ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 7
Prevalence of prehypertension and associated risk factors in Zhengzhou, middle China: A cross-sectional study
Ya-Nan Ding, Lei Wu, Guo-Ying Geng, Hao-Kun Wang, Zhen-Xuan Hao, Dan-Li Wang, Shu-Ming Bai, Wen-Jie Han and Heng-Liang Liu*
Division of Cardiovascular Medicine, Zhengzhou People’s Hospital, Southern Medical University, Zhengzhou, China
- *Corresponding Author:
- Heng-Liang Liu
Division of Cardiovascular Medicine
Zhengzhou People’s Hospital
Southern Medical University, China
Accepted date: December 3, 2016
The prevalence of hypertension has increased in China, and prehypertension frequently progress to hypertension over a couple of years, both has been public health problems. Therefore a cross-sectional epidemiological survey was conducted in order to determine the prevalence of pre-hypertension and associated risk factors in Zhengzhou, middle of China. A total of 4800 community residents aged 18 year and older from 6 communities were screened by a stratified random cluster sampling method. Baseline characteristics of residents were acquired by questionnaire, physical examination, blood and urine biochemical measurement. Prehypertension was defined according to the Seventh Report of the Joint National Committee (JNC 7) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure guidelines. Multivariate logistic analysis was used to analyse the risk factors of prehypertension. Prevalence of prehypertension was 30.3% in Zhengzhou adult population, and 36.1% in men and 26.0% in women separately. Prevalence of prehypertension was 27.4% in overweight residents, 32.5% in insulin resistance residents, 36.1% in current smoking residents, and increased dramatically with age. Multivariate logistic regression indicated that age, Body Mass Index (BMI), waist circumference, Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) smoking, and brachial-ankle Pulse Wave Velocity (baPWV), were independent risk factors of prehypertension. Prehypertension has been a major public health problem in Zhengzhou, middle China; obesity and insulin resistance have been important risk factors.
Keywords
Prehypertension, Overweight, Homeostatic model assessment of insulin resistance, Risk factor, Crosssectional study.
Introduction
During the past decades, studies indicate that hypertension was a major threat to health, increasing the risk of cardiovascular disease, stroke, renal failure, and visual loss [1-5], and has become an important public-health challenge worldwide [6]. Previous researches reveal that there has different prevalence of hypertension in China according to geographic locations [7-10]. Geographic attributes may be as diverse as physical, socio-demographic, and medical care access of an environment [11,12]. There were substantial geographic variations in the prevalence of hypertension, and geographic variation may lead to geographic risk factors for the prevalence of prehypertension and hypertension [13].
Prehypertension frequently progress to hypertension over a period of 4 years, especially in older adults, in American population by the Framingham Heart Study [14] and in Western European population by Flemish Study on Environment, Genes and Health Outcomes [15]. Prehypertension is also associated with an increased risk of cardiovascular disease, with a risk-factor-adjusted hazard ratio of 2.5 in women and 1.6 in men compared to optimal blood pressure [16]. Prehypertension is very common in the general population. The prevalence of prehypertension in American adults was 40% in men and 23% in women, according to the 1999-2000 National Health and Nutrition Examination Survey [17]. However, there was few studies developed on the epidemiology of prehypertension and associated risk factors in Chinese population, and there was in death of epidemiological data of prehypertension in Zhengzhou. Therefore, we conduct this community based cross-sectional study in order to determine the prevalence of prehypertension and associated risk factors in Zhengzhou adult population.
Materials and Methods
Participants
A community-based survey for prevalence investigation of prehypertension was conducted in Zhengzhou from October 2011 to October 2012. Participants were selected using a stratified random cluster sampling method. Three districts were first selected randomly, and then three further communities were also selected randomly from each district. Finally all residents living in Zhengzhou for at least 5 years from the street blocks and/or villages in each community were selected and invited to participate our survey. Using this method, a total of 4065 participants from 4800 citizens complete the entire survey, with a response rate of 84.6%. All participants were given their written informed consent prior to data collection. Illiterate participants had the information leaflet read out to them and provided a thumb impression. The Human Ethics Committees of Zhengzhou People’s Hospital, Zhengzhou, China, approved the study.
Questionnaire
All clinical doctors, technicians, medical students and nurses participated in the project had received intensive training on proper methods for screening. All participants were asked to fill in the questionnaire under the guidance of well-trained investigators. The questionnaire consists of age, sex, personal and family history of diabetes (yes vs. no), hypertension (yes vs. no), cardiovascular disease (yes vs. no), education (>10 years vs. 6-10 years vs. 1-5 years vs. no), smoking (yes (current) vs. yes (former) vs. no), alcohol intake (>5 times a week vs. 1-4 times a week vs.
Blood and urine sample collection
Appointments were made for urine and blood collection from participants by investigators. Participants were asked to provide the first morning urine, it’s the midstream urine, and no proteases inhibitor was used. Menstrual period in females was avoided. Fasting venous blood drawing was performed at local community clinics or health stations. All urine and blood samples were sent to the central laboratory of Zhengzhou People’s Hospital, Southern Medical University. The blood and urine samples were either disposed within 3 hours or stored at 4°C for not more than two days. The central laboratory had successfully finished a standardization and certification programme.
Blood and urine measurements
Fasting Plasma Glucose (FPG) test was performed, and fasting serum insulin concentration was measured by electrochemical luminescence immunoassay. Serum Total Cholesterol (TC), High-Density Lipoprotein (HDL) cholesterol, Triglycerides (TG), and Low-Density Lipoprotein (LDL) cholesterol were measured by an auto analyser (Toshiba, Japanese). Serum creatinine (Scr) was measured from overnight fasting venous blood samples by Jaffe’s kinetic method. Albuminuria was measured with immuno-turbidimetric tests.
Evaluation criteria
The classification of normotension, prehypertension and hypertension was based on the classification of BP from the JNC-7 [19]. Normotension was defined as not being on antihypertensive medication and having a SBP<120 mmHg and DBP<80 mmHg. Prehypertension was defined as not being on antihypertensive medication and having a SBP of 120-139 mmHg and/or DBP of 80-89 mmHg. Hypertension was defined as SBP ≥ 140 mmHg and/or DBP ≥ 90 mmHg, and also if the individual was on antihypertensive medication. Family history of hypertension was defined as a diagnosis of hypertension in one parent.
Homeostatic Model Assessment of Insulin Resistance (HOMA-IR) was calculated according to the formula: HOMAIR= fasting plasma glucose (mmol/L) × fasting insulin (mU/L)/ 22.5. Upper quartile was considered as cut-off point of Insulin Resistance (IR) according to the recommendation of European Group for the Study of Insulin Resistance [20].
Statistical analysis
Relevant characteristics were described and stratified according to the blood pressure (normotension and prehypertension). Non-normal distributed variables were transformed into normally distributed variables, and then performed analysis. Continuous variables were given as the mean ± SD, and categorical variables as the percentage in each subgroup. Two-sample unequal variance t-test followed by Bonferroni’s correction was used to calculate whether the differences between normotension and prehypertension groups were statistically significant. p<0.05 were considered significant.
A multivariate logistic analysis was used to examine the association of risk factors with the occurrence of prehypertension and normotension, with the method of backward elimination, only co-variables that were significant (p<0.05) were retained in the final model. Covariates included were age, sex, systolic blood pressure, history of diabetes, hypertension, cardiovascular disease, education, smoking, alcohol intake, physical activity, BMI (continuous variable), HOMA-IR (continuous variable), FPG (a continuous variable), albuminuria (continuous variable), plasma cholesterol (a continuous variable), triglyceride (a continuous variable), HDL cholesterol (a continuous variable), LDL cholesterol (a continuous variable), and baPWV (a continuous variable). Epidata software (version 3.1) was used for data entry and management. SPSS13.0 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, and GraphPad Prism 5 was used for mapping.
Results
4065 participants finished the survey, and 42.6% of which was man. The mean age and SD of the subjects in this analysis were 45.0 ± 13.1 years. Of which, 1836 individuals had normal blood pressure, 1233 individuals were prehypertension, and 996 individuals were hypertension. The overall prevalence rate of prehypertension was 30.3%, and hypertension was 24.5%.
The baseline characteristics of the prehypertension and normal tension residents
Table 1 lists the baseline characteristics of the prehypertension and normal tension. Individuals with prehypertension were significantly older (45.5 ± 12.2) than those with normal blood pressure (39.22 ± 11.06). There was 50.8% of male have prehypertension in all 1233 prehypertension residents, and 36.3% of male have normal tension in all 1836 normal tension residents. Maybe, we can reach the conclusion that the overall prevalence of prehypertension was associated with an increase in age, and male seems to have the trend to develop prehypertension. The mean HOMA-IR in prehypertension (1.59 ± 1.46) was significantly higher than that of normal tension (1.09 ± 1.10), and the mean of BMI in prehypertension (23.83 ± 3.21) was also significantly higher over that of normal tension (22.34 ± 2.96). Education status, smoking, drinking, physical activity, family history of hypertension, family history of diabetes, family history of cardiovascular disease, all of them have significant difference between prehypertension and normal tension. Waist circumference, SBP, DBP, albuminuria, serum creatinine, blood glucose, serum insulin, TC, HDL-C, TG, LDL-C, and baPWV, all of them were significantly different between groups.
| Normotension (n=1836) | Prehypertension (n=1233) | P value | |
|---|---|---|---|
| Male (%) | 36.30% | 50.80% | <0.05 |
| Age-year (Mean ± SD) | 39.22 ± 11.06 | 45.45 ± 12.22 | <0.05 |
| High school education and above (%) | 58.20% | 51.00% | <0.05 |
| Current Smoking (%) | 17.50% | 19.80% | <0.05 |
| Habitual drinking (%) | 3.60% | 6.40% | <0.05 |
| Physical activity (%) | 39.70% | 31.20% | <0.05 |
| Family history of hypertension (%) | 22.80% | 24.60% | <0.05 |
| Family history of diabetes (%) | 9.40% | 9.90% | <0.05 |
| Family history of Cardiovascular disease (%) | 7.20% | 8.00% | <0.05 |
| Waist (cm) (Mean ± SD) | 77.34 ± 9.16 | 82.55 ± 9.50 | <0.05 |
| SBP (mmHg) (Mean ± SD) | 104.78 ± 8.11 | 124.67 ± 7.23 | <0.05 |
| DBP (mmHg) (Mean ± SD) | 66.86 ± 5.63 | 77.43 ± 6.33 | <0.05 |
| Albuminuria (mg/l) (Mean ± SD) | 13.18 ± 19.63 | 18.03 ± 38.96 | <0.001 |
| Serum creatinine (mmol/l) (Mean ± SD) | 70.02 ± 49.68 | 77.29 ± 50.23 | <0.05 |
| Glucose (mmol/l) (Mean ± SD) | 4.84 ± 1.09 | 5.07 ± 1.25 | <0.05 |
| Serum insulin (μU/ml) (Mean ± SD) | 5.45 ± 5.03 | 7.53 ± 5.80 | <0.05 |
| TC (mmol/l) (Mean ± SD) | 4.59 ± 1.10 | 4.91 ± 1.23 | <0.05 |
| HDL-C (mmol/l) (Mean ± SD) | 1.42 ± 0.54 | 1.41 ± 0.56 | >0.05 |
| TG (mmol/l) (Mean ± SD) | 1.35 ± 1.23 | 1.68 ± 1.45 | <0.05 |
| LDL-C (mmol/l) (Mean ± SD) | 2.47 ± 0.93 | 2.54 ± 1.00 | <0.05 |
| eGFR (ml/min/1.73 m2 ) (Mean ± SD) | 125.87 ± 20.90 | 116.38 ± 22.34 | <0.05 |
| HOMA-IR (Mean ± SD) | 1.09 ± 1.10 | 1.59 ± 1.46 | <0.05 |
| BMI (kg/ m2) (Mean ± SD) | 22.34 ± 2.96 | 23.83 ± 3.21 | <0.05 |
| baPWV | 1242.03 ± 170.20 | 1502.26 ± 285.31 | <0.05 |
Table 1: Baseline information of participants with normal tension and prehypertension.
Risk factors of prehypertension by multivariate logistic regression
Multivariate logistic regression show that age, BMI, waist circumference, HOMA-IR, smoking, and baPWV were independent risk factors of prehypertension (Table 2). Of which, age increased per 10 years was associated with the increase of prevalence of prehypertension, and there have significant differences. Obesity and overweight both were independent risk factors of prehypertension, according to the recommendation of the Working Group on Obesity in China that is BMI of 18.5 to 23.9 was considered as optimal, 24.0 to 27.9 as overweight, and above 28.0 and including of 28.0 as obesity [21]. Central obesity, considered as an abnormal waist circumference for Chinese males’ ≥ 90 cm and for Chinese females’ ≥ 80 cm [18], was also an independent risk factor with a p value of p<0.05. According to the recommendation of European Group for the Study of Insulin Resistance, 75% cut off point was considered as IR [20], thus IR was an important independent risk factor of prehypertension. We also found current smoking and baPWV were independent risk factors of prehypertension.
| OR | 95% CI | P value | |
|---|---|---|---|
| Sex (ref: female) | 2.663 | 2.113-3.356 | <0.001 |
| Age groups (years): 18-29 | 1.000 (reference) | ||
| 30-39 | 1.355 | 1.050-1.748 | <0.05 |
| 40-49 | 1.798 | 1.381-2.342 | <0.001 |
| 50-59 | 3.723 | 2.670-5.192 | <0.001 |
| 60-69 | 4.376 | 2.769-6.914 | <0.001 |
| 70-79 | 3.776 | 1.920-7.425 | <0.001 |
| BMI (kg/ m2)<23.9 | 1.000 (reference) | <0.001 | |
| 24.0<BMI<27.9 | 1.617 | 1.095-2.388 | <0.001 |
| BMI>28.0 | 2.377 | 1.433-3.944 | <0.001 |
| Waist (ref: male <90 cm, female<80 cm) | 1.25 | 1.011-1.545 | <0.05 |
| HOMA-IR (ref: HOMA-IR<75% cut point) | 1.447 | 1.177-1.780 | <0.001 |
| Current smoking (ref: never smoking) | 0.572 | 0.443-0.739 | <0.001 |
| baPWV | 0.454 | 0.249-0.830 | <0.001 |
Table 2: Risk factors of prehypertension by multivariate logistic regression.
Map analysis of risk factors
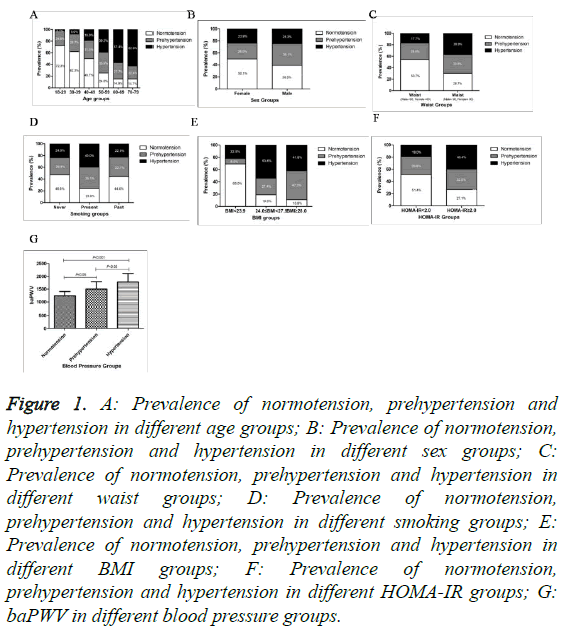
Figure 1A illustrates crude proportions of prehypertension, hypertension and normal tension according to age of all participants. The age-specific prevalence of prehypertension increased with age increased per 10 years, however, the agespecific prevalence of hypertension increased with age increased per 10 years tin 50-59, then decreased. Figure 1B illustrates crude proportions of prehypertension, hypertension and normal tension accounted for all participants by sex. The sex-specific prevalence of prehypertension and hypertension both increased in male population. There were 36.1% of prehypertension and 25.3% of hypertension in male participants. Figure 1C illustrates crude proportions of prehypertension, hypertension and normal tension accounted for all participants by waist circumference. The waist circumference-specific prevalence of prehypertension and hypertension both increased, and there were 33.5% of prehypertension and 36.9% of hypertension in central obesity participants. Figure 1D illustrates crude proportions of prehypertension, hypertension and normal tension accounted for all participants by smoking status. The smoking-specific prevalence of prehypertension increased in present smoking population, and there were 36.1% of prehypertension and 40.0% of hypertension in current smoking participants. The smoking-specific prevalence of prehypertension increased in past smoking population, with the incidence of 33.1%, however the smoking-specific prevalence of hypertension not increased in past smoking participants. Figure 1E illustrates crude proportions of prehypertension, hypertension and normal tension accounted for all participants by BMI. The BMIspecific prevalence of prehypertension and hypertension both increased, and there were 27.4% of prehypertension and 53.6% of hypertension in overweight population; the BMI-specific prevalence of prehypertension and hypertension both increased also in obesity participants, with the incidence of 47.3% of prehypertension and 41.8% of hypertension. Figure 1F illustrates crude proportions of prehypertension, hypertension and normal tension accounted for all participants by HOMAIR. The HOMA-IR-specific prevalence of prehypertension and hypertension both increased, and there were 32.5% of prehypertension and 40.4% of hypertension in IR participants. G reveals baPWV in different blood pressure groups. There were significant difference in baPWV between normal tension and prehypertension groups (p<0.05), between normal tension and hypertension groups (p<0.001).
Figure 1: A: Prevalence of normotension, prehypertension and hypertension in different age groups; B: Prevalence of normotension, prehypertension and hypertension in different sex groups; C: Prevalence of normotension, prehypertension and hypertension in different waist groups; D: Prevalence of normotension, prehypertension and hypertension in different smoking groups; E: Prevalence of normotension, prehypertension and hypertension in different BMI groups; F: Prevalence of normotension, prehypertension and hypertension in different HOMA-IR groups; G: baPWV in different blood pressure groups.
Discussion
In our present study, the prevalence of prehypertension is 30.3% (36.1% in men and 26.0% in women) in Zhengzhou adult population, which was almost the same as the prevalence of 31% (40% in men and 23% in women) in American adults in the 1999-2000 National Health and Nutrition Examination Survey [17], and both indicate that there has sex difference in prevalence of prehypertension. Our result was higher than the prevalence of prehypertension of 28.7% (30.0% in men and 27.2% in women) in five cities of Indian [22], maybe the difference coming from the BP measuring on a single day or day-to-day in our present study.
However our result was lower than the prevalence of 35.87% (37.82% in men and 34.43% in women) in Fujian province [23], 38.89% among a Mongolian population [24], and a research focus on northeast of China during 2009 and 2010 found that the prevalence of prehypertension was 56.9%, men 71.1% and women 44.6%, respectively in adults aged 18-74 years [25]. Our result also lower than prevalence of 40.5% in urban Chinese [26], lower than 35.7% (38.2% in men and 31.8% in women) in Beijing suburban adults [27], lower than 38.6 in Southern China [28], and lower than 44.1% (48.7% in men and 39.6% in women) in rural adults in Liaoning Province [29]. This heterogeneity might be related to differences in study methodology, variability in lifestyles and economic development, or geographic attributes.
Our research also reveals that age was an independent risk factor of prehypertension. In our present study, prevalence of prehypertension was increased with age increased per 10 years until 50-59, then decreased gradually. However, prevalence of hypertension was always increased by age increased per 10 years. Maybe the reason is that with the increase of age, most of prehypertension developed into hypertension finally, especially in old adults [14,15].
Our results also indicate that prevalence of prehypertension was 27.4% in overweight residents, prevalence of prehypertension was 47.3% in obesity participants, and it was 28.6% in non-central obesity participants, 33.5% in central obesity participants. Therefore, overweight, obesity and central obesity were most important independent risk factors of prehypertension. It was already shown in many studies [17,30]. An interesting research by the Coronary Artery Risk Development in Young Adults (CARDIA) study report that young adults who maintained a stable BMI (within 2 kg/ m2 of baseline) at 6 examinations during 15 years had no significant changes in SBP or DBP, whereas those who had an increase in their BMI ≥ 2 kg/ m2 had substantial increases in blood pressure [31]. Obesity, special in abdominal obesity, is also considered a major risk factor for cardiovascular disease by the Framingham Heart Study [32,33].
Most important finding in our study was that HOMI-IR play an important role in occurrence of prehypertension, because that prevalence of prehypertension and hypertension were 32.5% and 40.4% separately in IR participants, and prevalence of prehypertension and hypertension were 29.6% and 19.0% separately in non-insulin resistance participants. Obesity may be a kind of determinant for IR [34,35], and it’s associated with activated and insulin resistant immune cells [36]. Thus, obesity and IR tracked together in prehypertension and cardiovascular disease.
Accumulated evidence indicated that baPWV is an independent predictor of blood pressure progression and incident hypertension [37,38]. BMI was associated with PWV, and abdominal obesity is associated with arterial stiffness determined by pulse wave velocity in middle-aged adults [39]. Visceral adiposity index, a good measure of visceral obesity and significantly increased in prehypertension in our previous study [40], was a positive independent indicator of baPWV [41]. However, baPWV was also significantly increased in prehypertension in our study.
Our study also indicated that current smoking was an independent risk factor of pre-hypertension; there was 36.1% prevalence of prehypertension in current smoking participants and 29.4% prevalence of prehypertension in non-smoking populations. Together with other risk factors of overweight, obesity, central obesity, baPWV and IR, maybe all of these risk factors can attribute to lifestyles [42].
Zhengzhou is a rapidly growing city, as well as a major transportation hub for Central China, which had experienced unequal economic prosperity. More and more people drive cars to work, have no time to do outdoor activities and seldom walk around after dinner. People enjoy spending leisure time on the indoor entertainments such as watching TV, surfing on the internet, and playing games both in rural and urban areas. People usually consume a lot of high calorie or high fat food than in previous times. Young guys tend to smoking addiction, white-collar have no time do physical activity, middle-aged have a lot of social activity such as the Chinese business dinner or banquet, then IR present in old people. A research conducted by the CARDIA study reveal that, weight maintenance than substantial weight loss may be a good strategy for preventing or controlling of hypertension [31]. Therefore, Life style changing and thus induced overweight or obesity and/or insulin resistance were the specific problems in Zhengzhou city residents, which increased the potential of CAD. It’s time to act.
Limitations
The community based cross-sectional epidemiological survey in Zhengzhou had been carried by our study group, and some valuable indications were present, however a large scale prospective research remains to be carried out to further reveal the relationship of risk factors and prehypertension, and the mechanisms through which obesity and IR directly causes hypertension are still an area of research.
Conclusions
Prehypertension has become an important public health problem in Zhengzhou. It’s suggested to develop healthy lifestyles to avoid risk factors of prehypertension.
Acknowledgements
This work was supported by grants from the Diagnosis and Treatment of Atherosclerosis and Related Diseases (No: 096SYJH33114), which was supported by Zhengzhou Municipal Science and Technology Research and Development Commission. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Competing Interests
The authors have declared that no competing interests exist.
Author Contributions
Hengliang Liu design the study, Yanan Ding performed research and wrote the first draft of the manuscript, Lei Wu, Guoying Geng, Haokun Wang, Zhenxuan Hao, Danli Wang, and Shuming Bai, Wen-Jie Han performed research and participated in the statistical analyses. All the authors read and approved the final manuscript.
References
- Chong EW, Lamoureux EL, Jenkins MA, Aung T, Saw SM, Wong TY. Sociodemographic, lifestyle, and medical risk factors for visual impairment in an urban asian population: the singapore malay eye study. Arch Ophthalmol 2009; 127: 1640-1647.
- Lawes CM, Vander Hoorn S, Rodgers A. International Society of Hypertension. Global burden of blood-pressure-related disease, 2001. Lancet 2008; 371: 1513-1518.
- Mannisto T, Mendola P, Vaarasmaki M, Jarvelin MR, Hartikainen AL. Elevated blood pressure in pregnancy and subsequent chronic disease risk. Circulation 2013; 127: 681-690.
- Zoccali C, Mallamaci F, Tripepi G. Hypertension as a cardiovascular risk factor in end-stage renal failure. Curr Hypertens Rep 2002; 4: 381-386.
- Kim MJ, Lim NK, Park HY. Relationship between prehypertension and chronic kidney disease in middle-aged people in Korea: the Korean genome and epidemiology study. BMC Public Health 2012; 12: 960.
- Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK. Global burden of hypertension: analysis of worldwide data. Lancet 2005; 365: 217-223.
- Yongqing Z, Ming W, Jian S, Pengfei L, Xiaoqun P, Meihua D, Peian L, Jianmei D, Guoyu Z, Jie Y, Ping L, Yan X. Prevalence, awareness, treatment and control of hypertension and sodium intake in Jiangsu Province, China: a baseline study in 2014. BMC Public Health 2016; 16: 56.
- Chen L, Zong Y, Wei T, Sheng X, Shen W, Li J, Niu Z, Zhou H, Zhang Y, Yuan Y, Chen Q, Zhong H. Prevalence, awareness, medication, control, and risk factors associated with hypertension in Yi ethnic group aged 50 years and over in rural China: the Yunnan minority eye study. BMC Public Health 2015; 15: 383.
- Fan L, Feng SX, Han B, Wang CC, Gao L. Prevalence, awareness, treatment and control of hypertension in Henan Province, China. Aust J Rural Health 2014; 22: 264-269.
- Zhao Y, Lu F, Sun H, Liu Z, Zhao Y, Sun S, Wang S, Diao Y, Zhang H. Trends in hypertension prevalence, awareness, treatment, and control rates in Shandong Province of China. J Clin Hypertens (Greenwich) 2012; 14: 637-643.
- Wu F, Guo Y, Chatterji S, Zheng Y, Naidoo N, Jiang Y, Biritwum R, Yawson A, Minicuci N, Salinas-Rodriguez A, Manrique-Espinoza B, Maximova T, Peltzer K, Phaswanamafuya N, Snodgrass JJ, Thiele E, Ng N, Kowal P. Common risk factors for chronic non-communicable diseases among older adults in China, Ghana, Mexico, India, Russia and South Africa: the study on global AGEing and adult health (SAGE) wave 1. BMC Public Health 2015; 15: 88.
- Basu S, Millett C. Social epidemiology of hypertension in middle-income countries: determinants of prevalence, diagnosis, treatment, and control in the WHO SAGE study. Hypertension 2013; 62: 18-26.
- Li D, Lv J, Liu F, Liu P, Yang X. Hypertension burden and control in mainland China: Analysis of nationwide data 2003-2012. Int J Cardiol 2015; 184: 637-644.
- Vasan RS, Larson MG, Leip EP, Kannel WB, Levy D. Assessment of frequency of progression to hypertension in non-hypertensive participants in the Framingham Heart Study: a cohort study. Lancet 2001; 358: 1682-1686.
- Zhang H, Thijs L, Kuznetsova T, Fagard RH, Li X, Staessen JA. Progression to hypertension in the non-hypertensive participants in the Flemish Study on Environment, Genes and Health Outcomes. J Hypertens 2006; 24: 1719-1727.
- Vasan RS, Larson MG, Leip EP, Evans JC, ODonnell CJ. Impact of high-normal blood pressure on the risk of cardiovascular disease. N Engl J Med 2001; 345: 1291-1297.
- Wang Y, Wang QJ. The prevalence of prehypertension and hypertension among US adults according to the new joint national committee guidelines: new challenges of the old problem. Arch Intern Med 2004; 164: 2126-34.
- Alberti KG, Zimmet P, Shaw J. Metabolic syndrome-a new world-wide definition. A Consensus Statement from the International Diabetes Federation. Diabet Med 2006; 23: 469-480.
- Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jones DW, Materson BJ, Oparil S, Wright JT, Roccella EJ. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206-1252.
- Balkau B, Charles MA, Drivsholm T, Borch-Johnsen K, Wareham N, Yudkin JS, Morris R, Zavaroni I, van Dam R, Feskins E, Gabriel R, Diet M, Nilsson P, Hedblad B. Frequency of the WHO metabolic syndrome in European cohorts, and an alternative definition of an insulin resistance syndrome. Diabet Metab 2002; 28: 364-376.
- Chen C, Lu FC. The guidelines for prevention and control of overweight and obesity in Chinese adults. Biomed Environ Sci 2004; 17: 1-36.
- Singh RB, Fedacko J, Pella D, Macejova Z, Ghosh S. Prevalence and risk factors for prehypertension and hypertension in five Indian cities. Acta Cardiol 2011; 66: 29-37.
- Lin Y, Lai X, Chen G, Xu Y, Huang B. Prevalence and risk factors associated with prehypertension and hypertension in the Chinese She population. Kidney Blood Press Res 2012; 35: 305-313.
- Li H, Xu T, Tong W, Liu Y, Zhao L, Zhang Y. Comparison of cardiovascular risk factors between prehypertension and hypertension in a Mongolian population, Inner Mongolia, China. Circulation J 2008; 72: 1666-1673.
- Dong GH, Wang D, Liu MM, Liu YQ, Zhao Y, Yang M, Meng XJ, Tian S, Meng X, Zhang HY. Sex difference of the prevalence and risk factors associated with prehypertension among urban Chinese adults from 33 communities of China: the CHPSNE study. J Hypertens 2012; 30: 485-491.
- Meng XJ, Dong GH, Wang D, Liu MM, Liu YQ, Zhao Y, Deng WW, Tian S, Meng X, Zhang HY. Epidemiology of prehypertension and associated risk factors in urban adults from 33 communities in China--the CHPSNE study. Circ J 2012; 76: 900-906.
- Zhang WH, Zhang L, An WF, Ma JL. Prehypertension and clustering of cardiovascular risk factors among adults in suburban Beijing, China. J Epidemiol 2011; 21: 440-446.
- Huang Y, Qiu W, Liu C, Zhu D, Hua J, Cai X, Wu Y, Hu Y, Xu D. Prevalence and risk factors associated with prehypertension in Shunde District, southern China. BMJ Open 2014; 4: e006551.
- Sun Z, Zheng L, Wei Y, Li J, Zhang X, Zhang X, Liu S, Xu C, Li J, Zhao F, Dong G, Hu D, Sun Y. The prevalence of prehypertension and hypertension among rural adults in Liaoning province of China. Clin Cardiol 2007; 30: 183-187.
- Glasser SP, Judd S, Basile J, Lackland D, Halanych J, Cushman M, Prineas R, Howard V, Howard G. Prehypertension, racial prevalence and its association with risk factors: analysis of the reasons for geographic and racial differences in stroke (REGARDS) study. Am J Hypertens 2011; 24: 194-199.
- Lloyd-Jones DM, Liu K, Colangelo LA, Yan LL, Klein L, Loria CM, Lewis CE, Savage P. Consistently stable or decreased body mass index in young adulthood and longitudinal changes in metabolic syndrome components: the coronary artery risk development in young adults study. Circulation 2007; 115: 1004-1011.
- Preis SR, Pencina MJ, Mann DM, DAgostino RB, Savage PJ, Fox CS. Early-adulthood cardiovascular disease risk factor profiles among individuals with and without diabetes in the Framingham heart study. Diabetes Care 2013; 36: 1590-1596.
- Mahabadi AA, Massaro JM, Rosito GA, Levy D, Murabito JM, Wolf PA, ODonnell CJ, Fox CS, Hoffmann U. Association of pericardial fat, intrathoracic fat, and visceral abdominal fat with cardiovascular disease burden: the Framingham Heart Study. Eur Heart J 2009; 30: 850-856.
- Bai XP, Li HL, Yang WY, Xiao JZ, Wang B. Sequence of fat partitioning and its relationship with whole body insulin resistance. Chin Med J (Engl) 2010; 123: 3605-3611.
- Lee JM, Okumura MJ, Davis MM, Herman WH, Gurney JG. Prevalence and determinants of insulin resistance among U.S. adolescents: a population-based study. Diabetes Care 2006; 29: 2427-2432.
- Viardot A, Heilbronn LK, Samocha-Bonet D, Mackay F, Campbell LV, Samaras K. Obesity is associated with activated and insulin resistant immune cells. Diabetes Metab Res Rev 2012; 28: 447-454.
- Zheng X, Jin C, Liu Y, Zhang J, Zhu Y. Arterial stiffness as a predictor of clinical hypertension. J Clin Hypertens (Greenwich) 2015; 17: 582-591.
- Kawada T. Brachial-ankle pulse wave velocity and blood pressure control in treated hypertensive patients. Int J Cardiol 2015; 184: 611.
- Strasser B, Arvandi M, Pasha EP, Haley AP, Stanforth P. Abdominal obesity is associated with arterial stiffness in middle-aged adults. Nutr Metab Cardiovasc Dis 2015; 25: 495-502.
- Ding Y, Gu D, Zhang Y, Han W, Liu H, Qu Q. Significantly increased visceral adiposity index in prehypertension. PLoS One 2015; 10: e0123414.
- Yang F, Wang G, Wang Z, Sun M, Cao M, Zhu Z, Fu Q, Mao J, Shi Y, Yang T. Visceral adiposity index may be a surrogate marker for the assessment of the effects of obesity on arterial stiffness. PLoS One 2014; 9: e104365.
- Gu DF, Shi YL, Chen YM, Liu HM, Ding YN, Liu XY, Li YQ, Shao XF, Liang Y, Chen YS, Yuan ZY, Zou HQ. Prevalence of chronic kidney disease and prediabetes and associated risk factors: a community-based screening in Zhuhai, Southern China. Chin Med J (Engl) 2013; 126: 1213-1219.