ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2012) Volume 23, Issue 1
Serum visfatin levels before and after levothyroxin treatment in cases with hypothyroidism and subclinical hypothyroidism and their relationships between the lipid levels
1Gulhane Military Medical Academy, Department of Family Medicine, Etlik/Ankara, Turkey
2Gulhane Military Medical Academy, Department of Internal Medicine, Etlik/Ankara, Turkey,
3Gulhane Military Medical Academy, Department of Biochemistry, Etlik/Ankara, Turkey
4Suleyman Demirel University, Department of Family Medicine, Etlik/Ankara, Turkey
- *Corresponding Author:
- Oktay SARI
Gulhane Military Medical Academy
Department of Family Medicine
Etlik/Ankara
Turkey
Accepted date: August 18 2011
The theory that cases with thyroid disfunction have several lipid metabolism disorders has been suggested in previous studies but there were no previous studies about visfatin levels of patients with thyroid disfunction. In the study, it is aimed to research the role of visfatin in hypothyroid and subclinical hypothyroid status related to dislipidemia after determining the visfatin levels before and after Levothyroxin treatment. Patients with hypothyroidism and subclinical hypothyroidism were enrolled in the study. Patients were chosen randomly and divided into three groups according to their body mass indexes. After first physicial examination, patiens were given Levothyroxin treatment and were to be followed regularly. Total, 43 patients were enrolled in our study; 18.6% of them were hypothyroid and 81.4% were subclinical hypothyroid. 37 patients were female (86%) and 6 were male (14%). Mean age was 45.02±13.23 (16-74) years. After they had become euthyroid and were given Levothroxin treatment, statistically, visfatin levels decreased significantly in all patients (p=0.008, p<0.001). In addition, after Levothyroxin treatment, visfatin levels decreased dramatically in all overweight and obese patients [p=0.010 (for normal weights), p<0.001 (overweights), p=0,010 (obeses)]. After Levothyroxin treatment, serum total cholesterol and LDL cholesterol levels decreased significantly too, but HDL cholesterol levels did not change [p=0.001 (TC), p=0.003 (LDL), p=0.101 (HDL)]. Visfatin levels were positively correlated with TSH levels and negatively correlated with FT3 and FT4 levels. On the other hand, visfatin levels were positively correlated with serum total cholesterol and LDL cholesterol levels and negatively correlated with serum HDL cholesterol levels. Visfatin may have important effects on hypothyroidism and subclinical hypothyroidism related dislipidemia. Due to the likely effects of visfatin, following up visfatin levels may provide a guide for treatment in these conditions.
Keywords
Hypothyroidism, subclinical hypothyroidism, visfatin, lipid levels.
Introduction
It is well known that alterations in thyroid function result in changes in the composition and transport of lipoproteins [1,2]. Generally, overt and subclinical hypothyroidism is associated with hypercholesterolemia mainly due to the elevation of low density lipoprotein (LDL) cholesterol levels, whereas high density lipoprotein (HDL) cholesterol concentration is usually normal or even elevated [3,4].
Adipose tissue is widely considered as a hormonally active system with metabolic effects. The term ‘adipocytokines’ has been coined to designate different bioactive substances derived from adipose tissue that modulates several functions in other tissues [5]. Visfatin is one of the most abundant adipocytokines recently discovered with the capacity to modulate several functions. Visfatin receive much attention as it was reported to function as an insulin sensitizer [6]. Plasma visfatin levels are highly correlated to the amount of visceral fat [6,7]. The role of visfatin in human physiology and pathophysiology remains to be elucidated, while, according to some authors, plasma concentrations of visfatin are elevated in obesity and type 2 diabetes, which are states characterised by insulin resistance [7].
No study, until now, has been reported concerning the possible role of changes in the release of the recently discovered visfatin, in the metabolic disturbances that frequently accompany thyroid dysfunction related to dyslipidemia. In the study, it is aimed to research the likely role of visfatin in hypothyroid and subclinical hypothyroid status related to dislipidemia, after determining the visfatin levels before and after levothyroxine treatment.
Material and Method
Study was performed in 43 patients with overt and subclinical hypothyroidism (18,6% overt, 81,4% subclinical). Patients were divided into three groups according to their BMI levels (Group 1: BMI=18.5-23.9 (normal), Group 2: BMI=24-29.9 (overweight), Group 3: BMI > 30 (obese). Patients with chronic renal failure, congestive heart failure, smokers, pregnant women, hypertansive patients, patients with cancer and drug usage (which may have effects on lipid metabolism) were excluded from the study.
Patients with overt and subclinical hypothyroidism were evaluated at the time of diagnosis and again after normalization of thyroid function following appropriate Levothyroxin therapy. All subjects were ambulatory and were studied as outpatients during visits to the endocrinology and internal medicine clinics. Serum concentrations of free T4 (FT4), free T3 (FT3), TSH, fasting blood glucose, visfatin, thyroid peroxidase autoantibodies, thy roglobuline antibodies, LDL cholesterol, HDL cholesterol, total serum cholesterol levels, and triglyceride levels were measured in all subjects. All patients’ body mass indexes (BMI) were calculated. All patients were treated with the appropriate dose of Levothyroxin therapy to become euthyroid. The dosage of levothyroxine (LT4) was adjusted in an attempt to keep the serum FT4 and TSH concentrations within the normal range. All patients were followed periodically (monthly periods). All patients became euthyroid within 3 months. After 3 months, all parameters were measured again.
Results are given as the mean SEM. Comparisons of mean averages between groups were made using the Student t -test for normally distributed data and the Mann– Whitney U -test for nonparametric data. For paired data, statistical analysis before and after therapy were carried out with the paired Student t -test or the Wilcoxon signedrank test, as necessary. Test 2 was used to study the relationship between qualitative variables. Correlations between variables were assessed using Pearson’s correlation analysis. A value of p<0.05 was accepted as statistically significant. SPSS for Windows vs 12.0 was used for statistical analyses.
Results
Study was performed in 43 patients with overt and subclinical hypothyroidism (18.6% overt, 81.4% subclinical). 37 patients were female (86%) and 6 were male (14%).
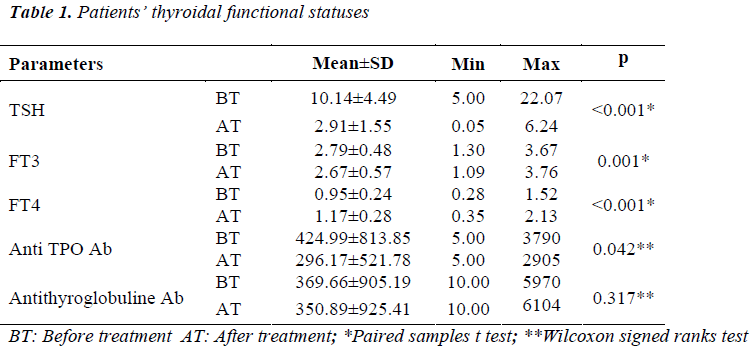
Patients’ thyroidal functional statuses (before and after LT4 treatment) are shown in table 1. All patients’ posttreatmental TSH, FT3 and FT4 levels were euthyroidal. There were statistically significant changes between the pre and posttreatmental measurements of thyroidal functional tests.
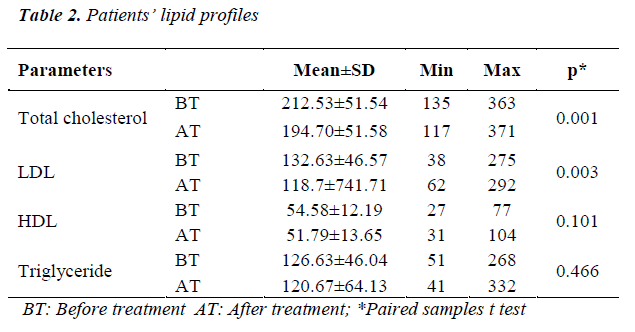
Patients’ lipid profiles (before and after LT4 treatment) are shown in Table 2. There were statistically significant decreases in LDL and total cholesterols after LT4 treatment. However, there were not any differences in HDL cholesterol and triglyceride levels.
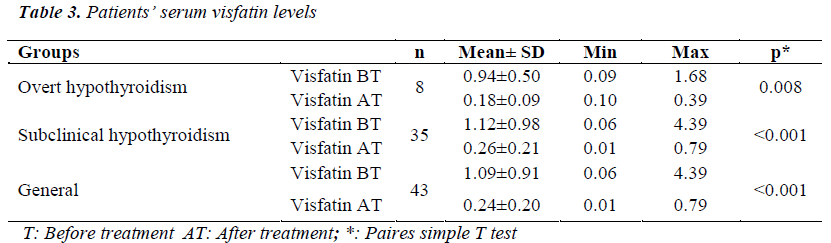
Before LT4 treatment, serum visfatin levels of patients with overt hypothroidism were higher than patients with subclinical hypothyroidism, but this difference was not statistically significant (p=0.619). On the other hand, there was not any significant difference of visfatin after LT4 treatment (p=0.731). After LT4 treatment, statistically, visfatin levels of all the patients decreased remarkably (Table 3). There were not any differences between the serum visfatin levels of male and female patients before and after LT4 treatment. However after LT4 treatment, visfatin levels of all the male and female patients decreased significantly (p=<0.001).
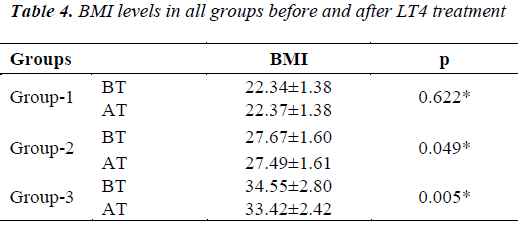
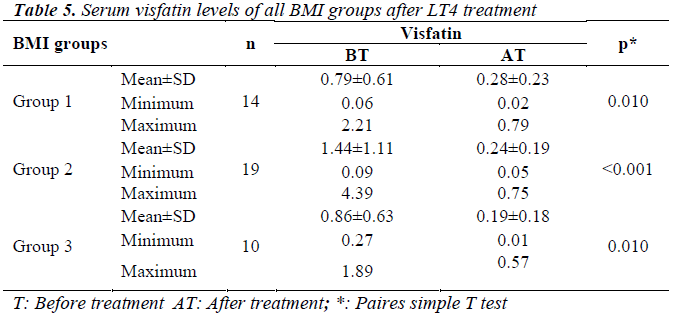
After LT4 treatment, statistically, BMI levels of the patients decreased significantly in Group 2 and 3. Moreover; after LT4 treatment, visfatin levels of all the BMI groups decreased significantly (Tables 4,5).
In the study, visfatin levels were positively correlated with TSH levels and negatively correlated with FT3 and FT4 levels. On other hand visfatin levels were positively correlated with serum total cholesterol and LDL cholesterol levels and negatively correlated with serum HDL cholesterol levels.
Discussion
There have been some debates about normal plasma levels of visfatin. Many authors found visfatin levels between 14-50 ng/ml [8,9]. In one study, plasma visfatin levels were between 1.52-2.9 ng/ml [10]. In this study Takebayashi et al. suggests that plasma visfatin levels are related to envorimental factors and etnicity. In a study of 19 metabolic syndrom patients from Turkey, plasma visfatin levels were between 35.2±22.8 ng/ml [11].
There has not been any study about plasma visfatin levels in overt/subclinical hypothyroid patients. In the study, before Levothyroxin treatment, we found overt/- subclinical plasma visfatin levels of hypothyroid patients at about 1.09±0.91 ng/ml. After getting euthyroid with Levothyroxin treatment, all patients’ visfatin levels decreased to 0.24±0.20 ng/ml. These decreases were statistically significant (p<0.001). On the other hand, these decreases made us think that visfatin may be used as a following marker in hypothyroid patients in the future and may have an important role in hypothroidism treatment protocols in the near future. The pre/post Levothyroxin treatmental visfatin levels of our patients were parallel with the study of Takebayashi et al. Consisting of about 80 type 2 diabetes mellitus patients [10]. In the findings, we suggest that visfatin levels are related to patient groups (ie. diabetic groups, hypothyroid groups etc), etnicity and other envorimental factors. Our different visfatin levels were attributed to this suggestion.
In previous studies, it has been stated that there is no difference between the plasma visfatin levels of males and females [9,10]. In the study, there were no statistically significant differences between the pre/post Levothyroxin treatmental serum visfatin levels of males and females. Study results (serum visfatin levels) were compatible with previous studies. In the light of Levothyroxin effectiveness, visfatin levels of all patients (male and female) decreased after they had bocome euthyroid.
Between three BMI groups (Group 1: BMI=18.5-23.9 (normal), Group 2: BMI=24-29.9 (overweight), Group 3: BMI > 30 (obese)) there were no significant differences of plasma visfatin levels. This finding was not in concordance with the observations made by Berndt et al. [12], who found that plasma visfatin concentration and visceral visfatin expression positively correlated with BMI, and a study of Haider et al. about obese children and high plasma visfatin levels [13]. The reasons for these discrepancies are unclear, but may have been caused by the following factors: (i) ethnic heterogeneity of these studies may affect visfatin level or visfatin sensitivity; (ii) criteria for recruitment were different in the various studies, thus, differences in confounding factors such as age and, lifestyle may affect visfatin levels and other traits of interest and obscure the results. On the other hand, TSH or hypothroidism related factors may have influences on visfatin levels independent from BMI. These suggestions need to be studied in future research.
In the light of lipid profile; total cholesterol, triglyceride and LDL cholesterol levels decreased significantly after proper Levothyroxin treatment. On the other hand, HDL cholesterol levels did not change after partients had become euthyroid. Study results here were parallel with the studies of Jian et al. (in year 2006, in Chinese population) [14] and Bailey et al. (in year 2006, French-Canadian collective working) [15] that serum visfatin levels are decreasing with the improvement of serum lipid profiles. In addition, our results showed that visfatin levels positively correlated with total cholesterol and LDL cholesterol levels before Levothyroxin treatment. After proper Levothyroxin treatment, visfatin levels negatively correlated with LDL levels. All these results suggest that visfatin may have an important role on human body lipid equilibrium. However the mechanism of this role remains unclear and needs to be studied in the future.
Statistically, TSH and FT4 levels of the patients improved significantly after Levothyroxin treatment. This result indicates that we successfully treated our patients properly with Levothyroxin treatment and they become euthyroid. Furthermore, visfatin levels of our patients positively correlated with TSH levels before and after Levothyroxin treatment.
Conclusion
In conclusion, study found that the serum concentration of visfatin has relationships between the overt/subclinical hypothroid status and the status related dyslipidemia, and this study is the first of which has investigated these relationships. Further studies are needed to clarify the molecular relationships between visfatin, thyroid status and lipid metabolism.
References
- Duntas LH. Thyroid disease and lipids. Thyroid 2002; 12 (4): 287-293
- Friis T, Pedersen LR. Serum lipids in hyper- and hypothyroidism before and after treatment. Clin Chim Acta 1987; 162: 155-163
- O.Brien T, Dinneen SF, O.Brien PC, Palumbo PJ. Hyperlipidemia in patients with primary and secondary hypothyroidism. Mayo Clin Proc 1993; 68 (9): 860-866
- Muls E, Rossenen M, Blaton V, Lesaffre E, Lamberigts G, De Moor P. Serum lipids and apolipoproteins AI, AII and B in primary hypothyroidism before and during treatment. Eur J Clin Invest 1984; 14 (1): 12-17
- Maeda K, Okubo K, Shimomura I, Funahashi T, Matsuzawa Y, Matsubara K. cDNA cloning and expression of a novel adipose specific collagen-like factor, apM1 (adipose most abundant gene transcript 1). Biochem and Biophys Res Commun 1996; 221 (2): 286- 289
- Fukuhara A, Matsuda M, Nishizawa M, et al. Visfatin: a protein secreted by visceral fat that mimics the effects of insulin. Science 2005; 21:426-430
- Arner P. Visfatin--a true or false trail to type 2 diabetes mellitus. J Clin Endocrinol Metab. 2006;91:28-30
- Hammarstedt A, Pihlajamaki J, Sopasakis VR at all. Visfatin is an adipostokine but it is not regulated by thiazolidinediones. J Clin Endocrinol Metab 2006; 18: 25-29
- Dogru T, Sonmez A, Tasci I. et al. Plasma visfatin levels in patients with newly diagnosed and untreated type 2 diabetes mellitus and impaired tolerance. Diabetes Res Clin Pract., 2007; 76 (1): 24-33
- Takebayashi K, Suetsugu M, et al. Association between plasma visfatin and vascular endothelial function in patients with type 2 diabetes. Metabolism 2007; 56: 451- 458
- Erdem G, Naharcı MI, Demirtas A, at al. Therapeutıc lıfestyle change ınterventıon ın metabolıc syndrome decreases plasma vısfatın levels. Anatol J Clin Investig 2008; 2 (2): 58-62
- Berndt J, Kloting N, Kralisch S, et al. Plasma visfatin concentrations and fat depot-specific mRNA expression in humans. Diabetes 2005;54: 2911-6
- Haider DG, Holzer G, Schaller G, et all. The adipokine visfatin is markedly elevated in obese children. J. Pediatr Gastroenterol. Nutr 2006; 43: 548-549
- Jian WX, Luo TH, Gu YY, Zhang HL, Zheng S, Dai M, at all. The visfatin gene is associated with glucose and lipid metabolism in a Chinese population. Diabet Med 2006; 23 (9): 967-973
- Bailey SD, Loredo-Osti JC, Lepage P, et al. Common polymorphisms in the promoter of the visfatin gene (PBEF1) influence plasma insulin levels in a French- Canadian population. Diabetes 2006; 55: 2886-2890