ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 3
Single-stage approach of posterior debridement, allograft and internal fixation in management of lumbosacral tuberculosis
Jiawen Wu1, Juanjuan Wang2, Ming Kang3, Hao Wang1, Jingbiao Chen1, Yuliang Huang3, Qian Yue1, Dejia Wang1 and Honghua Cai1*
1Department of Spine Surgery, Huizhou Municipal Central Hospital, Huizhou, Guangdong, PR China
2Department of Ophthalmology, Huizhou Municipal Central Hospital, Huizhou, Guangdong, PR China
3Department of Orthopaedics, Huizhou Municipal Central Hospital, Huizhou, Guangdong, PR China
- *Corresponding Author:
- Honghua Cai
Department of Spine Surgery
Huizhou Municipal Central Hospital, PR China
Accepted date: September 13, 2016
Background: To evaluate clinical efficacy and safety of posterior debridement, allograft and internal instrumental fixation in the management of lumbosacral tuberculosis.
Methods: Fifteen patients diagnosed with lumbosacral tuberculosis were recruited in this study. All participants were scheduled to undergo posterior debridement, bone fusion, lumbar and sacral pedicle screw fixation or screw fixation in the bilateral iliac alar.
Results: The mean operation time was (170.5 ± 24.2) min. The average intraoperative haemorrhage volume was (980.3 ± 168.6) ml. No dural or the great artery injury was observed. No sinus tract formation was observed. All patients were followed up for 12 to 39 months. Bone fusion and internal fixation were successfully performed in 15 cases. All patients were completely recovered and no recurrence of tuberculosis was reported. Before surgery, 11 patients were diagnosed with decreased lower limb myodynamia of varying degree. During the last follow-up, the toe extension myodynamia was restored from grade III to grade IV in one case, and recovered to grade V in 10 patients. Postoperatively, 11 patients presented with lower leg or foot dermatalgia and hypopselaphesia. During subsequent follow-up, 2 patients were partially healed and 9 were fully recovered. Among 9 patients with knee or ankle hyporeflexia before surgery, 2 cases were partially treated and 7 were successfully healed. Prior to operation, 6 cases were positive for Lasegue's test and returned to normal after surgery.
Conclusions: Based upon conventional anti-tuberculosis medication, one stage posterior debridement, allograft and internal instrumental fixation is an efficacious and safe intervention for lumbosacral tuberculosis.
Keywords
Tuberculosis, Lumbosacral junction, Posterior route, Clinical efficacy, Safety.
Introduction
Tuberculosis of the lumbosacral junction is rare, accounting for approximately 3% of vertebral column tuberculosis [1,2]. Common surgical interventions of spinal tuberculosis include surgical debridement, bone fusion and grafting, etc. The goals of surgical treatment of spinal tuberculosis are to accelerate nerve functional recovery, prevent spinal deformity and maintain spinal stability. Early stage lumbosacral tuberculosis has been successfully handled with chemotherapy. For patients with advanced stage tuberculosis affecting extensive lumbosacral region, loss of lumbar lordosis and lumbosacral biomechanics should be scheduled to undergo surgery [3].
The management of tuberculosis involved in the lumbar spine and lumbosacral junction is entirely different when treating the disease of either of these regions individually. The goals and principles of clinical treatment of extensive disease involving both the lumbar spine and the lumbosacral junction have been rarely described in the literatures [4]. The instrumentation at the lumbosacral junction is technically demanding considering complicated topical anatomy, unique biomechanics characteristics and the difficulty in internal fixation adjacent to the affected bones.
In this investigation, 15 patients diagnosed with lumbosacral tuberculosis were scheduled to receive posterior debridement, bone fusion, lumbar and sacral pedicle screw fixation or lateral internal fixation. Favourable clinical outcomes were obtained.
Materials and Methods
Baseline data
Among 15 participants, 6 were male and 9 female, aged 35 to 67 years with a mean age of (48.6 ± 12.3) years. Seven cases had a medical history of pulmonary tuberculosis. Patients presented with varying degree of low heat, night sweat and toxic symptoms induced by tuberculosis.
Fourteen patients were admitted due to lumbar and back pain, and one due to abdominal pain. Eleven patients reported decreased lower limb myodynamia including 4 with grade III toe extension myodynamia and 7 with grade IV. Nine cases had decreased knee and ankle reflex. Six patients had positive outcomes for Lasegue’s test.
Imaging diagnosis
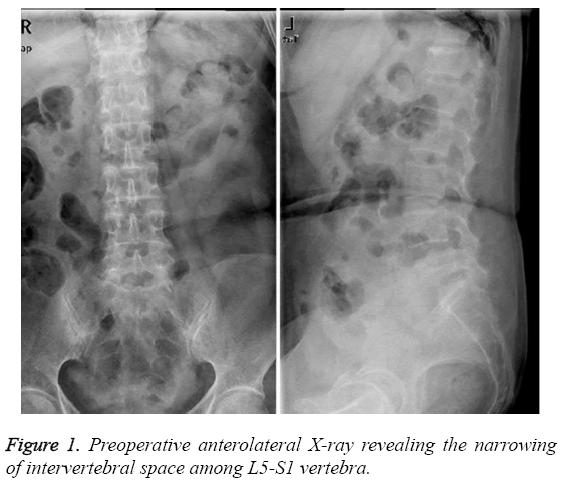
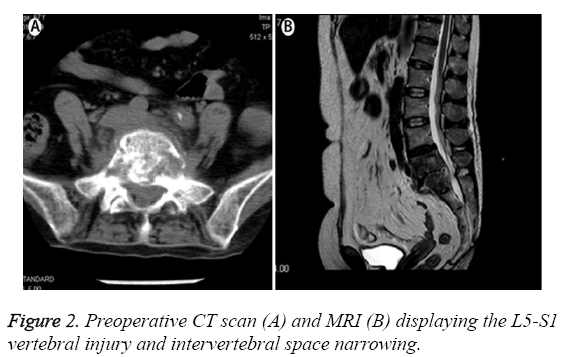
Preoperative X-ray (Figure 1), CT scan (Figure 2A) and MRI (Figure 2B) examination revealed that L4-S1 vertebral involvement in 5 patients, L5-S1 in 8 and L5-S2 in 2 cases. Imaging findings demonstrated the signs of intervertebral space narrowing in all cases. Bone destruction and sequestration were observed in the diseased vertebrae. Cold abscess formation was noted in the unilateral or bilateral psoas muscle.
Preoperative preparation
Prior to operation, all patients underwent X-ray, CT scan and MRI examination of the lumbosacral region. Laboratory tests were performed. Fasting patients were administered with 0.3 g isoniazid, 0.45 g rifampicin and 0.75 g pyrazinamide in the morning once daily. They were injected with 0.75 g streptomycin via intramuscular route once daily. Nutrition supporting therapy was delivered simultaneously. Four patients without neurological symptoms, they underwent surgery after 4-week anti-tuberculosis therapy and erythrocyte sedimentation rate declined below 40 mm/h. The remaining 11 cases presenting with neurological symptoms received antituberculosis treatment for 6 to 10 d. Following the tuberculosis-induced toxic symptoms were mitigated, they were immediately scheduled to undergo the operation.
Surgical intervention
The patients received endotracheal intubation under general anaesthesia in a prone position. The median incision was made, the supraspinal ligament was preserved and the diseased vertebra and two surrounding vertebrae were exposed. Decompression management was delivered at the side with extensive abscess, and intact vertebral lamina, zygapophysial joints and joint capsule were retained at the contralateral side. The pedicle screw was inserted. The sacral screw was replaced and inserted laterally in 7 patients who developed vertebral injury induced by pedicle screw fixation. The nondecompression side was first fixed by using a titanium rod of a suitable length. After proper internal fixation, the radian between the lumbar and sacrum almost returned to normal. Subsequently, the zygapophysial joints and a slight portion of vertebral lamina at the decompression side of the diseased vertebra were eliminated, exposing the abscess and vertebral gap. The nerve root was carefully protected. The abscess fluid was discharged. The necrotic and granulation tissues were thoroughly removed until the sign of errhysis was documented. The autologous iliac bone was implanted in the vertebra or the vertebral defect. Then, the titanium rod was fixed at the decompression side. Normal saline irrigation was performed on the wound surface. Then, 0.3 g isoniazid and 1 g streptomycin were placed in the wound site. A drainage tube was placed at the decompression side and the incisions were sutured layerby- layer.
Postoperative management
Conventional antibiotics therapy was delivered via intravenous drip for 48 h. Liver protection therapy and nutritional support treatment were strengthened. Administration of albumin was delivered when necessary. Postoperative nursing care should be enhanced to prevent the incidence of deep vein thrombosis and other postoperative complications. After the surgery, fasting patients were administered with 0.3 g isoniazid, 0.45 g rifampicin and 0.75 g pyrazinamide in the morning once daily. They were injected with 0.75 g streptomycin via intramuscular route once daily. The drainage tube was removed when the drainage volume declined below 50 ml/d. On a regular basis, all patients were required to receive routine blood test, liver and kidney function test, erythrocyte sedimentation rate test and detection of C-reactive protein levels with a time interval of 5 to 7 d. At approximately 1 week after surgery, the patients remained physically stable and were advised to do physical activities using brace protection for 6 to 8 months. X-ray imaging test was performed to evaluate the status of bone fusion once every 3 months.
According to individual situation, a triad medication regime consisting of 0.3 g isoniazid, 0.45 g rifampicin and 0.75 g pyrazinamide was further delivered for 12 to 18 months until the tuberculosis was fully treated.
Results
The operation time ranged from 145 to 235 min with a mean value of (170.5 ± 24.2) min. Intraoperative haemorrhage volume was measured from 800 to 1300 ml with a mean quantity of (980.3 ± 168.6) ml. All patients presented with neither dural nor the great artery injuries. No sinus tract was formed. For male patients, no symptoms of retrograde ejaculation occurred.
Pathological diagnosis results confirmed the incidence of chronic inflammatory changes accompanied by sequestration. Three patients showed transient aggravation of nerve symptoms and were restored after administration of dehydration and trophic nerve therapy for 4 to 15 d. It may be resulted from intraoperative traction of the nerve root. All participants were subject to 12-39 month follow-up.
Erythrocyte sedimentation rate and C-reactive protein levels returned to normal range after anti-tuberculosis treatment for 2 to 6 months. The bone fusion rate achieved up to 100%. No signs of loosening internal fixation were observed. According to the criteria of bone tuberculosis healing [4], all patients were completely recovered. No indications of tuberculosis recurrence were documented.
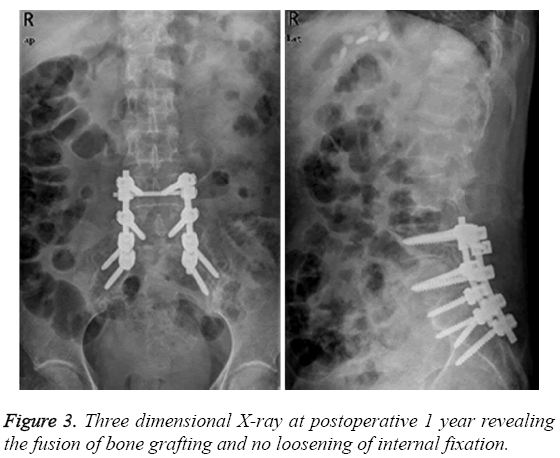
Before surgery, 11 patients were diagnosed with decreased lower limb myodynamia of varying degree. During the final follow-up, the toe extension myodynamia was restored from grade III to grade IV in one case, and recovered to grade V in 10. Preoperatively, 11 patients presented with lower leg or foot dermatalgia and hypopselaphesia. During subsequent followup, 2 patients were partially healed and 9 fully recovered. Among 9 patients with knee or ankle hyporeflexia before surgery, 2 cases were partially treated and 7 were successfully healed. Prior to operation, 6 cases were positive for Lasegue's test and returned to normal after surgery. Three dimensional Xray at postoperative 1 year indicated the fusion of bone grafting and no loosening of internal fixation, as illustrated in Figure 3.
Discussion
Clinical treatment of tuberculosis of the lumbosacral junction remains a controversial and challenging task for surgeons. Few studies have been performed focusing on the surgical intervention in advanced lumbosacral junction tuberculosis. Previous studies [5-7] have reported that patients receiving non-surgical treatment developed a high incidence of kyphosis associated with trunk shortening. Advanced-stage tuberculosis with extensive destruction of the lumbosacral spine leads tothe occurrence of kyphosis or hypolordosis, accompanied with back pain and difficulties during childbirth. Due to complicated local anatomy, the unique biomechanics, and difficult fixation in the surrounding diseased bone, instrumentation at the lumbosacral junction is highly technically demanding. In tuberculosis with extensive injuries of the lumbar spine and lumbosacral junction requiring long fusion to the sacrum, the loss of sacral bone for implant anchoring changes the fixation options suitable for these patients.
In this investigation, 15 patients diagnosed with lumbosacral tuberculosis were scheduled to undergo posterior debridement, bone fusion, lumbar and sacral pedicle screw fixation or lateral internal fixation. Lumbosacral tuberculosis is adjacent to the rectum, iliac vessels and ureter, where the abscess is likely to form. Hence, thorough removal of the diseased tissues is a highly demanding task. In addition, inflammation is involved with surrounding nerve vessels, which enhances the tissue fragility, increases the risk of vascular injury and elevates the incidence of retrograde ejaculation after sympathetic nerve damages. Therefore, in our experience, we were not expected to thoroughly eliminate the granulation tissues in front of and bilateral to the vertebra to avert the incidence of vertebral injury. The abscess fluid was discharged as possible. Meantime, the necrotic tissues between the vertebra and invading into the vertebral canal should be fully eliminated, which could enhance the bone fusion rate and accelerate nerve functional recovery. In this study, neither the great artery injury nor retrograde ejaculation occurred before, during and after the procedures. All patients presented with bone fusion. The timing of surgical intervention is of clinical significance, which should be initiated based upon the anti-tuberculosis therapy and after the tuberculosis-induced toxic symptoms are mitigated. Otherwise, the surgery probably leads to the systemic dissemination of the tuberculosis and further aggravates the severity of diseases.
The goals of conventional treatment of lumbosacral tuberculosis are to correct and prevent a lumbar kyphosis, decompress the neural elements, restore or preserve a normal lumbosacral angle, and maintain the vertebral height and global spinal stability. Due to the complex lumbosacral anatomical structure, posterior surgery has been widely accepted as an ideal surgical approach, which can thoroughly eliminate the lesions, proper vertebral canal decompression and effectively support the bone graft [8-10]. Anterior debridement and fusion with a strut graft can prevent and lessen a kyphosis, but there is a high incidence of graft-related problems, such as high incidence of the great artery injury, limited correction angle, difficulty in internal fixation and slow rehabilitation. Another common option is anterior debridement, bone grafting combined with posterior internal fixation, which not only incorporates the advantages of anterior surgery, but also supports the spine using three columns. Application of this approach can reconstruct the spinal stability, decrease the incidence of bone graft slippage and collapse, and enhance the bone fusion rate [11,12]. In addition, anterior combined with posterior approach requires long operation time and yields severe surgical injury, which is not applicable to the elderly patients diagnosed with lumbosacral tuberculosis.
In this investigation, posterior debridement, bone grafting combined with internal fixation is not one of the conventional options for treatment of lumbosacral tuberculosis. However, it has multiple advantages of small surgical trauma, short operation time and three column supporting force, etc. It is suitable for patients with slight vertebral collapse, mild lumbar kyphosis, slight abscess surrounding the vertebra, lesions located between two vertebrae or at the posterior margin of the vertebra [13,14]. Nevertheless, the scope of lesion elimination is constrained, especially the diseased tissues in front of or on the contralateral side of the diseased vertebra. It is not applicable to those with extensive destruction of the spine and lumbosacral junction. Therefore, prior to the formal surgery, those with severe and extensive involvement of lumbosacral tuberculosis were excluded from the subsequent surgical procedures.
Our experience obtained from this clinical trial reveals that similar to other types of tuberculosis; anti-tuberculosis medication therapy remains the fundamental treatment for lumbosacral tuberculosis. It is not required to eliminate all the diseased bone within the vertebra, whereas the abscess fluid outside the vertebra should be thoroughly discharged and completely irrigated using normal saline solution. Another advantage of posterior approach is that it merely destroys unilateral articular process and vertebral lamina, but retains the joint capsule of the adjacent articular process and exerts no influences upon the spinal stability. In this investigation, all patients had successful bone fusion, no incidence of grafting slippage or kyphosis.
The principles of our screw use in this study are that the screws can be utilized for patients without vertebral pedicle injuries based upon preoperative CT or MRI imaging. At least, two disease-free vertebrae upper and lower the diseased vertebra should be fixed using a screw. For those with vertebral pedicle damages, a biomechanically stable fixation was achieved with screws in the disease-free sacral along with additional screws in the iliac alar bilaterally. In this study, 7 patients with vertebral pedicle injury but no iliac alar damages were treated with screw fixation in the iliac alar bilaterally. During subsequent follow-up, no screw slippage occurred and successful bone fusion was obtained in all 7 cases.
Conclusion
Taken together, posterior debridement, bone grafting and fusion combined with internal fixation is an efficacious and safe surgical procedure for lumbosacral tuberculosis. For patients with sacral pedicle and vertebral injuries but intact iliac alar, screw fixation in the iliac alar bilaterally is another favourable option.
Disclosure
The authors declare that there is no conflict of interest regarding the publication of this manuscript.
References
- Tuli SM. General principles of osteoarticulartuberculosis. ClinOrthopRelat Res 2002; 398:11.
- Wang XB, Li J, Lu GH. Single stage posterior instrumentation and anterior debridement for active tuberculosis of the thoracic and lumbar spine with kyphotic deformity. J IntOrthop 2012; 36:373-380.
- Ledbetter LN, Salzman KL, Sanders RK. Spinal neuroarthropathy: Pathophysiology, clinical and imaging features, and differential diagnosis. J Radiographics 2016; 36:783-799.
- Wang YX, Zhang HQ, Liao W. One-stage posterior focus debridement, interbody graft using titanium mesh cages, posterior instrumentation and fusion in the surgical treatment of lumbo-sacral spinal tuberculosis in the aged. J IntOrthop2016; 40:1117-1124.
- Jiang T, Zhao J, He M. Outcomes and treatment of lumbosacral spinal tuberculosis: A retrospective study of 53 patients. PLoS One 2015;10:e0130185.
- Zeng H, Wang X, Pang X. Posterior only versus combined posterior and anterior approaches in surgical management of lumbosacral tuberculosis with paraspinal abscess in adults.Eur J Trauma EmergSurg 2014; 40:607-616.
- Adeolu AA, Komolafe EO. Outcome of a posterior spinal fusion technique using spinous process wire and vertical strut. Ann Afr Med 2014; 13:30-34.
- Jin W, Wang Q, Wang Z. Complete debridement for treatment of thoracolumbar spinal tuberculosis: a clinical curative effect observation. Spine J 2014; 14:964-970.
- Mahapatra S, Sahoo M, Sethi G. Comment on Wang: Single-stage posterior instrumentation and anterior debridement for active tuberculosis of the thoracic and lumbar spine with kyphotic deformity. IntOrthop 2013; 37: 1623-1627.
- Zhang HQ, Li JS, Guo CF. Two-stage surgical management using posterior instrumentation, anterior debridement and allografting for tuberculosis of the lower lumbar spine in children of elementary school age-minimum 3-year follow-up of 14 patients. Arch Orthop Trauma Surg 2012; 132: 1273-1279.
- Sundararaj GD, Behera S, Ravi V. Role of posterior stabilization in the management of tuberculosis of the dorsal and lumbar spine. J Bone Joint Surg Br 2003; 85: 100-106.
- Sun L, Song Y, Liu L. One-stage posterior surgical treatment for lumbosacral tuberculosis with major vertebral body loss and kyphosis. Orthopedics 2013, 36: e1082-1090.
- Chandra SP, Singh A, Goyal N. Analysis of changing paradigms of management in 179 patients with spinal tuberculosis over a 12-year period and proposal of a new management algorithm. World Neurosurg 2013; 80:190-203.
- Kotil K, Alan MS, Bilge T. Medical management of Pott disease in the thoracic and lumbar spine: a prospective clinical study. J Neurosurg Spine 2007 6: 222-228.