ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2023) Volume 34, Issue 3
Relation between body mass index, blood pressure, heart rate and work-related musculoskeletal disorders among healthcare workers in some reference hospitals in Douala, Cameroon.
Basil Kum Meh1,5*, Orelien Sylvain Mtopi Bopda1,6, Franklin Chu Buh1, Jerson Mekoulou Ndongo2, Emmanuel Haddison Sako3, Thelma Akah Eni4,5, Harry Mbacham Fon1,5, Samuel Honoré Mandengue2
1Department of Animal Biology and Conservation, University of Buea, Buea, Cameroon
2Physiology and Medicine of Physical Activities and Sports Unit, University of Douala, Douala, Cameroon
3Department of General Medicine, University of Yaounde I, Yaounde, Cameroon
4Department of Public Health and Hygiene, University of Buea, Buea, Cameroon
5Department of Health Sciences, STEM Higher Institute of Health and Business Douala, Douala, Cameroon
6Department of Biomedical Sciences, University of Buea, Buea, Cameroon
- Corresponding Author:
- Basil Kum Meh
Department of Animal Biology and Conservation
University of Buea
Buea
Cameroon
Accepted date: June 20, 2023
Healthcare workers spend longer hours working without giving much attention to their health, eating habits and consequently, abnormal body weight, blood pressure and heart rate may worsen Work-related Musculoskeletal Disorders (WRMSDs). The study assessed the relation between body mass index, blood pressure, heart rate and WRMSDs among healthcare workers in some Reference Hospitals in Douala, Cameroon. A Cross-sectional, hospital-based study was conducted to assess the relation between Body Mass Index (BMI), Blood Pressure (BP), Heart Rate (HR) and WRMSDs in some Reference Hospitals in Douala, Cameroon. Were included; physicians, nurses, medical laboratory scientists, physiotherapists and other healthcare workers who had worked for at least 12 months. BMI was calculated using the formula: Mass (kg)/height (m2) while BP and HR were measured with the help of an automated blood pressure machine (BP-103 H; arm-type fully automated). WRMSDs was assessed with the Nordic questionnaire, and the relation between BMI, BP, HR and WRMSDs was analyzed using SPSS version 23. Descriptive statistics was used to present proportions while the relation between BMI, BR, HR and WRMSDs was evaluated using the Pearson's chi-square test, and statistical significance was set at P<0.05. 561 healthcare workers who consented were enrolled into the study using a non-probability sampling technique. Generally, 83.4% of healthcare workers had one or more WRMSDs, with 34.7% and 32.4% being overweight and obese, while 52.8% and 94.1% had normal BP and HR respectively. About 63.8% of nurses were obese with 57.2% having above normal HR compared to the other healthcare workers. BMI was significantly related (P=0.016) to WRMSDs in which 90.2% of the obese healthcare workers had one or more WRMSDs. Obesity and overweight are major concerns among nurses. BMI was significantly associated with WRMSDs. Thus, there is need to address overweight/obesity burden among healthcare workers by promoting healthy weight as a way to prevent WRMSDs.
Keywords
Body mass index, Blood pressure, Heart rate, Work-related musculoskeletal disorders, Healthcare workers.
Abbreviations
MD: Medical Doctor; PT: Physiotherapist; SSA: Sub-Saharan Africa; MSDs: Musculoskeletal Disorders; MLS: Medical Laboratory Scientist; WRMSDs: Work Related Musculoskeletal Disorders; WHO: World Health Organization.
Introduction
Moreira-Silva et al. [1] reported elevated rates of overweight and obesity among employed adults and showed a consistent increase over the past few years. Most researchers have published a relation between obesity, musculoskeletal disorders and other none demographic risk factors [1-3]. Body Mass Index (BMI) is regarded as one of the risk factors of WRMSDs among healthcare workers [2]. It is a consistent indicator of body fatness for most individuals and can be used as a screening tool to identify potential weight problems [2]. According to the World Health Organization (WHO) in 2008, over 1.4 billion adults were overweight and more than half a billion were obese [4].
The prevalence of obesity in the adult Cameroonian population increased steadily from 4.9% in the year 2000 to 9.5% in 2016 [5]. There has been a two-fold increase in the age-standardized prevalence of overweight and obesity in rural Cameroon over a period of about 10 years [5]. This highlights the fact that the obesity epidemic is increasingly taking an important place as a cause of disease burden in Cameroon and may deteriorate if no action is taken. Furthermore, Amougou et al. [6], reported prevalence of 30.3% of obesity among healthcare workers in two teaching hospitals in the city of Yaoundé, Cameroon and concluded that obesity is a serious problem and a reality among healthcare workers. Healthcare workers awareness and proper lifestyle promotion programs are more than ever needed to win the fight against obesity [6].
On the other hand, hypertension is a major public health problem. Around 7.5 million deaths or 12.8% of the total of all annual deaths worldwide occur due to high blood pressure [7]. In 1998, the prevalence of hypertension in Cameroon was 18.5% in males, and 12.6% in females, and this increased to 37.2% in males and 37.5% in females in 2012 [8]. A nationwide survey of hypertension showed a prevalence of 29.7% in Cameroon [8]. The prevalence of hypertension among health workers in Yaoundé, Cameroon was 13.9% compared to 24.5% local population-based prevalence [8,9].
Furthermore, Heart Rate (HR) is a readily available vital sign that holds important prognostic information. The normal adult resting HR values lie between 60 and 90 beats per minute (bpm), and the American Heart Association de?nes the normal sinus HR as between 60 and 100 bpm [10].
Over decades, high rates of workplace injury within the health care industry including Work Related Musculoskeletal Disorders (WRMSDs) has been reported [11,12]. WRMSDs are categorized as non-communicable disease and best described as disorders or discomforts sustained by the worker on the musculoskeletal, peripheral nerves, and neurovascular systems resulting from prolonged exposure to repetitive tasks, awkward postures, use of vibrating objects and other workplace hazards [12].
Prevalence rates of WRMSDs of over 70% have been reported in nurses [12,13], physiotherapists [12,13], and in Africa, Abla et al. [14] published a prevalence range of 44.1% to 94% of WRMSDs.
The healthcare sector of Cameroon is still developing, thus monitoring and preventing overweight/obesity, HBP and WRMSDs among healthcare workers is a major concern. Few studies have determined non-demographic risk factors of WRMSDs in isolated hospitals and in single health professional groups in Cameroon [12,13]. Moreover, not much attention has been given on the possible influence of some physiological parameters like BMI, BP and HR on WRMSDs among health care providers. Thus, we evaluated the relation between BMI, BP, and HR on WRMSDs among healthcare workers in some Reference Hospitals in Douala, Cameroon.
Materials and Methods
Study design, setting, and population
A cross-sectional study was carried out between July and August 2022 among 561 healthcare workers from five reference hospitals in the city of Douala, Cameroon. Healthcare workers working in the following hospitals: HLD, GHD, NBDH, NDH and BDH in the city of Douala, Cameroon took part in the study. These are public hospitals, and are among the largest hospitals in city of Douala in terms of capacity, activities and in the number of healthcare workers.
Full-time healthcare workers in the selected reference hospitals who consented to take part in the study and have been working for at least 12 months were included in the study. Were excluded; all participants diagnosed with a musculoskeletal disorder, recent surgery, workers who had any form of accidents before engaging into the medical profession.
Sampling and procedure
A total of 561 respondents were recruited in the study using a non-probability sampling method, since participants were recruited according to their availability.
The sample size was calculated with the Lorenz formula:
N=P(1-P) Z2/D2
where N is the minimum sample size; p is the prevalence of MSDs (65%) in the range reported previously by Abla et al. [14], z is the statistic for the desired confidence level (Z=1.96 for confidence at 95%), and d is the accepted margin of error (D=0.05). The estimated sample size was n=350. The authors ended up recruiting 561 participants in view of increasing the power and significance of the study.
Data collection
Socio-demographic features: Demographics data were collected using a well-designed questionnaire. The questionnaires were administered through a face-to-face interview. Data collected included: Demographic and personal profiles (age groups, specialty and place of work).
Assessment of work-related musculoskeletal disorders: WRMSDs was assessed with the use of the Nordic questionnaire proposed by researchers from the Institute of Public Health of Scandinavian countries which assesses WRMSDs in nine sites of the body including the neck, shoulders, elbows, wrists/thighs, knees and ankles at two different moments preceding the survey, 7 days and 12 months [15].
Validity of the questionnaire
After a deep literature review by the author and co-authors, the content of the questionnaires and the different tools used for data collection, including the modified Nordic questionnaire was validated and accepted to be used in this study. Secondly, a pretest was carried out using the research tools and the results were compared from that obtained from another instrument and the results were validated by the expert panel.
Clinical data (BMI, BP and HR)
A non-invasive recording of the blood pressure and the heart rate were obtained for all participants who gave their consent using an automated blood pressure machine (BP- 103 H; arm-type fully automated). Normal blood pressure is defined as a systolic BP<120 mmHg and diastolic BP<80 mmHg according to the Joint National Committee while hypertension is defined as systolic BP level of ≥ 140 mmHg and/or diastolic BP level ≥ 90 mmHg [16]. The weight of all the participants who gave their consent were also measured with a weighing balance and their BMI calculated using the formula: Weight/(height (m2) and if ≥ 25 ≤ 29.9 kg/m² a person is classi?ed as being overweight, while a BMI of 30-34.9 was considered light obesity, 35.0- 39.9 is classified as moderate obesity, morbid obesity is having a BMI greater than or equal to 40.0 (BMI ≥ 40.0), and super obesity is having a BMI greater than or equal to 50.0 (BMI ≥ 50.0) [17].
Heart rate: Below normal (<60 beats per minute), Normal (60-100 beats per minute), above normal (>100 beats per minute) [10].
Data analysis
The data collected was verified, cleaned and analyzed with SPSS version 23 (SPSS Inc., Chicago, IL, USA). Descriptive statistics was used to analyze proportions of BMI, BP and HR while Pearson independence (X2) test to assess the relation between groups. Statistical significance was set at P>0.05 while results were presented on tables and figures.
Results
Socio-demographic characteristics of healthcare workers in Douala hospitals
Five hundred and sixty-one (561) participants took part in this study. The average age of participants was 34.10 years. Participants between the ages of 30 and 39 were most represented (41.4%). Majority (62.9%) of the study participants were nurses followed by MLS (14.3%), and a greater majority worked at LHD (26.4%). Out the 561 participants who took part in the study, 83.4% (468/561) had one or more WRMSDs (Table 1).
| Factor | Variable | Frequency (n) | Percentage (%) |
|---|---|---|---|
| Age group (Years) | 20-29 | 207 | 36.9 |
| 30-39 | 232 | 41.4 | |
| 40-49 | 87 | 15.5 | |
| 50-59 | 35 | 6.2 | |
| Specialty | MLS | 80 | 14.3 |
| MD | 52 | 9.3 | |
| Nurses | 353 | 62.9 | |
| PT | 26 | 4.6 | |
| Others | 50 | 8.9 | |
| Place of work | LHD | 148 | 26.4 |
| GHD | 136 | 24.2 | |
| BDH | 103 | 18.4 | |
| NBDH | 56 | 10.0 | |
| NDH | 115 | 21.0 | |
| WRMSDs | Positive | 468 | 83.4 |
| Negative | 93 | 16.6 |
Table 1. Demographic characteristics and prevalence of work-related musculoskeletal disorders in Douala hospitals.
Prevalence of BMI, BP and HR of participants
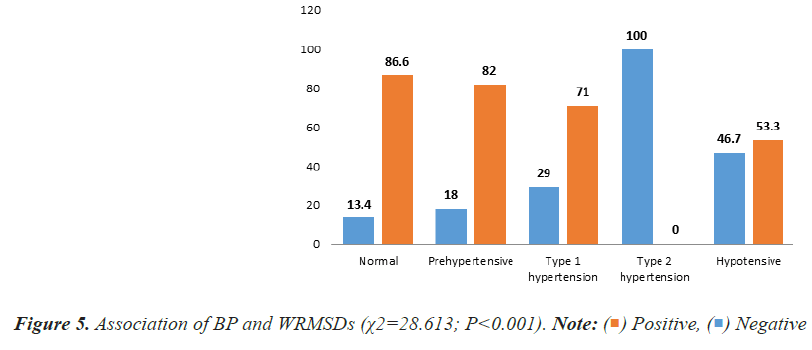
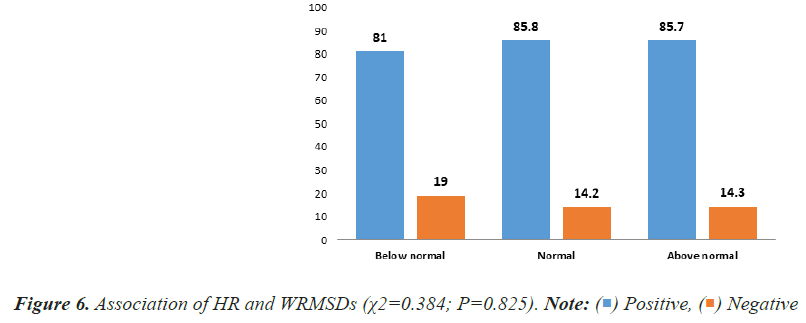
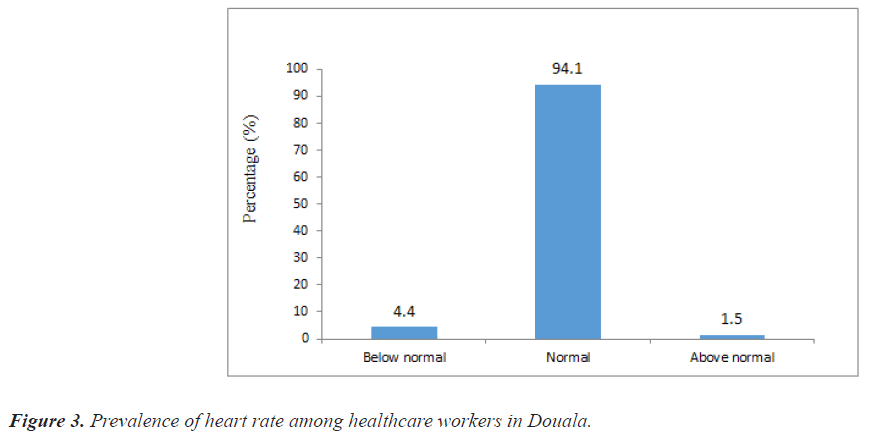
Out of the 561 healthcare workers recruited in the study, 510, 481 and 472 consented to provide their body BMI, BP and HR respectively. The mean ± SD of BMI was 27.38 ± 5.748 Kg/m2 while the mean ± SD of systolic and diastolic BP were 118.15 ± 14.830 mmHg and 75.04 ± 11.489 mmHg respectively. Majority of the study participants (34.7%) were overweight (BMI: 25-29.9), 32.2% were obese (BMI ≥ 30 kg/m2), while just a few (1.6%) were underweight (Figure 1). The study revealed that more than half of the healthcare workers had normal (52.8%) BP, while just a few were diagnosed with type 1 (6.4%) type 2 (0.6%) hypertension (Figure 2). Furthermore, majority of the study participants presented with a normal HR while at work (94.1%) as shown in Figure 3.
Prevalence of BMI, BP and HR with respect to specialty and place of work
It was observed that most obese healthcare workers were nurses (63.8%) as shown in Table 2 and they worked predominantly in LHD (33.1%) (Table 2). Also, most of the nurses (66.7%) were the healthcare workers who presented more with type 2 hypertension compared to the other healthcare workers (Table 3) while type 2 hypertension was more common in GHD (100%) (Table 3). More so, the nurses (57.2%) (Table 4) present more with above normal heart rate which was predominantly observed in the LHD (57.1%) as seen in Table 4.
| Specialty | Body mass index (N = 510) | |||
|---|---|---|---|---|
| Underweight %(N) | Normal weight %(N) | Overweight %(N) | Obese %(N) | |
| MLS | 25.0 (2) | 13.6 (22) | 14.1 (25) | 10.4 (17) |
| MD | 12.5 (1) | 12.3 (20) | 10.2 (18) | 7.4 (12) |
| Nurse | 50.0 (4) | 63.6 (103) | 62.1 (110) | 63.8 (104) |
| PT | 0.0 (0) | 4.3 (7) | 2.8 (5) | 7.4 (12) |
| Others | 12.5 (1) | 6.2 (10) | 10.7 (19) | 11.0 (18) |
| Hospital type | ||||
| LHD | 37.5 (3) | 24. (39) | 24.3 (43) | 33.1 (54) |
| GHD | 12.5 (1) | 24.7 (40) | 26.6 (47) | 23.3 (38) |
| BDH | 12.5 (1) | 20.4 (33) | 16.4 (29) | 12.3 (20) |
| NBDH | 0.0 (0) | 11.7 (19) | 7.9 (14) | 9.8 (16) |
Table 2. Prevalence of body mass index with respect to specialty.
| Specialty | Blood pressure (N = 481) | ||||
|---|---|---|---|---|---|
| Normal % (N) | Prehypertension % (N) | type 1 hypertension % (N) | Type 2 hypertension % (N) | Hypotension % (N) | |
| MLS | 9.8 (25) | 16.9 (30) | 19.4 (6) | 0.0 (0) | 20.0 (3) |
| MD | 10.2 (26) | 7.9 (14) | 3.2 (1) | 0.0 (0) | 0.0 (0) |
| Nurse | 68.5 (174) | 59.6 (106) | 71.0 (22) | 66.7 (2) | 80.0 (12) |
| PT | 2.8 (7) | 6.7 (12) | 3.2 (1) | 33.3 (1) | 0.0 (0) |
| Others | 8.7 (22) | 9.0 (16) | 3.2 (1) | 0.0 (0) | 0.0 (0) |
| Hospital | |||||
| LHD | 26.8 (68) | 0.0 (0) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
| GHD | 46.1 (117) | 0.0 (0) | 45.2 (14) | 100.0 (3) | 13.3 (2) |
| BDH | 18.9 (48) | 17.4 (31) | 54.8 (17) | 0.0 (0) | 46.7 (7) |
| NBDH | 5.5 (14) | 20.2 (36) | 0.0 (0) | 0.0 (0) | 40.0 (6) |
| NDH | 2.8 (7) | 62.4 (111) | 0.0 (0) | 0.0 (0) | 0.0 (0) |
Table 3. Prevalence of blood pressure with respect to specialty.
| Specialty | Heart rate (N = 472) | ||
|---|---|---|---|
| Below normal % (N) | Normal % (N) | Above normal % (N) | |
| MLS | 14.3 (3) | 11.8 (53) | 28.6 (2) |
| MD | 9.5 (2) | 10.4 (46) | 0.0 (0) |
| Nurse | 71.4 (15) | 64.2 (285) | 57.1 (4) |
| PT | 0.0 (0) | 5.0 (22) | 0.0 (0) |
| Others | 4.8 (1) | 8.6 (38) | 14.3 (1) |
| Hospital | |||
| LHD | 23.8 (5) | 29.7 (132) | 57.1 (4) |
| GHD | 23.8 (5) | 25.9 (115) | 28.6 (2) |
| BDH | 23.8 (5) | 14.6 (65) | 14.3 (1) |
| NBDH | 0.0 (0) | 8.8 (39) | 0.0 (0) |
| NDH | 28.6 (6) | 20.9 (93) | 0.0 (0) |
Table 4. Prevalence of heart rate with respect to specialty.
Association between BMI, BP, and HR with work-related musculoskeletal disorders
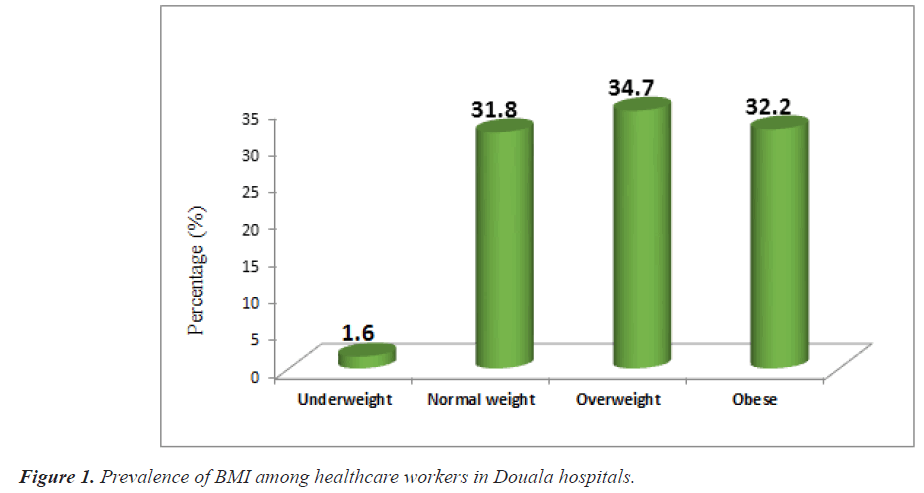
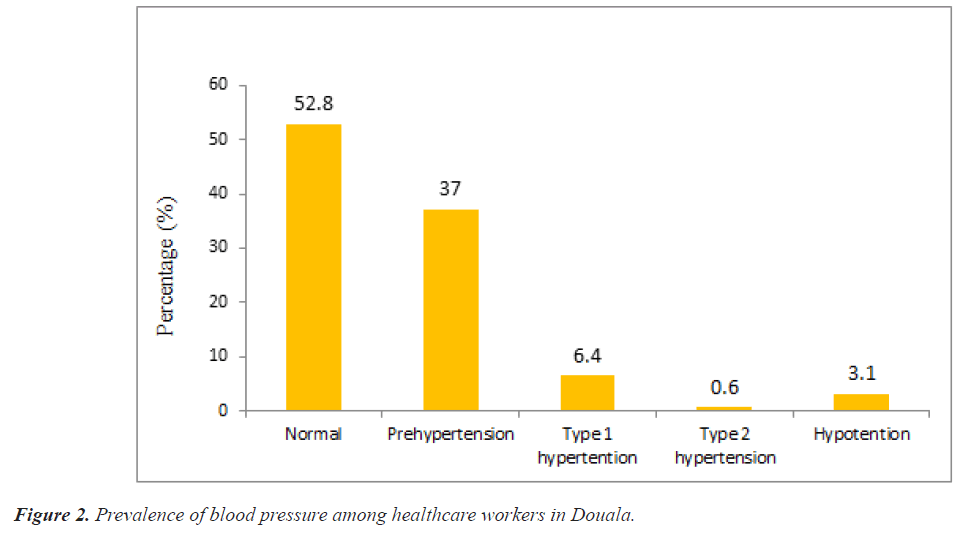
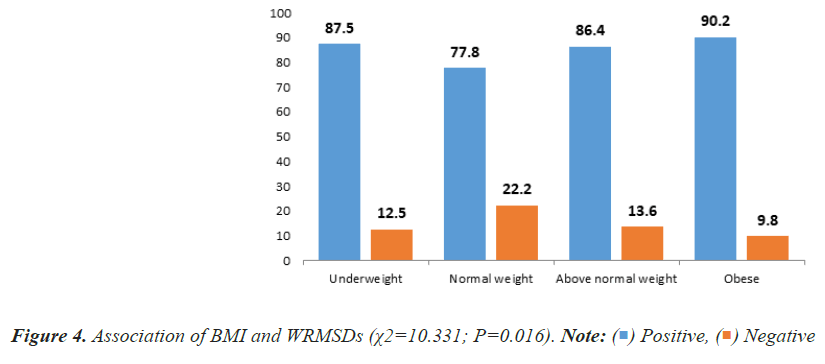
The study further evaluated the relation between BMI, BP, HR and WRMSDs. There was a statistically significant relation (P=0.016) between BMI and WRMSDs in which, majority (90.2%) of the obese healthcare workers had one or more WRMSDs (Figure 4). Also, there was a statistically significant relation (P<0.001) between WRMSDs and blood pressure in which, healthcare workers with normal blood pressure (86.6%) presented with WRMSDs while healthcare workers with type 2 hypertension were significantly void of WRMSDs (Figure 5). There was no statistical relation between WRMSDs and HR (Figure 6).
Discussion
The study aimed at investigating the relation between BMI, BP and HR with WRMSDs among healthcare workers in Douala Hospitals. Most of the participants (70.6%) were females, consistent with the study of Abla et al. [14], where the females made up about 75% of the study population. Majority (62.9%) of the study participants were nurses which constitute a greater proportion of the healthcare workforce.
The study found that about 34.7% and 32.2% were overweight and obese respectively. This results disagrees with the study of Darebo et al. [19] in Ethiopia and Ijoma et al. [20] in southeast Nigeria where the prevalence of obesity was found to be about 28.2% and 10.9% respectively in their study populations. This difference could be due to the differences in socio-cultural and environmental determinants as reported by Lee et al. [21]. However, the results from this study was partly in line with the study of Simo et al. [5], where the prevalence of overweight was 31.1% and obesity 18.9%. The obesity prevalence rate seen in the present study may also be secondary changes in diet, and the adoption of sedentary lifestyles [22].
Most of the participants had a normal BP (52.8%) and normal HR (94.1%), may be because of the fact that majority of the study population were of the age group 30-39 and were not married, and being married and age according to the study of Seher et al. [23], are potential risk factors of hypertension. About 37% and 7% of the healthcare workers were pre-hypertensive and hypertensive respectively. This is a warning sign that if proper preventive measures are not taken, the prevalence of hypertension may increase in the study population from 7% to about 30% or even 40% as seen in the study of Defo et al.[24]. The prevalence of pre-hypertension in the present study is slightly similar to the prevalence (21.5%) obtained by Jingi et al. [25] among primary care physicians in Cameroon. This slight difference could be due to the fact that Jingi and collaborators considered only physicians in their study.
With respect to specialty, majority of the nurses were obese (63.8%), had type 2 hypertension (66.7%) and heart rates above normal (57.2%). This disagrees with the study of Zapka et al., [26] were about 37% of nurses were overweight and only 28% were obese. This difference could be due social, cultural and environmental factors. Also, the prevalence of hypertension in the present study population was slightly higher than the prevalence reported by Bosu et al., [27], in West Africa and Amougou et al. [8] who conducted their study among health workers in two teaching hospitals in Yaoundé-Cameroon. These differences could be attributed to the fact that many health workers were considered in their studies, and the sample size could have influenced the result of this study.
There was a statistically significant relation between BMI and WRMSDs in which, majority of the obese healthcare workers had one or more WRMSDs. This results is similar to that reported by Sethi et al. [28] Moreira-Silva et al. [1] and Paul et al. [29] whose findings indicated that workers with high BMI were found to be at risk of developing WRMSDs. However, the results from the study of Sayed et al. [30] did not agree with that of our present study. They indicated that there was no relation between BMI and WRMSDs, maybe because of the difference in environmental, cultural, social and behavioural factors.
There was no clear relation between BP and HR with WRMSDs as healthcare workers with normal BP, type 2 hypertension, hypotension, normal HR and above normal HR reported with WRMSDs, similar to the study of Sotrate et al. [31] who reported no relation between BP and HR with WRMSDs.
Despite that, much work have been done on the relation between BP and HR in the development of WRCVDs [5,23,32]. Increases in BP, HR and other factors such as diabetes, tobacco use, obesity, and sedentarily lifestyle increases the risks of developing WRCVDs among the working population [9,33-35]. Less work has been done on the relation between BP, HR and WRMSDs `in Cameroon. The results obtained from this study therefore encourages more research, using case study approach and longitudinal studies to determine the actual relation between BP, HR and WRMSDs, to bridge the knowledge gap.
Limitations and perspectives
The present study has some limitations that should be considered. The measurements were carried out at the workplace, which may have led to a lack of concentration by the health workers, since their work was interrupted. Another limitation is the cross-sectional design which does not allow causal inferences. Cross-sectional studies measure exposure and outcome at the same time and it is often difficult to establish a temporal relation between exposure and outcome, that is, whether exposure or disease occurs first. Future studies should include participants’ follow up in a longitudinal design.
Also, we did not consider other factors such as exposure to poor working posture, work stress, working with vibrating objects, repetitive tasks, standing or sitting for long that have been reported in many studies as potential risk factors of WRMSDs [10,12,13,17,18,30].
In spite of these limitations, the present findings indicate prospects for future studies among healthcare workers in Cameroon and the Sub-Saharan Africa in general.
Conclusion
Obesity and overweight are major concerns among healthcare workers particularly in the nursing profession in Douala hospitals, Cameroon. BMI was found to be significantly associated with WRMSDs among health care workers in Douala, Cameroon.
There was no clear relation between blood pressure, heart rate and WRMSDs among healthcare workers in Douala hospitals as seen in this study. Further studies with longitudinal design would provide more insights for a more global conclusion.
Acknowledgments
Our sincere gratitude goes to the participants of this study for all their time and patience, which greatly contributed to the completion of this work. Equally, we thank Madam SIH Mary Progress and AKIH Victoire MANG for proofreading this article and making relevant corrections that have greatly ameliorated the quality.
Declarations
Ethical consideration
Ethical clearance (No. 2021/1511-07/UB/SG/IRB/FHS) was obtained from the Institutional Review Board (IRB) of the Faculty of health science of the University of Buea (UB) while administrative authorizations were obtained from the Douala regional delegation of public health and hospital directors. For ethical reasons, names of hospitals were coded. The fundamental principles of medical research according to Helsinki’s Declaration were strictly respected.
Consent for publication
All the authors consented and accepted for this article to be submitted for publication.
Availability of data and materials
Most data generated or analysed during this study are included in this article.
Conflict of Interest
The authors certify there is no conflict of interest.
Funding
This research did not receive any grant from funding agencies.
Author’s Contribution
B. K.M: Study conception, design, data collection, analysis, results interpretation and writing. B.M.O.S: Study conception, design, writing and editing. FCB: data collection, writing and editing. T.A.E: results interpretation, writing, and editing. J.M.N: study design, writing and editing. H.M.F: data analysis, writing and editing. E.H.S: study design, data collection and editing. M.S.H. study design, editing and validation. All Authors fully reviewed the manuscript.
References
- Moreira-Silva I, Santos R, Abreu S, Mota J. Associations between body mass index and musculoskeletal pain and related symptoms in different body regions among workers. SAGE Open 2013; 3: 2158244013491952.
- Gothey AI, Lembariti BS. Work-related musculoskeletal disorders and associated factors among dental professionals in Tanzania. J Oral Health Comm Dent 2022; 16: 26-29.
- Frilander H, Solovieva S, Mutanen P. Role of overweight and obesity in low back disorders among men: A longitudinal study with a life course approach. BMJ Open 2015; 5: e007805.
[Google Scholar] [PubMed] [Crossref]
- Rautela YS, Reddy BV, Singh AK, Gupta A. The prevalence of obesity among adult population and its association with food outlet density in a hilly area of Uttarakhand. J Family Med Prim Care 2018; 7: 809-814.
[Google Scholar] [PubMed] [Crossref]
- Simo LP, Agbor VN, Temgoua FZ. Prevalence and factors associated with overweight and obesity in selected health areas in a rural health district in Cameroon: A cross-sectional analysis. BMC Public Health 2021; 21: 475.
[Google Scholar] [PubMed] [Crossref]
- Amougou SN, Tchangoum LL, Gweth MN, Danwe D, Maadjjhou CM, Kingue S, Mbanya JC. Epidemiological profile of obesity among health staff at the Yaoundé central hospital and at the Yaoundé university teaching hospital. World J Cardiovas Dis 2019; 9: 511-523.
- Shikha Singh, Ravi Shankar, Gyan Prakash Singh. "Prevalence and associated risk factors of hypertension: A cross-sectional study in urban Varanasi". Int J Hyperten 2017; 5491838.
[Google Scholar] [PubMed] [Crossref]
- Amougou SN, Tchokote KK, Hamadou B, Jingi AM, Nganou-Gnindjio CN, Ngwet MN, Kuaté LM, Jemea B, Epok LE, Danwé D, Kingue S. Prevalence, awareness, and control of hypertension in health workers of two teaching hospitals of Yaounde-Cameroon: The Hypertension Awareness Initiative (THAI) pilot survey. Open Access Library Journal August 2018; 5: 1-10.
- Danwe D, Amougou SN, Choumi AT, Ouankou CN, Bala LA, Adala PS, Lemogoum D. Prevalence, awareness and control of high blood pressure in a semi-urban area of cameroon: An analysis of may measurement month 2019 screening results. Open Access Library Journal 2019; 6: 1-7.
- Avram R, Tison GH, Aschbacher K, Kuhar P, Vittinghoff E, Butzner M, Runge R, Wu N, Pletcher MJ, Marcus GM, Olgin J. Real-world heart rate norms in the Health eHeart study. npj Digit Med 2019; 2: 58.
[Google Scholar] [PubMed] [Crossref]
- Yasobant S, Rajkumar P. Work-related musculoskeletal disorders among health care ssprofessionals: A cross-sectional assessment of risk factors in a tertiary hospital, India. Indian J Occu Environ Med 2014; 18: 75-81.
[Google Scholar] [PubMed] [Crossref]
- Esembeson M, Abia W, Longdoh NA, Cyrille N, Mokake D, Nde-Fon P, Ngunde PJ, Halle-Ekane GE. Prevalence of work-related musculoskeletal disorders and risk factors amongst nurses of Buea and Tiko health districts, South West Region, Cameroon. Int J Trend Sci Res Develop 2020; 4: 1216-1223.
[Crossref]
- Buh CK, Kuate T, Vera V. Prevalence and risk factors of work related musculoskeletal disorders among nurses and physiotherapists in Douala: A descriptive cross-sectional study. Int J Adv Res Rev 2021; 6: 35-47.
- Abla Kofi-Bediako W, Sama G, Yarfi C, Ed-Bansah D, Appah Acquah A. Work-related musculoskeletal disorders among nurses at the Ho Teaching Hospital, Ghana. InProceedings of the Human Factors and Ergonomics Society Annual Meeting 2021; 65: 1291-1294.
- Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sørensen F, Andersson G. Standardised nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987; 18: 233-237.
[Google Scholar] [PubMed] [Crossref]
- De la Sierra A. New American and European hypertension guidelines, reconciling the differences. Cardiol Ther 2019; 8: 157-166.
[Google Scholar] [PubMed] [Crossref]
- Weir CB, Jan A. BMI classification percentile and cut off points. StatPearls [Internet] 2022.
[Google Scholar] [PubMed]
- Meh B, Bopda O, Ndongo J, Buh F, Léle C, Ayina C, Ndemba P, Sako E, Bongue B, Mandengue S. Epidemiological patterns of work-related musculoskeletal disorders among healthcare workers in five reference hospitals in the city of Douala, Cameroon. Open J Prev Med 2023; 13: 109-128.
- Darebo T, Mesfin A, Gebremedhin S. Prevalence and factors associated with overweight and obesity among adults in Hawassa city, southern Ethiopia: A community based cross-sectional study. BMC Obes 2019; 6: 8.
[Google Scholar] [PubMed] [Crossref]
- Ijoma UN, Njoku PO, Arodiwe EB, Ijoma CK. Increasing trend of overweight and obesity in a rural community in South East Nigeria. Open J Epidemiol 2020; 10: 323-333.
- Lee A, Cardel M, Donahoo WT. Social and environmental factors influencing obesity. Endotext 2015.
[Google Scholar] [PubMed]
- Fox A, Feng W, Asal V. What is driving global obesity trends? Globalization or "modernization"?. Global Health 2019; 15: 1-6.
[Google Scholar] [PubMed] [Crossref]
- Seher K, Funda K. The prevalence of hypertension and influencing factors among the employees of a university hospital. Afr Health Sci 2020; 20: 1725-1733.
[Google Scholar] [PubMed] [Crossref]
- Kuate Defo B, Mbanya JC, Kingue S, Tardif JC, Choukem SP, Perreault S, Fournier P, Ekundayo O, Potvin L, D'Antono B, Emami E, Cote R, Aubin MJ, Bouchard M, Khairy P, Rey E, Richard L, Zarowsky C, Mampuya WM, Mbanya D, Sauvé S, Ndom P, Silva RBD, Assah F, Roy I, Dubois CA. Blood pressure and burden of hypertension in Cameroon, a microcosm of Africa: A systematic review and meta-analysis of population-based studies. J Hypertens 2019; 37: 2190-2199.
[Google Scholar] [PubMed] [Crossref]
- Jingi AM, Noubiap JJN. Cardiovascular risk factors awareness and prevalence among primary care physicians: An insight from the West region Awareness Initiative survey to fight Cardiovascular Disease (WAIT-CVD) in Cameroon. BMC Res Notes 2015; 8: 762.
[Google Scholar] [PubMed] [Crossref]
- Zapka JM, Lemon SC, Magner RP, Hale J. Lifestyle behaviours and weight among hospital-based nurses. J Nurs Manag 2009; 17: 853-860.
[Google Scholar] [PubMed] [Crossref]
- Bosu WK. The prevalence, awareness, and control of hypertension among workers in West Africa: A systematic review. Glob Health Action 2015; 8: 26227.
[Google Scholar] [PubMed] [Crossref]
- Sethi J, Sandhu JS, Imbanathan V. Effect of Body Mass Index on work related musculoskeletal discomfort and occupational stress of computer workers in a developed ergonomic setup. BMC Sports Sci Med Rehabil 2011; 3: 22.
[Google Scholar] [PubMed] [Crossref]
- Paul A., Gregory R, Aleck O. Work, obesity, and occupational safety and health. J Public Health 2007; 97: 428-436.
[Google Scholar] [PubMed] [Crossref]
- Sayed A, Batool A, Amina A. Work-related musculoskeletal disorders among employees with different tasks: An ahlia university case study. Physiotherapy Quarterly 2020; 30: 59-64.
- Sotrate Gonçalves J, de Oliveira Sato T. Factors associated with musculoskeletal symptoms and heart rate variability among cleaners: Cross-sectional study. BMC Public Health 2020; 20: 774
[Google Scholar] [PubMed] [Crossref]
- Cook S, Togni M, Schaub MC, Wenaweser P, Hess OM. High heart rate: A cardiovascular risk factor?. Eur Heart J 2006; 27: 2387-2393.
[Google Scholar] [PubMed] [Crossref]
- Kazemi T, Sharifzadeh G, Javadinia SA, Salehiniya H. Prevalence of cardiovascular risk factors among the nurse population in the East of Iran. Int J Travel Med Glob Health 2015; 3: 133-136.
- Timnou AT, Boombhi J, Njonnou SJ, Jingi AM, Efon KN, Bâ H, Mfeukeu-Kuate L, Nganou-Ngnindjo CN, Amougou SN, Essomba MJ, Kebiwo OK. Prevalence of hypertension and associated risk factors among a group of prisoners in Yaoundé central prison: A cross-sectional study. J Xiangya Med 2019; 4: 22-29.
- Kolkenbeck-Ruh A, Soepnel LM, Crouch SH. Obesity, hypertension, and tobacco use associated with left ventricular remodelling and hypertrophy in South African women: Birth to twenty plus cohort. BMC Cardiovasc Disorder 2022; 22: 1-1.
[Google Scholar] [PubMed] [Crossref]
 Positive,
Positive,  Negative
Negative