ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2005) Volume 16, Issue 3
Reduced blood glutathione and erythrocyte stability in osteoarthritis
G.M. Rao, Sreelaxmi, A. Naser and Vandana
Department of Biochemistry, Kasturba Medical College, Mangalore, India
- Corresponding Author:
- Dr. Gayathri.M. Rao
Department of Biochemistry
Centre for Basic Sciences K.M.C
Mangalore 575 004, India
e-mail: gayatrimrao ( at ) yahoo.com
Accepted date: October 7 2005
Inflammation and oxidative stress are believed to function as primary degenerative mechanism in the development and progression of osteoarthritis. Oxidants can inactivate latent collagenase and potentiate the damage. In the present study an attempt was made to study the nonessential endogenous antioxidants like reduced glutathione (GSH) and uric acid levels. Reduced glutathione in R.B.C. levels decreased significantly (p= 0.011) in the osteoarthritic group. Plasma uric acid levels showed a tendency to increase, however remained statistically insignificant. Oxidative stress was studied by evaluating the percent hemolysis and the study group showed a significant increase (p= 0.001) when compared with the control group. There was a significant drop in the hemoglobin (Hb) level (p= 0.003) in the study group. Reduced levels of GSH allow peroxides to accumulate in RBC and hemolysis can occur due to their oxidative effect on the lipid RBC membrane, which may be one of the cause for the observed decrease in the erythrocyte stability reflected by the increase in the percent hemolysis and decrease in the Hb level.
Keywords
Oxidative stress, osteoarthritis, latent collagen, endogenous antioxidants, glutathione
Abstract
Inflammation and oxidative stress are believed to function as primary degenerative mechanism in the development and progression of osteoarthritis. Oxidants can inactivate latent collagenase and potentiate the damage. In the present study an attempt was made to study the nonessential endogenous antioxidants like reduced glutathione (GSH) and uric acid levels. Reduced glutathione in R.B.C. levels decreased significantly (p= 0.011) in the osteoarthritic group. Plasma uric acid levels showed a tendency to increase, however remained statistically insignificant. Oxidative stress was studied by evaluating the percent hemolysis and the study group showed a significant increase (p= 0.001) when compared with the control group. There was a significant drop in the hemoglobin (Hb) level (p= 0.003) in the study group. Reduced levels of GSH allow peroxides to accumulate in RBC and hemolysis can occur due to their oxidative effect on the lipid RBC membrane, which may be one of the cause for the observed decrease in the erythrocyte stability reflected by the increase in the percent hemolysis and decrease in the Hb level.
Introduction
Both inflammation and oxidative stress are believed to function as primary degenerative mechanisms in the development and progression of osteoarthritis. It is a chronic, most common form of arthritis and is called the wear and tear arthritis in which the cartilage breaks down. There are two categories of osteoarthitis. Primary osteoarthritis appears without any apparent cause, usually as a result of aging. Secondary osteoarthritis occurs in joints that have sustained injuries, experienced infections, obesity, fractures or secondary to another type of arthritis.
Movement of the inflamed joints provides the potential patho- physiological environment for the production of oxidative stress through free radical generation by hypoxic reperfusion injury [1]. Chen and his colleges [2] discovered a high predisposition to free radical release and tissue damage in osteoarthritis.
Other researchers have called attention to the role of the free radicals in actual destruction of joint tissue in osteoarthritis and emphasized the importance in utilizing antioxidants and free radical scavengers in treating the disease [3].
One theory about the role of oxidative stress in joint pain emphasizes the movement and blood flow. Articular cartilage is unique because it is nonvascular and depends directly on movement for nourishment. Motion of the ligaments and tendons surrounding the joint facilitates nutriant delivery to the cartilage by allowing nearby blood vessels to fully dilate. When movement is absent and the synovial pressure becomes greater than the pressure in the nearby blood vessels, the vessels can collapse and may result in hypoxic reperfusion injury [4]. This process involves the greater ironies of oxygen metabolism and ROS (Reactive Oxygen Species) production and risk of cell damage. One of the study shows that, synovial cavity damage correlates with fluctuating oxygen pressure in the joint, over production of reactive oxygen species (ROS), and lack of oxygen processing enzymes and free radical scavenging molecules.
Various oxygen radical stresses have been shown to result in GSSG formation and short term depletion of GSH [5]. Reduced glutathione (GSH) is also capable of directly scavenging radicals and peroxides by being oxidized to either GSSG or to a mixed disulphide, thereby preventing cell membrane lipid peroxidation and subsequent deleterious effects of cellular functions [6].
The reducing power of GSH is the key to multiple actions of GSH at the molecular and cellular levels and to its effectiveness as a systemic antitoxin [7]. Intracellular GSH appears to be a sensitive indicator of cells overall health, and its ability to resist toxic challenge. Hence in the present study we made an attempt to evaluate the levels of reduced glutathione, hemoglobin and extent of hemolysis and uric acid in osteoarthritic subjects.
Subjects and Methods
Blood was collected from osteoarthritic subjects (n= 17) and age and sex matched healthy volunteers (n= 17) by venipuncture. Whole blood was taken for the estimation of reduced glutathione and hemoglobin. Rest of the blood was immediately centrifuged at 3000 rpm for 10 minutes. Plasma and buffy coat were carefully removed and the separated red blood cells washed thrice with cold saline-phosphate buffer. The washed RBC was used for the estimation of percent hemolysis.
Reduced glutathione was estimated in whole blood by the method of Butler et al [8]. Percent hemolysis was studied by the method of Kartha and Krishnamoorthy [9]. Hemoglobin level was estimated by cyanmethemoglobin method [10]. The method adopted for the study of plasma uric acid level was that of method of Gowenlock, Mc-Murry, McLauchlan [11].
Statistical analysis was done by Mann-Whitney test.
Result
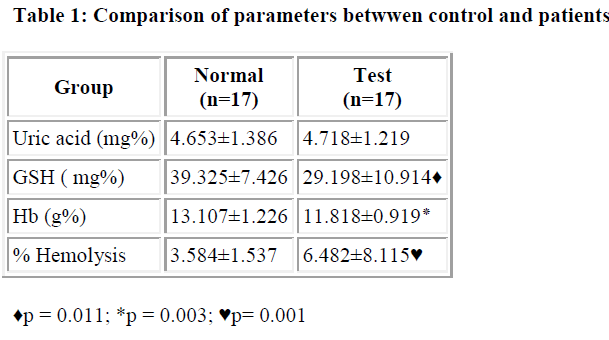
As shown in the table, plasma uric acid levels observed in the study group remained in the normal control range. Percent hemolysis showed a tendency to increase significantly (p= 0.001) in osteoarthritis group whereas hemoglobin (p= 0.003) and reduced glutathione (p= 0.011) levels in the blood were significantly decreased when com-pared with the normal controls
Discussion
Defense against oxidative stress is primarily dependent upon an orchestrated synergism between several endogenous and exogenous antioxidants. In the face of endogenous oxidative burden, the formidable reducing power of GSH is a profound physiochemical asset for the aerobic organism. Although higher concentrations of GSH have been associated with good health, the significance of low GSH status in elderly is inferred from limited data [12, 13]. Intracellular depletion of GSH can be due to either by forming a direct complex with an electrophilic agent or via inhibition of synthesis or by subjecting cell to oxidati-ve stress [5]. Severe depletion of GSH effects numerous cell functions [14]. Many enzymes are GSH dependent and their activity may be regulated by thiol disulphide exchange and thus dependent on the GSH status. Many experimental approaches show that the cell not only become more susceptible to any further challenge, but their basic functions are also perturbed by extensive GSH depletion [15].
Investigators have noted lower GSH concentrations have to be associated with the combination of advanced age and increased risk of chronic diseases such as chronic renal failure, malignant disorders, diabetes cataract formation, Parkinson’s disease etc. It has been postulated that the oxidation- reduction status of GSH may acts as a 3rd messenger in either enhancing or diminishing the activities of a number of biological processes, such as enzyme catalysis, protein synthesis and receptor binding [16]. Reduced levels of GSH allow peroxides to accumulate in erythrocytes and hemolysis can occur due to their oxidative effect on the lipids of RBC membrane. Lipid peroxidation products and particularly aldehyde derivatives can inhibit protein synthesis, block macrophage action and cause changes in chemotaxis and enzymatic activity. GSH depletion and subsequent low stores of protein thiol result in both in release from intracellular stores and inhibition of Ca extrusion, producing a marked increase in cytosolic calcium concentration which trigger cytotoxicity [17]. This may be the one of the cause for the increased tendency of the RBC for hemolysis and in turn significant decrease in the hemoglobin levels in the study group. Decreased erythrocyte stability is reflected by the increase in the percent hemolysis. One of the study on osteoarthritis showed that generalized OA are associated with hyperuricemia [18]. However our results remained statistically insignificant.
If oxidative stress and connective tissue hypothesis is correct, then supplementation with oxygen processing enzymes and free radical scavenging molecules should protect connective tissue and the evidence pointing towards a favorable verdict.
References
- Winrow VR, Winyard PG, Morris CJ, Blake DR. Free radicals in inflammation: second messengers and mediators tissue destruction. Br Med Bull 1993; 49: 506-522.
- Chen BX, Francis MG, Duthie RB, Bromey L, Osman O. Oxygen free radical in human Osteoarthritis. Chin Med J 1989; 102: 931-933.
- Henrotin Y, Deby DG, Deby C, Franchimont P, Emerit I. Active oxygen species, articulr inflmmation and cartilage damage. Exs 1992; 62: 308-322.
- Mapp PJ, Grootveld Mc et al. Hypoxia, oxidative stress and rheumatoid arthritis. Br Med Bull 1995; 51: 419-436.
- Deneke SM, Farberg TZ. Regulation of cellular glutathione lung cells. Mol Physiol 1994; 1163-1173.
- Wu D, Meydam SN, Sastre J, Heyek M, Meydani M. In vitro glutathione supplementation enhances IL-2 production and nitrogenic response of peripheral blood mononuclear cells from young and old subjects. J Nutr 1994; 24: 655-663.
- Meister A. Glutathione- Ascorbic acid antioxidant system in animals. J.Biol.Chem. 1994; 269: 9397-9400
- Butler E, Duron O, Kelly BM. Improved method for the determination of blood GSH, J Lab & Clin Med 1963; 61: 883-887.
- Kartha VNR, Krishnamoorthy S. Effect of hypervitaminosis A on hemolysis and lipid peroxidation in the rat. J Lipid Res 1978; 19: 332-334.
- VIth edition, In Gowenlock AH, McMurry RJ, McLauchlan DM. Varley’s Clinical Biochemistry 1988; 664-665.
- Gowenlock AH, McMurry RJ, McLauchlan DM. Varley’s Clinical Biochemistry. 1980; 470-471.
- Lang CA, Narishkin S, Scheider DL, Mills B, Linderman RD. Low blood glutathione in healthy and aging adults. J Lab Clin Med 1992; 120: 720-725.
- Sato M, Miyaziki. Antioxidants inhibits TNF &alpha mediated stimulation of IL-8 monocyte chemo attractant protein and collagenase -expression in cultured human syno-vial fluid. J Rhumatol 1996; 23: 432-438.
- Mustafa G, Fatma ZK, Sadan T, Osmoh H. Cellular and clinical implications of glutathione. Ind J Expt iol 2000; 38: 625-634
- Julius M, Lang CA, Gleiberman L, Harberg E, DiFranceisco W, Schork A. Glutathione and morbidity in a co-mmunity base sample of elderly. J Clin Epidemiol 19-94; 47: 1021-1026.
- Wu D, Meydam SN, Sastre J, Heyek M, Meydani M. In vitro glutathione supplementation enhances IL-2 production and nitrogenic response of peripheral blood mon-onuclear cells from young and old subjects. J Nutr. 19-94; 124: 655-663.
- Bellioma G, Offhenius S. Altered thiol and calcium homeostasis in oxidative hepatocellular injury. Hepa-tology 1985; 5:876-882.
- Al Arfaj A S. Serum uric acid and radiographic osteoarthritis. J Pak Med Assoc 2003; 53: 187-189.