ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2011) Volume 22, Issue 4
Thrombocytopenia in Malaria: A clinical study
Department of General Medicine, A J Institute of Medical sciences, Mangalore, Karnataka, India.
- Corresponding Author:
- Nithish Bhandary
Department of General Medicine
A J Institute of Medical sciences
Mangalore, Karnataka
India.
Phone no: 9448023147
E-mail: drnithishmd@yahoo.co.in
Accepted Date: May 27 2011
Objective was to assess the occurrence and severity of thrombocytopenia in hospitalized malaria patients. A total of 102 patients who were hospitalized after confirmation of diagnosis of malaria by malarial parasite fluorescent technique (MPFT) and above 15yrs of age were included in this study. Hematological parameters were determined by using automated analyzer. Those with reduced platelet count were re-evaluated with manual method. In the study group of 102 patients; 50(49.01%) patients had mixed malaria & 46 (45.09%) were positive for plasmodium vivax. Isolated P.falciparum was detected in only 6(5.88%) thus showing that P.falciparum was less seen in this Dakshina Kannada region. Out of 50 cases detected with mixed malaria 38 cases had platelet count less than 1,50000 out of which 9(18%) patients had a platelet count less than 50,000.Out of the 46 patients detected with vivax malaria 34 patients had platelet count less than 1,50000 out of which 5(10.86%) patients had platelet count less than 50,000. Higher frequency of mild to severe thrombocytopenia was observed in hospitalized patients, which should alert the possibility of malarial infection. In this study mixed as well as plasmodium vivax was found to be common species.
Keywords
Malaria, thrombocytopenia, severity, hospitalized patients.
Introduction
Malaria remains today one of the major health problems in most parts of India with increased morbidity and mortality [1]. It causes 300 million new infections and 1 million deaths a year (WHO, 1999). Malaria is the second most fatal communicable disease and is a public health problem in 90 countries in the world, where 40% of the human population live (WHO, 1998).Malaria rates and climatic variables were significantly correlated in the districts of Karnataka, India [2]. Caused by P. falciparum and P. vivax clinically malaria mimics many diseases and there are no absolute diagnostic clinical features. Hematological abnormalities have been observed in patients with malaria, with anemia and thrombocytopenia being the most common [2,3]. Both non-immunological as well as immunological destruction of platelets have been implicated in causing thrombocytopenia but the mechanisms involved are still not completely clear. Immune-mediated lysis, sequestration in the spleen and a dyspoietic process in the marrow with diminished platelet production have all been postulated in the cause for thrombocytopenia [4]. A finding of thrombocytopenia should increase the suspicion of malaria and lead to performance of more specific tests, including multiple peripheral smears and ELISA for parasite-specific antigen [5]. Hence we conducted this study to assess the occurrence of thrombocytopenia in hospitalized patients of malaria and to correlate its severity with the type of malaria.
Materials and Methods
The study was conducted in A.J. Institute of Medical sciences Mangalore which is a tertiary referral center. A total of 102 patients who were hospitalized after confirmation of diagnosis of malaria by malarial parasite fluorescent technique (MPFT) and above 15yrs of age were included in this study.
Exclusion criteria
Patients with acute febrile illness and negative for MP on peripheral blood film or fluorescent technique in three consecutive samples at intervals of twelve hours were excluded. Similarly patients where localizing cause of fever could be determined, patients with history or clinical features suggesting chronic liver disease and those patients with history of bleeding disorder, thrombo-cytopenia or purpura and those with history of drug in take such as fansidar, septran, thiazides and chemotherapeutic agents were also excluded.
Patients were divided into three subgroups based on platelet count. Thrombocytopenia was considered severe if platelet count was <50,000 cells/cmm, moderate if 50,000-100,000 cells/cmm, and mild if 100,000-150,000 cells/cmm.
Results
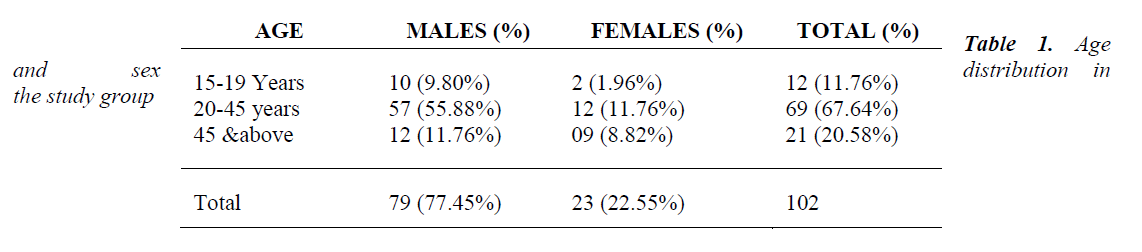
In our study 102 patients with malarial positive was investigated with platelet count. Out of 102 patients 79(77.45%) patients were males and 23(22.55%) patients were females. Majority of the patients were between 20-
45 years (69 patients).[ Table 1]
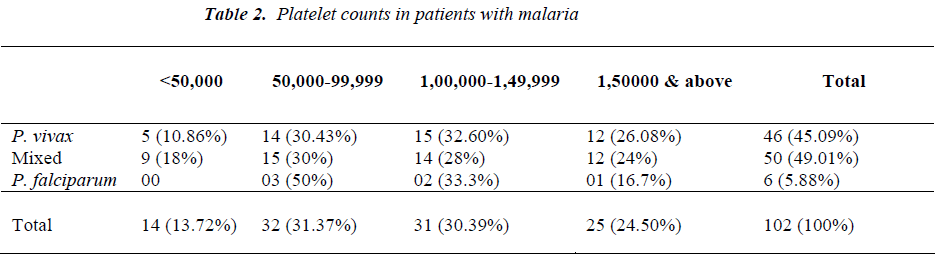
In the study group of 102 patients; 50 (49.01%) patients had mixed malaria and 46 (45.09%) were positive for plasmodium vivax. Isolated P. falciparum was detected in only 6 (5.88%) thus showing that P.falciparum was less seen in this Dakshina Kannada region. Out of 50 cases detected with mixed malaria 38 cases had platelet count less than 1,50,000 out of which 9 (18%) patients had a platelet count less than 50,000. Out of the 46 patients detected with vivax malaria 34 patients had platelet count less than 1,50,000 out of which 5(10.86%) patients had platelet count less than 50,000; thus showing that P.vivax can also result in low platelet count [Table 2].
Discussion
Thrombocytopenia often accompanies malaria and is usually mild to moderate and very rarely symptomatic. Hematological abnormalities are common. Thrombocyto-penia occurs in 60-80% and anaemia in 25% [6]. Finding of thrombocytopenia with anaemia is an important clue to the diagnosis of malaria in patients with acute fes are comparable to studies done by other investigators as 71% by Robinson, Jenney, Tachado, Yung, Manitta, Taylor et al. [7] and 58.97% by Rodriguez-Morales, Sanchez, Vargas, Piccolo, Colina, Arria [8]. Hence patients with acute febrile illness without localizing signs and having combination of anemia and thrombocytopenia should alert the treating physician about the possibility of malaria infection which can be confirmed with specific tests.
Absence of thrombocytopenia is uncommon in the laboratory diagnosis of malaria. Presence of thrombocytopenia is not a distinguishing feature between the two types of malaria. In our study it was found that the prevalence of mixed and P vivax was more than P falciparum, it is usually believed that thrombocytopenia is more common in falciparum malaria. Contrary to the pop-ular belief, P. vivax can also give rise to thrombocyto-penia as was seen in our study.
The mechanism of thrombocytopenia in malaria is not clearly known. Fajardo and Tallent in 1974 demonstrated P. vivax within platelets by electron microscopy and suggested a direct lytic effect of the parasite on the platelets [9]. Both non-immunological destruction as well as immune mechanisms involving specific platelet-associated IgG antibodies that bind directly to the mala-rial antigen in the platelets have been recently reported to play a role in the lysis of platelets and the development of thrombocytopenia. In clinical trials, recombinant – macro-phage colony stimulating factor (M-CSF) has been known to cause a reversible dose dependent thrombocytopenia. Elevated M-CSF levels in malaria, by increasing macrophage activity may mediate platelet destruction in such cases [10]. Oxidative stress damage of thrombocytes has also been implicated in the etiopathogenesis based on the finding of low levels of platelet superoxide-dismutase and glutathione peroxidase activity and high platelet lipid peroxidation levels in malaria patients, when compared to those of healthy subjects [1].Conclusion
Higher frequency of mild to severe thrombocytopenia was observed in hospitalized patients suffering from malaria, and mixed as well as plasmodium vivax was found to be common species in these cases. The above findings can have therapeutic implications in context of avoiding unnecessary platelet infusions with the relatively more benign course in P. vivax malaria. We propose that the platelet count can serve as an important initial screening tool in this setting.
References
- Makkar, RPS, Mukhopadhyay S, Monga A, Gupta AK. Plasmodium Vivax Malaria Presenting With Severe Thrombocytopenia. The Brazilian Journal of Infectious Diseases 2002; 6 (5):263-265.
- http://www.brown.edu/Research/EnvStudies
- Khan SJ, Khan FR, Usman M, Zahid S. Malaria can lead to Thrombocytopenia. Rawal Med J 2008; 33: 183-185.
- Jadhav UM, Patkar VS, Kadam NN .Thrombocyto-penia in Malaria - Correlation with Type and Severity of Malaria.JAPI 2004; 52: 615-618.
- Patel U, Gandhi G, Friedman S, Niranjan S. Thrombo-cytopenia in Malaria. Journal of the national medical association 2004; 96 (9): 1212-1214.
- Ansari S,Khoharo HK, Abro A, Akhund IA,Qureshi F. Thrombocytopenia in plasmodium falciparam malaria.J Ayub Med Coll Abbottabad 2009;21(2): 145-147.
- Robinson P, Jenney AW, Tachado M, Yung A, Manitta J,Taylor K et al. Imported malaria treated in Melbourn Austrlia: Epidemiology and clinical features in 246 patients. JTravel Med 2001; 8:76?81.
- Morales AJ, Sanchez E, Vargas M, Piccolo C, ColinaR, Arria M. Anemia and Thrombocytopenia in children with Plasmodium vivax malaria. J Trop Pediatr. 2005; 10: 1093-1097.
- Fajardo L.F, Tallent C. Malarial parasites within human platelets. JAMA 1974; 229: 1205-1209.
- Lee S.H, Looaresuwan S, Chan J, et al. Plasma macro-phage colony stimulating factor and P-selection levels in malaria associated thrombocytopenia. Thromb Haemost 1997; 77 (2): 289-293.