ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 15
The comparison of pneumatic and hydrostatic reposition with surveillance of ultrasound in the treatment of intussusception
Yushui Huai1*, Zhengyin Yin1 and Kai Zhou2
1Department of Ultrasound, the First Affiliated Hospital of Bengbu Medical College, Anhui, PR China
2Department of Paediatric Surgery, the First Affiliated Hospital of Bengbu Medical College, Anhui, PR China
- *Corresponding Author:
- Yushui Huai
Department of Ultrasound
The First Affiliated Hospital of Bengbu Medical College
Anhui, PR China
Accepted date: July 13, 2017
Objective: Intussusception is a common acute abdomen in infants. With the excellent sensitivity and specificity, ultrasonography has become the preferred imaging method for diagnosis of intussusception. Our study aimed to investigate the efficacy of pneumatic and hydrostatic reposition with surveillance of ultrasound in the treatment of intussusception.
Methods: A total of 201 children and infants with intussusception diagnosed by ultrasonography were collected from June 2011 to January 2016 in our hospital. The patients were divided into two groups for different treatments (pneumatic or hydrostatic reposition). The successful rates of two methods were compared. In addition, the factors affect the treatment outcomes were also identified.
Results: The success rate of pneumatic reposition was 91.6% and the success rate of hydrostatic reposition was 86.7%. The success of treatment was negatively correlated with the course of disease and the weight of the patients. In addition, the patients with lesion sites in the upper part of the abdomen usually showed better treatment outcomes compared with the patients with lesion sites in other parts.
Conclusion: Ultrasonography, which can avoid radioactive examination, is safe and effective in the diagnosis and treatment of paediatric intussusception. Pneumatic and hydrostatic reposition both showed satisfactory success rate but pneumatic reposition was better.
Keywords
Ultrasonography, Intussusception, Pneumatic reposition, Hydrostatic reposition
Introduction
Intussusception is medical condition that one segment of the bowel folds into an adjacent segment [1]. Although a variety of factors including anatomical factors, infections and altered motility were shown to be correlated with the onset and development of intussusception, the mechanism of this disease is still unknown [1-3]. The death caused by intussusception is rare with a fatality rate below 1% [4]. However, the clinical symptoms caused by intussusception, including periodic abdominal pain, vomiting, nausea or even rectal bleeding and dyspnoea, can seriously affect the patient’s health [5]. Intussusception is mostly observed in children and has been shown to be the most common acute abdominal disease in children below 2 y old and the second most important cause of intestinal obstruction in the children with pyloric stenosis [6]. Previous studies have shown that the timely management of the intussusception can usually lead to satisfactory treatment outcomes, while delayed treatment may cause bowel perforation and infarction or even death [7]. Therefore, the early diagnosis is the key for the treatment of intussusception [7,8].
Accurate imaging plays an essential role in the diagnosis of intussusception [9]. Abdominal radiography is usually the first diagnostic test for the patients with abdominal pain. However, it has been proved that the sensitivity and specificity of x-rays, which ranged from 36%-90% and 45%-90%, respectively, were usually not enough for the diagnosis of intussusception, and more than one-fifth of patients with proven intussusception showed normal X-ray results [10,11]. A recent clinical study also showed that abdominal radiography was not necessary for the diagnosis of children with intussusception [12]. Compared with abdominal radiography, the higher sensitivity and specificity of ultrasound make it the ideal choice for diagnosing intussusception [13]. In addition, radioactive examination was avoided in the application of ultrasound, which in turn significantly increased the safety of the diagnosis [13]. Clinical practice has proved that the success rate of ultrasound guided hydrostatic reposition reached 90% in the treatment of intussusception in children between 3 months and 2 y old [14]. Recently, ultrasound combined with pneumatic reposition was also reported to be safe and effective in the treatment of children with intussusception, and the success rate was reported to be higher than 80% [15,16]. So, it will be interesting to compare the efficacy of those two treatments to find the better way for the diagnosis of treatment of intussusception.
In our study, the children and infants with intussusception were subjected to pneumatic reposition or hydrostatic reposition with surveillance of ultrasound. The success rates of those two methods were compared and the factors that determine the success of the treatment were also discussed.
Materials and Methods
General information
201 cases of children with intussusception were collected from June 2011 to January 2016 in the First Affiliated Hospital of our University. Surgical treatment is performed for 19 cases of the patients due to intestinal inflammation, intestinal perforation, moderate abdominal pain and other contra indications. The other patients (182 cases) received pneumatic or hydrostatic reposition. Among the patients, there were 102 boys and 80 girls, and the age ranged from 2 months to 7 y with an average aged of 25.6 months. The main clinical manifestations include vomiting, recurrent abdominal pain or irritable crying, jam-like stool and abdominal mass. All the patients or their family members signed the informed consent and this study was proved by the Ethics Committee of our Hospital.
Ultrasonography
GE Logiq-7 color Doppler ultrasound system (GE, USA) was for ultrasonic examination. Intrarectal application of midazolam solution (0.4 mg/kg) was performed for the children with irritable crying before examination. The children were fixed in supine position. The abdomen was scanned with probe frequency of 2-5 MHz and appropriate probe pressure. The probe was moved slowly to check the presence of abnormal mass, intestinal expansion, peristalsis hyperthyroidism, peritoneal effusion etc. If the abnormal parts were found, linear high-frequency probe (6-10.0 MHz) was used to scan the vertical, horizontal and oblique sections of abdomen with a focus on the internal structure of the mass. The transverse section of the lesion site of intussusception showed concentric circle, and the longitudinal section was “sleeve-like”. Intestinal cavity gas can show pseudo-kidney sign. Longitudinal section was used to measure the length of the nesting section.
Pneumatic reposition with surveillance of ultrasound
The patients were fixed in supine position with help from their parents if necessary. Foley tube was inserted into the anus. The buttocks were tightened with tape or hands to prevent the dropping of anal canal and gas leakage. Inflation pressure was adjusted according to the course of disease and the length of the lesion area. The treatment was started with low pressure (7 kPa) for 20 s, then the pressure was gradually increased (0.5 kPa for each time) to reach the maximum gas pressure of 16 kPa. It took 3 min to finish the whole procedure, and the whole procedure was repeated several times until the reposition was achieved. The reposition was achieved with the entrance of large amount of air into ileum and the disappearance of mass. Gas pressure was recorded.
Hydrostatic reposition with surveillance of ultrasound
The patients were fixed in supine position with help from their parents if necessary. Foley tube was inserted into the anus. The buttocks were tightened with tape or hands to prevent the dropping of anal canal and gas leakage. Physical saline was used as an enema. Water pressure was determined according to the age of the patients. The maximum water pressure for the patients below 6 months old was 90 mmHg (1 mmHg=0.1333 kPa), and the maximum water pressure was 130 mmHg for the patients above 6 months old. The temperature of the physiological saline was maintained at 37°C, and the enema administration unit was placed at a height of 1 to 1.2 m from the treatment bed. The disappearance of “concentric circles” showed by ultrasound and the disappearance of resistance in colon or ileocecal indicated the success of reposition. The second treatment was performed if failed in the first time, and the treatment could be repeated up to 4 times.
All patients who received pneumatic or hydrostatic reposition were monitored during their hospitalization. Ultrasonography was performed again between 12-24 h after treatment to avoid early recurrence of intussusception.
Statistical analysis
All the monitoring data were analyzed using GraphPad Prism 5.0 statistical software. Chi-square (Fisher’s exact) test or Student’s t-test was used for univariate analysis. All analytical data were expressed as mean ± SD (mean ± SD), and p<0.05 was statistically significant.
Results
The comparison of the basic information of the patients in two groups
The basic information of patient, including gender, age, weight course of disease, temperature etc., was compared between two groups. As shown in Table 1, no significant difference was found in the basic information between groups, indication, the patients involved in those two groups can be used as the subjects for comparison study.
| Characteristics | Pneumatic reduction (n=107) | Hydrostatic reduction (n=75) | p value |
|---|---|---|---|
| Gender | 0.087 | ||
| Male | 73 | 41 | |
| Female | 34 | 34 | |
| Age (month) | 24 | 25.5 | 0.642 |
| Weight (kg) | 10.7 | 12.5 | 0.578 |
| Weight ≤ 13 kg | 66 | 45 | |
| Weight>13 kg | 41 | 30 | |
| Duration (h) | 25.2 | 24.4 | 0.804 |
| Duration ≤ 48 h | 81 | 50 | |
| Duration >48 h | 26 | 25 | |
| Vomiting | 94 | 59 | 0.104 |
| Abdominal pain | 81 | 47 | 0.07 |
| Bloody stool | 78 | 46 | 0.1 |
| Location | 0.284 | ||
| Lower side | 48 | 27 | |
| Upper side | 59 | 48 | |
| Temperature (°C) | 37.8 | 37.6 | 0.538 |
| Temperature ≤ 37.8°C | 68 | 44 | |
| Temperature>37.8°C | 39 | 31 |
Table 1: The comparison of the basic information of the patients in two groups.
Treatment outcomes of pneumatic reposition with surveillance of ultrasound
A total of 107 patients, including 73 boys and 34 girls, received pneumatic reposition. As shown in Table 2, the success of reposition was observed in 98 cases, accounting for 91.6 % of all the patients. Our data also showed that the average weight and temperature of patients in success group was significantly lower than those of the patients in failure group (10.2 vs 15.6, p=0.002; 37.5 vs 38.6, p=0.011). The course of disease in success group was significantly shorter than in failure group (22 vs. 60, p<0.001). In addition, the patients with lesion sites in the upper part of the abdominal cavity showed significantly better outcomes than the ones with lesion sites in other parts (p=0.01). Our data suggested that the success of pneumatic reposition was negatively correlated with the weight and temperature of the patients and course of disease. The position of lesion sites also determined the treatment outcomes.
| Characteristics | Success (n=98) | Failure (n=9) | p value |
|---|---|---|---|
| Gender | |||
| Male | 67 | 6 | 0.917 |
| Female | 31 | 3 | |
| Age (month) | 23.8 | 26.6 | 0.709 |
| Weight (kg) | 10.2 | 15.6 | 0.002 |
| Weight ≤ 13 kg | 65 | 1 | |
| Weight>13 kg | 33 | 8 | |
| Duration (h) | 22 | 60 | <0.001 |
| Duration ≤ 48 h | 79 | 2 | |
| Duration >48 h | 19 | 7 | |
| Vomiting | 86 | 8 | 0.921 |
| Abdominal pain | 75 | 6 | 0.6848 |
| Bloody stool | 70 | 8 | 0.259 |
| Location | 0.01 | ||
| Lower side | 40 | 8 | |
| Upper side | 58 | 1 | |
| Temperature (°C) | 37.5 | 38.6 | 0.011 |
| Temperature ≤ 37.8°C | 66 | 2 | |
| Temperature>37.8°C | 32 | 7 |
Table 2: Treatment outcomes of pneumatic reposition with surveillance of ultrasound.
Treatment outcomes of hydrostatic reposition with surveillance of ultrasound
There were 75 patients, including 40 boys and 35 girls, received hydrostatic reposition. As can be seen in Table 3, the success of reposition was observed in 65 cases, accounting for 86.7 % of all the patients. Our data also showed that the average weight and temperature of patients in success group was significantly lower than that of the patients in failure group (11.8 vs. 16.9, p=0.012). The course of disease in success group was significantly shorter than in failure group (18 vs. 66, p=0.013). In addition, the patients with lesion sites in the upper part of the abdominal cavity showed significantly better outcomes than the ones with lesion sites in other parts (p=0.003). Our data suggested that the success of hydrostatic reposition was negatively correlated with the weight of the patients and course of disease. The position of lesion sites also determined the treatment outcomes.
| Characteristics | Success (n=65) | Failure (n=10) | p value |
|---|---|---|---|
| Gender | 0.716 | ||
| Male | 35 | 6 | |
| Female | 30 | 4 | |
| Age (month) | 25.2 | 27.1 | 0.792 |
| Weight (kg) | 11.8 | 16.9 | 0.012 |
| Weight ≤ 13 kg | 43 | 2 | |
| Weight>13 kg | 22 | 8 | |
| Duration (h) | 18 | 66 | 0.013 |
| Duration ≤ 48 h | 47 | 3 | |
| Duration>48 h | 18 | 7 | |
| Vomiting | 52 | 7 | 0.436 |
| Abdominal pain | 38 | 9 | 0.08 |
| Bloody stool | 40 | 6 | 0.926 |
| Location | 0.003 | ||
| Lower side | 19 | 8 | |
| Upper side | 46 | 2 | |
| Temperature (°C) | 37.2 | 37.8 | 0.927 |
| Temperature ≤ 37.8°C | 38 | 6 | |
| Temperature>37.8°C | 27 | 4 |
Table 3: Treatment outcomes of hydrostatic reposition with surveillance of ultrasound.
Comparison of the success rates of the two treatments
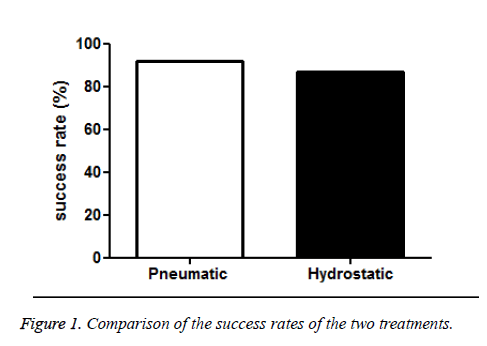
Pneumatic reposition and hydrostatic reposition with surveillance of ultrasound are the two most commonly used methods in the treatment of intussusception. Our data showed that the success rate of pneumatic reposition was 91.59%, and the success rate was 86.67% for hydrostatic reposition. Both the two treatments achieved satisfactory efficacy. Although the success rate of pneumatic reposition was slightly higher than that of hydrostatic reposition, no significant differences were found between them. Our data suggested that both the methods can be used in the treatment of intussusception (Figure 1).
Discussion
Intussusception is the most common cause of intestinal obstruction in infants and children with the incidence higher in male than in female [17]. Consistent with previous studies, there were 102 boys and 80 girls diagnosed with intussusception in our study, the male/female ratio are 1.275:1. The classic clinical symptoms of intussusception include palpable abdominal, red currant jelly stools and abdominal pain. However, clinical studies have shown that the classic symptoms can only be observed in one-third cases of intussusception [18]. In our study, some patients showed the symptoms of vomiting and irritable crying. Therefore, the clinical judgement is only enough for the diagnosis of intussusception, and imaging should be applied. Radiography, Computed Tomography (CT) and ultrasound are the three imaging methods widely used in the detection of intussusception [19]. Radiography was used widely in the diagnosis of intussusception. However, radiography was not recommended to be used in routine workup of suspected intussusception now due to the unacceptably low specificity and sensitivity was well as the safety issue caused by the using of radiation examination [10,19]. CT can be used for equivocal cases. However, the routine use of CT in the detection of intussusception was also limited by the high radiation exposure to the patients [17,20]. Ultrasound, in which the use of radioactive material was avoided, is a relatively safe imaging technique compared with radiography and CT [12,19]. In addition, ultrasound can be highly specific and sensitive in non-destructive testing [19]. All the characteristics of ultrasound make it the most promising imaging methods in the diagnosis of intussusception.
Ultrasound combined with hydrostatic reposition has been proved to be an effective way in the diagnosis and treatment of intussusception. With the real-time ultrasound, the whole procedure of hydrostatic reposition can be monitored to increase the safety of operations, which in turn increased the success rate of treatment [13]. A recent study carried out by Ahmad et al. has shown that 70 out of 78 patients with intussusception showed satisfactory outcomes after the treatment of hydrostatic reposition with the guidance of ultrasound and the successful rate reached to 90% [21].
Another study focused on the application of ultrasound-guided hydrostatic reposition also shown a success rate of about 90% in the diagnosis and the treatment of the intussusception children patients with an age of 3 months to 2 y [13]. In our study, 75 patients received hydrostatic reposition under the guidance of ultrasound and 65 cases showed complete reposition, accounting for 86.7% of all the patients, which is close to the success rate that has been reported previously [13,21]. The combination of pneumatic reposition and ultrasound is another widely used method [14]. A clinical study performed by Hasan et al. has found that the success rate of the pneumatic reposition with the guidance of ultrasound in the treatment of intussusception was 84.4% [20]. In our study, 107 patients underwent pneumatic reposition with surveillance of ultrasound, and complete reposition was found in 98 patients, accounting for 91.6% of all the cases, which is higher than the success rate reported in previous studies [18]. We also compared the success rate of the two methods, no significant differences were found, indicating that both two methods are effective and safe in the diagnosis and treatment of the children with intussusception.
The identification of factors related to the success of treatment is important for the prediction of treatment outcomes. A previous study has shown that operative time of the treatment and length of postoperative hospital stay were correlated with the treatment outcomes, and age was not correlated with the success rate [22]. In our study, the treatment outcomes of both the two treatments were found to be negatively correlated with the weight of the patients and course of disease. In addition, we also found that the position of lesion sites also determined the treatment outcomes. Those findings will helpful for the physicians to choose the proper individual treatment strategy.
In conclusion, Pneumatic reposition and hydrostatic reposition with surveillance of ultrasound both reached the success rate higher than 86.67%. Although the success rate of pneumatic reposition was slightly higher than that of hydrostatic reposition, no significant differences were found between them. The treatment outcomes were negatively correlated with the weight of the patients and course of disease. The position of lesion sites also determined the success rate. Reposition with surveillance of ultrasound is safe and effective in the treatment of intussusception, and should be popularized.
References
- Marsicovetere P, Ivatury SJ, White B. Intestinal intussusception: etiology, diagnosis, and treatment. Clin Colon Rectal Surg 2017; 30: 30-39.
- Paul DO, Adam R. Celiac disease presenting as intussusception from giardia lamblia. World Congress Pediatr Gastroenterol Hepatol Nutr 2016.
- Kvasha A, Khalifa M, Biswas S. Unlimited-length proctocolectomy utilizing sequential intussusception and pull-through novel clean endolumenal. Surg Innovation 2016; 23: 456-462.
- Rha B, Tate JE, Weintraub E. Intussusception following rotavirus vaccination: an updated review of the available evidence. Expert Rev Vaccines 2014; 13: 1339-1348.
- Kumar Mr L, Mukhtar H, Vaidya J. Benign causes of adult intussusception. World J Colorectal Surg 2014; 4: 3.
- Walker WA. Paediatric gastrointestinal disease: pathophysiology, diagnosis, management. PMPH-USA 2004.
- Applegate KE. Intussusception in children: evidence-based diagnosis and treatment. Paediatr Radiol 2009; 39: 140.
- Lehnert T, Sorge I, Till H. Intussusception in children-clinical presentation, diagnosis and management. Int J Colorectal Dis 2009; 24: 1187-1192.
- Somma F, Faggian A, Serra N. Bowel intussusceptions in adults: the role of imaging. La Radiologia Medica 2015; 120: 105-117.
- Robson N, Beasley S. Role of plain abdominal radiography in the initial investigation of suspected intussusception. J Paediatr Child Health 2014; 50: 251-252.
- Kodikara H, Lynch A, Morreau P. Ten-year review of intussusception at Starship Hospital: 1998-2007. New Zealand Med J 2010; 123.
- Tareen F, Mc Laughlin D, Cianci F. Abdominal radiography is not necessary in children with intussusception. Pediatr Surg Int 2016; 32: 89-92.
- Gfroerer S, Fiegel H, Rolle U. Ultrasound-guided reduction of intussusception: a safe and effective method performed by pediatric surgeons. Pediatr Surg Int 2016; 32: 679-682.
- Hossain MS, Huq MAU, Hannan J. Role of ultrasound-guided hydrostatic reduction of intussusception in children with early presentation. J Paediatr Surg 2015; 3: 61-64.
- Venkatesh SKK, Raghavan BP, Valiyakandoth G. Safety and efficacy of ultrasound guided pneumatic reduction of intussusception in children. Anz J Surg 2016; 86: 106.
- Hasan OB, Farees SN, Ibrahim M. Ultrasound guided pneumatic reduction of intussusception in children-a case series. Int J Recent Sci Res 2015.
- Mehendale S, Kumar CPG, Venkatasubramanian S. Intussusception in children aged less than five years. Indian J Pediatr 2016; 83: 1087-1092.
- Williams H. Imaging and intussusception. Archiv Dis Childhood Edu Pract 2008; 93: 30-36.
- Carroll AG, Kavanagh RG, Leidhin CN. Comparative effectiveness of imaging modalities for the diagnosis and treatment of intussusception: a critically appraised topic. Acad Radiol 2017.
- Amr MA, Polites SF, Alzghari M. Intussusception in adults and the role of evolving computed tomography technology. Am J Surg 2015; 209: 580-583.
- Ahmad MM, Wani MD, Dar HM. An experience of ultrasound-guided hydrostatic reduction of intussusception at a tertiary care centre. South Afr J Surg 2016; 54: 10-13.
- Wei CH, Fu YW, Wang NL. Laparoscopy versus open surgery for idiopathic intussusception in children. Surg Endosc 2015; 29: 668-672.