ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 1
The effects of emergent endoscopic variceal sclerotherapy combined with acrylate glue injection on esophageal variceal bleeding
Department of Gastroenterology, Chinese PLA General Hospital, Beijing 100853, PR China
- *Corresponding Author:
- Yunsheng Yang
Department of Gastroenterology
Chinese PLA
General Hospital
PR China
Accepted date: June 01, 2016
Background: To evaluate the hemostatic effects of emergent Eendoscopic Variceal Sclerotherapy (EIS) combined with acrylate glue (N-butyl-2-cyanoacrylate, NBCA) injection (ESCI) on esophageal variceal bleeding, and to investigate glue extrusion after endoscopic injection.
Methods: The rate of hemostasis and blood transfusion in patients that received ESCI were compared to 16 patients who received intervention therapy following the failure of endoscopic treatment. The glue extrusion time and complications of ESCI were also analyzed.
Results: Of the 30 patients that received ESCI therapy no heterotopic embolism or serious infection. Transient fever was found in 6 cases, dysphagia in 9 cases and severe dysphagia in 2 that were treated by endoscopy. NBCA (1~4 vials, mean 2.03 ± 0.182 vials) was injected into esophageal varices and glue extrusion from varices was started at 2 weeks (9 cases, 36%) to 3 weeks (15 cases, 60%) after the injection, completed at week 2~4 (88%). In patients receiving interventional therapy, no significant difference was found in the rate of hemostasis.
Conclusion: ESCI can effectively control acute esophageal variceal bleeding without heterotopic embolism. However, early glue extrusion could cause esophageal obstruction.
Keywords
Esophageal varices, Endoscopic variceal sclerotherapy (EIS), NBCA injection, Glue extrusion
Introduction
Esophageal Varices (EV) are a serious complication of liver cirrhosis. The mortality for cases with variceal bleeding was at least 20% within 6 weeks, and for untreated patients rebleeding rate was 70% within 1 year [1]. Endoscopic therapy is one of the most effective therapeutic methods to prevent re-bleeding, including Endoscopic Variceal Ligation (EVL), EIS and injection of tissue adhesives (NBCA) [2].
NBCA injection is the most effective treatment for gastric fundus varices [3,4], while limited by its serious complication of heterotopic embolism [5]. EIS is a common therapeutic method for EV, especially in cases of acute bleeding and/or impracticable EVL therapy [6,7]. NBCA injection is a good supplement for those patients where EIS could not control acute or refractory bleeding [8].
In this study we compared the clinical data of 30 patients with esophageal variceal bleeding, where EIS failed before being combined with NBCA injection, to 16 patients who received interventional therapy using balloon tamponade during the same period. This study aimed to explore the feasibility of this combined therapy, the characteristics of glue extrusion, and the treatment/prevention of complications in EV.
Materials and Methods
Patients
From January 2002 to December 2011, endoscopic diagnosis and treatment were conducted 4354 times in 2223 patients with gastroesophageal varices in our hospital. Clinical data, therapeutic methods and efficacy of ESCI therapy performed 31 times for 30 EV bleeding patients were summarized. These were compared to 16 EVB patients where initial endoscopic treatment failed and they underwent interventional therapy using balloon tamponade. The diagnosis, treatment and data collection were approved by the institutional ethics committee and informed written consent was obtained from all patients that participated in this study.
Material preparation
Fujinon EG-410G prior view endoscopy (or EG-450G oblique view endoscopy; Boston sclerosing injection needle (25G and 23G); 1% ethoxysclerol (Germany, or China Donglin Co.); 5% sodium morrhuate (Shanghai Donghai Pharmaceutical Factory); NBCA (Histoacryl, B Braun,Melsungen,Germany; or China Donglin Co) and lipiodol (Guerbet, Aulnay-Sous-Bols, France). The indications for the procedure were: (1) Portal hypertension; (2) Patients with history of hemorrhage due to esophageal and gastric varices rupture; (3) Patients with rough varices or unclear vision in the emergency operation and (4) Patients with esophageal varices residue which were not suitable for ligation treatment.
Methods
Routine endoscopy was carried out first. For those patients who were unsuitable for EVL following EIS, bulky or flaky varices, need supplementary therapy after EVL, and unclear endoscopic visual field due to active bleeding, EIS was performed (with 1% ethoxysclerol and/or 5% sodium morrhuate). Supplementary NBCA injection was delivered using sandwich method for patients with uncontrolled bleeding or active bleeding following removal of the sclerosing needle [9]. NBCA was injected at a dose of 0.5~2.0 ml following which EIS was performed on other varices. In the 16 patients where endoscopic therapy failed but did not undergo tissue adhesive injections were given balloon tamponade treatment and underwent interventional radiology treatment, including Transjugular Interhepatic Portosystemic Shunt (TIPSS), gastric coronary vein embolization and splenic embolization.
Post-endoscopic treatment and follow-up: patients received oral semi-soild food 6-8 hours after the procedure, intravenous injection of antibiotics for 3 days and then received the EIS after an interval of 1 week. Endoscopy was performed weekly till week 5, and then every 3 months (or based on endoscopic findings in few cases). Routine CT examination and X-ray scan of chest/abdomen were performed to observe the glue extrusion at intervals of 3 days, 2 weeks (or 3 weeks), 1 month and 2 month following the injection. Patients with interventional radiology treatment underwent endoscopy, abdominal ultrasound; CT scan examinations 3 months later to investigate the recurrence of varices, further endoscopic treatments were conducted if risk factors, such as red sign, were found.
Results
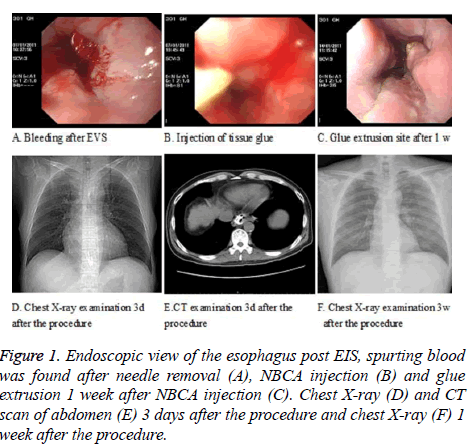
A total of 30 patients with esophageal variceal bleeding were recruited in our study (20:10 males/females), age 18~74 (mean 51.86 ± 12.94 years old) and their clinical characteristics were analyzed. In terms of etiological factor, they consisted of 1 case of congenital hepatic arterioportal fistula, 29 cases of liver cirrhosis. The liver cirrhosis cases consisted of hepatitis B induced cirrhosis (21 cases), hepatitis C induced cirrhosis (3 cases), alcoholic cirrhosis (3 cases), auto-immune cirrhosis 1 case and congenital liver fibrosis 1 case. Child-Pugh class was grade A (5 cases), grade B (11 cases) and grade C (14 cases). There were 5 patients with concomitant primary hepatocellular carcinoma. Among the patients that received ESCI therapy, there were 8 cases unsuitable for EVL after EIS, 9 cases unsuitable for EVL therapy due to bulky or flaky varices, 12 cases had unclear visual field due to active bleeding and 2 cases had bleeding following EVL. Bleeding was successfully controlled in 30 (96.77%) out of 31 times that ESCI was used (The procedure were showed in Figures 1A-1F) and for the case where it failed to control bleeding, the patient underwent TIPSS therapy following the administration of vasoactive drugs to achieve hemostasis. Subsequent EIS was performed weekly following ESCI therapy.
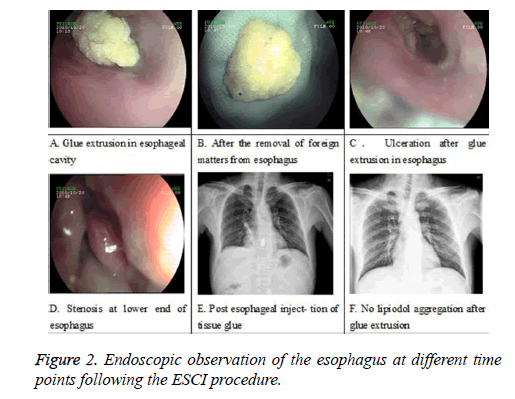
No heterotopic venous embolism or serious infection was recorded during this period. Minor symptoms such as transient fever (6 cases) which restored to normal body temperature after anti-inflammatory therapy and swallowing discomfort or dysphagia (9 cases, mostly mild and capable of normal diet) occurred. Two of these patients had serious esophageal stenosis caused by early glue extrusion(Figures 2A-2F) and NBCAlipiodol mixture evidenced by endoscopy (Figure 2A) and chest X-ray (Figures 2A, 2C and 2D) (i.e. 3.0 × 2.5 cm and 3.4 × 4.0 cm in diameter respectively). Of these 2 patients, 1 had evident symptom of dysphagia 2 weeks after the therapy due to past history of esophageal stricture (Figure 2D), and the other had cardiac obstruction due to ulceration at subsequent therapy. In both cases, dysphagia was relieved by endoscopic removal of the NBCA-lipidol mixture from the esophagus (Figure 2B). 16 cases with refractory bleeding (due to failed endoscopic sclerotherapy and ligation of esophageal varices) were treated using interventional radiology with balloon tamponade. Among these patients, hemorrhagic shock occured in 15 cases; TIPSS was carried out in 13 cases; among them, gastric coronary vein embolization conducted under TIPSS in 6 cases, splenic arterial embolization in the other 3 cases. The rate of hemostatis was 100%. The average blood transfusion was 11.7 u during hospitalization. During more than 30 months followup, no re-bleeding was found. Prophylactic endoscopic treatment was applied in 2 cases with high risk of re-bleeding evidences.
Two patients with advanced hepatocellular carcinoma and portal vein cancerous thrombosis discharged themselves from the hospital after successful hemostasis, three patients left hospital after the therapy without follow up; and the remaining 25 patients were followed up for 12 months to 36 months, average time was 20.23 ± 19.77 months. One of the patients that received TIPSS therapy following failed endoscopic treatment had no re-bleeding in the subsequent 30 months. One patient with EV bleeding induced by congenital hepatic arterioportal fistula died of massive upper gastrointestinal bleeding 2 months after therapy. Three patients with hepatocellular carcinoma died of liver failure 3~7 months after ESCI therapy. Six cases showed EV recurrence within 6 months to 12 months following treatment. Among these 6 patients, 4 had endoscopic therapy performed again, and 2 cases underwent surgical therapy. Among the 14 patients with regular follow-up, there was no evidence of re-bleeding related to EV.
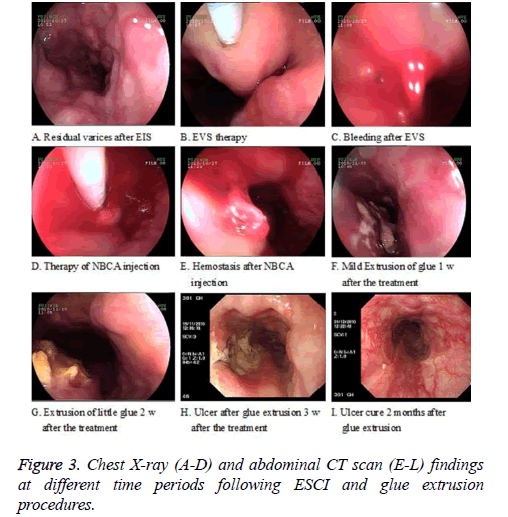
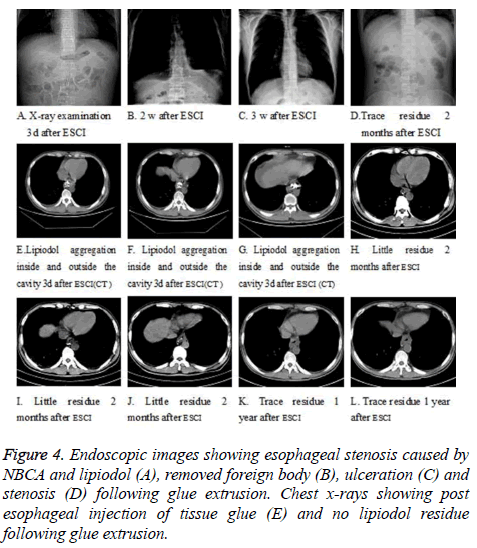
Twenty-five patients were followed up after glue extrusion by recording their symptoms, endoscopy (Figures 3A-3I), X-ray and (Figures 4A-4D)/or CT examination (Figures 4E-4L). As found by endoscopy, glue extrusion occurred with the endoscopic protrusion of spotted or nodular yellow-white colloid substances into esophageal cavity 1~2 weeks after esophageal ESCI therapy (Figures 3F-3G) and 2~4 weeks after the operation (Figure 3H). Following the glue extrusion, shallow longitudinal shape ulcers of different sizes formed (Figure 3H), the varices disappeared, the surface of ulcer was covered with yellow-white moss in short time (about 1-2 weeks), and scar tissue formed after the ulcer healed treated (Figure 3I). As found by chest X-ray examination 3 days after ESCI therapy (Figure 4A), lipiodol aggregated in the form of cylinder, stripe and node based on the shape of the local blood vessel (vessel casting) (Figure 4E). As shown by endoscopic observation, the glue extrusion started from week 1 (9 cases, 36%), week 2 (15 cases, 60%), and week 4 (1 case, 4%) respectively; completed through 2 weeks (3 cases, 12%), 3 weeks (15 cases, 60%), 4 weeks (4 cases, 16%), and 5, 8 and 12 weeks (1 case, 4% each). Glue extrusion lasted an average of 1 week (15 cases, 60%), 2 weeks (7 cases, 28%), and 3, 6 and 11 weeks (1 case, 4% each). Two weeks after glue extrusion, a little lipiodol still remained on chest X-ray examination. Among the patients with endoscopic glue extrusion (CT examination); a trace amount of lipiodol appeared in the esophageal cavity; a little lipiodol aggregated in the periesophagus or paraesophagus toward the fundus side (Fig. 3H-4L).
Discussion
EIS was first reported by Crafoord and Frenckner for esophageal variceal bleeding in 1939, and widely applied in clinical practice after 1973. In 1986, Soehendra et al. first treated Gastric Varices (GV) with tissue glue injection [10]. In 1988, Stiegmann GV et al. first applied EVL for esophageal varices [11]. So far, endoscopic diagnosis and treatment play an important role in gastroesophageal varices. Compared to the wide use of EVL, EIS becomes the second choice, and is mainly applicable for patients who are unsuitable for EVL or those that have unclear endoscopic visual field in emergency cases. In addition, re-bleeding after EVL is one of the indications for EIS. EIS still plays an important role in emergency hemostasis.
Routine EIS is generally performed through 1% ethoxysclerol and 5% sodium morrhuate. If this failed to control the bleeding, NBCA injection is an effective supplementary therapeutic means. In this study ECIS therapy was employed 31 times and the bleeding was successfully controlled in 30 cases (96.77%). As shown by X-ray and CT scan of chest/ abdomen after the procedure, lipiodol was found to be aggregated at the local injection site, and blood vessel casting formed in most cases (29 out of 31 cases, 93.54%). Although the hemostasis rate was 100% in balloon tamponade group, the bleeding volume increased and the average transfusion volume reached 11.7 u, these implicated severe liver dysfunction and slower recovery. ESCI therapy performed 31 times on 30 patients, in this study, showed no evidence of heterotopic embolism which was verified through X-ray and CT examination suggesting that this is an effective therapeutic option in treating EV.
Heterotopic embolism is one of the most serious complications of NBCA injection, and that is the reason for limiting its use in EV patient. However, in this study, there was no evident cough or other symptoms of heterotopic embolism which was verified by X-ray and CT examination following the procedure, possibly because ethoxysclerol and/or sodium morrhuate had been injected before NBCA injection. The former two common sclerosants could cause inflammation in the vascular endothelium, stimulate blood coagulation in local blood vessels and made the blood flow slow down. Thus, subsequent NBCA injection condensed easily at local injection site, so as to not only realize immediate hemostasis but also prevent heterotopic embolism.
After ESCI therapy, complications similar to those after ordinary EIS or NBCA therapy were observed. In this study, there was no serious heterotopic venous embolism or infection, but minor complications, such as fever which was controlled by anti-inflammatory drugs, were seen. The symptoms of discomfort in swallowing or dysphagia were also a common complication. Two cases had serious dysphagia caused by early glue extrusion due to the esophageal stenosis that was already present or formed after the ulceration. The glue mass that extruded early stayed at middle and lower sections of the esophagus to cause serious stenosis, drifted with food or water into esophageal cavity due to gravity so as to occasionally obstruct the esophagus completely through piston-like action. At this time, endoscopic re-examination and removal were performed to relieve the symptoms.
As observed during the follow-up in this study (endoscopy, X-ray and CT examination), the glue extrusion progressed in a certain fashion. In contrast to fundic varices, glue extrusion at esophagus started early from week 1~2, and completed mostly with flaky ulceration at glue extrusion site by the end of month 1. As shown by endoscopic examination in most patients, the glue extrusion progressed by week 2, and completed, possibly without glue residue or with only trace glue residue, (X-ray examination) 3 weeks after the procedure. CT or MRI examination revealed that a little lipiodol remained at the periesophageal wall. Such residue often lasted a relatively long time. However, after the tissue glue injection for fundic varix, the glue extrusion generally started from early week 2~3 to late stage of about 3~6 months after the procedure [12]. Such difference might result from the following fact: esophageal varix occurring at the superficial layer of mucosa whose blood supply distribution was sparser than that at the surface of fundic vein. With the embolism of blood vessel, blood and oxygen became deficient in the mucosa on the surface of esophageal blood vessel, so as to finally cause tissue necrosis and early adhesive extrusion.
Despite not being a routine endoscopic therapeutic method, ESCI for EV provides a new option of endoscopic therapy for massive EV bleeding. As verified by this study, ESCI was effective and could be extensively applied clinically. The limitations of the present study were: (1) This retrospective analysis had relatively small size of population; (2) Laboratory data such as hemoglobin, blood coagulation time and liver function before and after the procedure were not reported because no significant affection of the procedure on these parameters was found. Therefore, a multi center and randomized controlled study will be performed in the future study.
References
- D’Amico G, De Franchis R, Cooperative Study Group. Upper digestivebleeding in cirrhosis. Post-therapeutic outcome and prognostic indicators. Hepatology 2003; 38: 599-612.
- Sharara AI, Rockey DC. Gastroesophageal variceal hemorrhage. N Engl J Med 2001; 345: 669-681.
- Sarin SK, Jain AK, Jain M, Gupta R. A randomized controlled trial of cyanoacrylate versus alcohol injection in patients with isolated fundicvarices. Am J Gastroenterol 2002; 97: 1010-1015.
- Lo GH, Lai KH, Cheng JS, Chen MH, Chiang HT. A prospective, randomized trial of butyl cyanoacrylate injection versus band ligation in the management of bleeding gastric varices. Hepatology 2001; 33: 1060-1064.
- Sée A, Florent C, Lamy P, Lévy VG, Bouvry M. Cerebrovascular accidents after endoscopic obturation of esophageal varices with isobutyl-2-cyanoacrylate in 2 patients. Gastroenterol Clin Biol 1986; 10: 604-607.
- Bendtsen F, Krag A, Meller S. Treatment of acute variceal bleeding. Dig Liver Dis 2008; 40: 328-336.
- Nevens F, Rutgeerts P. Variceal band ligation in the management of bleedingoesophageal varices: an overview. Dig Liver Dis 2001; 33: 284-287.
- Cipolletta L, Zambelli A, Bianco MA, De Grazia F, Meucci C, Lupinacci G, Salerno R, Piscopo R, Marmo R, Orsini L, Rotondano G. Acrylate glue injection for acutely bleeding oesophageal varices: A prospective cohort study. Digest Liver Dis 2009; 41: 729-734.
- Seewald S, Sriram PV, Naga M, Fennerty MB, Boyer J, Oberti F. Cyanoacrylate Cyanoacrylate glue in gastric variceal bleeding. Endoscopy 2002; 34: 926-932.
- Soehendra N, Nam VC, Grimm H. Endoscop ic obliteration of large esophagogastric varices with bucrylate. Endoscopy 1986; 18: 25-26.
- Stiegmann GV, Cambre T, Sun JH. A new endoscopic elastic band ligating device. Gastrointest Endosc 1986; 32: 230.
- Wang YM, Cheng LF, Li N, Wu K, Zhai JS, Wang YW. Study of glue extrusion after endoscopic N-butyl-2-cyanoacrylate injection on gastric variceal bleeding. World J Gastroenterol 2009; 15: 4945-4951.