracranial hypertension with and without papilledema. Headache 2009; 49: 185-193.
- Biousse V, Bruce BB, Newman NJ. Update on the pathophysiology and management of idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry 2012; 83: 488-494.
- . Friedman DI, Liu GT, Digre KB. Revised diagnostic criteria for the pseudotumor cerebri syndrome in adults and children. Neurology 2013; 81: 1159-1165
- Bateman GA. Vascular hydraulics associated with idiopathic and secondary intracranial hypertension. Am J Neuroradiol 2002 23; 1180-1186.
- Cordell E, Tranmer BI, Adey G, Kohut J. Increased cerebral blood flow in idiopathic pseudotumor cerebri. Neurol Res 1990; 12: 226-230.
- Leker RR, Steiner I. Features of dural sinus thrombosis simulating pseudotumor cerebri. Eur J Neurol 199; 6: 601-604.
- Suzuki H, Takanashi J, Kobayashi K, Nagasawa K, Tashima K, Kohno Y. MR imaging of idiopathic intracranial hypertension. AJNR Am J Neuroradiol 2001; 22: 196-199.
- Hoffmann J, Huppertz HJ, Schmidt C, Kunte H, Harms L, Klingebiel R, Wiener E. Morphometric and volumetric MRI changes in idiopathic intracranial hypertension. Cephalalgia 2013; 33: 1075-1084.
- Iencean SM. Simultaneous hypersecretion of CSF and of brain interstitial fluid causes idiopathic intracranial hypertension. Med Hypotheses 2003; 61: 529-532.
- Lee SW, Gates P, Morris P, Whan A, Riddington L. Idiopathic intracranial hypertension; immediate resolution of venous sinus "obstruction" after reducing cerebrospinal fluid pressure to under 10cmH(2)O. J Clin Neurosci 2009; 16: 1690-1692.
- Stienen A, Weinzierl M, Ludolph A, Tibussek D, Häusler M. Obstruction of cerebral venous sinus secondary to idiopathic intracranial hypertension. Eur J Neurol 2008; 15: 1416-1418.
- Kumpe DA, Bennett JL, Seinfeld J, Pelak VS, Chawla A, Tierney M. Dural sinus stent placement for idiopathic intracranial hypertension. J Neurosurg 2012; 116: 538-548.
- Bateman G. Stenoses in idiopathic intracranial hypertension: to stent or not to stent? Am J Neuroradiol 2008, 29: 215.
- Rohr A, Dörner L, Stingele R, Buhl R, Alfke K, Jansen O. Reversibility of venous sinus obstruction in idiopathic intracranial hypertension. AJNR Am J Neuroradiol 2007; 28: 656-659.
- Lobo S, Ferro JM, Barinagarrementeria F, Bousser MG, Canhão P, Stam J. Shunting in acute cerebral venous thrombosis: a systematic review. Cerebrovasc Dis 2013; 37: 38-44.
- Karahalios DG, Rekate HL, Khayata MH, Apostolides PJ. Elevated intracranial venous pressure as a universal mechanism in pseudotumor cerebri of varying etiologies Neurology 1996; 46: 198-202.
- Kim AW, Trobe JD. Syndrome simulating pseudotumor cerebri caused by partial transverse venous sinus obstruction in metastatic prostate cancer. Am J Ophthalmol 2000; 129: 254-256.
- Kanazawa M, Sanpei K, Kasuga K. Recurrent hypertensive brainstem encephalopathy.J Neurol Neurosurg Psychiatry 2005; 76: 888-890.
- Lee S, Cho BK, Kim H. Hypertensive encephalopathy with reversible brainstem edema. J Korean Neurosurg Soc 2013; 54: 139-141.