ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 10
Minimum effective concentration for the inhibitory effect of remifentanil on circulatory response due to pneumoperitoneum during laparoscopic surgery in elderly patients
Department of Anesthesiology, Beijing Friendship Hospital, Capital Medical University, Beijing, PR China
- *Corresponding Author:
- Ming Tian
Department of Anesthesiology
Beijing Friendship Hospital
Capital Medical University
PR China
Accepted on February 22, 2017
Objective: To find the minimum effective concentration required by remifentanil to inhibit circulatory response due to pneumoperitoneum during laparoscopic surgery in elderly patients.
Methods: ASA grade I/II patients aged 65-80 years old who received elective laparoscopic colon surgery were selected. All patients received Target-Controlled Infusion (TCI) of propofol, with a target plasma concentration of 3.5 μg/ml. They were administrated with 0.9 mg/kg rocuronium after loss of consciousness, inserted with laryngeal mask 2 minutes later and given plasma TCI with remifentanil before the start of surgery to determine its concentration using the sequential method. If mean arterial pressure and/or heart rate of a previous patient increased by >20% within five minutes after pneumoperitoneum compared with before pneumoperitoneum, the current patient was administered with remifentanil at a higher concentration. If the values increased by <20% within five minutes, the current patient was a lower concentration of remifentanil. The target concentration ratio of adjacent effect-site compartments was 1.2. The TCI target plasma concentration (EC50) of remifentanil for inhibiting the hemodynamic fluctuations of 50% of elderly patients after pneumoperitoneum was calculated using the sequential method.
Results: With the sequential method, EC50 of remifentanil for suppressing the hemodynamic response to laparoscopic pneumoperitoneum was 2.67 ng/ml and the 95% confidence interval was 2.61-2.72 ng/ml.
Conclusion: In combination with propofol during TCI, remifentanil at the target plasma concentration of 2.67 ng/ml can inhibit 50% of elderly patients from circulatory fluctuations caused by laparoscopic pneumoperitoneum.
Keywords
Remifentanil, Circulatory response, Pneumoperitoneum, Laparoscopy, Elderly.
Introduction
As one of minimally invasive surgeries, laparoscopic surgery has been widely used in clinical practice, and has become popular owing to small surgical trauma, fast recovery and short hospital stay [1,2]. One of its characteristics is to establish artificial pneumoperitoneum, which requires injection of carbon dioxide gas into the abdominal cavity. After the establishment of pneumoperitoneum, abdominal visceral vessels and inferior caval veins are under pressure, and the backflow of central venous blood increases, i.e. the preload increases, so that the tension of left ventricular wall and the myocardial oxygen consumption increase. Besides, absorption of carbon dioxide into the bloodstream may cause hypercapnia, which can directly inhibit cardiac muscles, dilate peripheral blood vessels, stimulate the central nervous system, and enhance the sympathetic activity and catecholamine release, thus indirectly exciting the cardiovascular system and elevating blood pressure and Heart Rate (HR). Moreover, during laparoscopic operation, it is necessary to change body position to meet the requirements for surgery. For example, the foothigh position is often employed in laparoscopic colon surgery, which can increase the returned blood volume and aggravate circulation disorders. In view of the significant influence of laparoscopic surgery on respiratory circulation, anesthesia should be cautiously managed.
In the past, adverse cardiovascular reactions and autonomic reflex caused by pneumoperitoneum and surgical stress in laparoscopic surgery have been resisted by raising the concentration of inhaled anesthetics, sometimes in combination with fentanyl and muscle relaxants. However, it generally takes over 10 minutes from the increase of concentration of inhaled anesthetics to the onset of clinical effect, which is difficult to cope with cardiovascular reactions occurring at any time during surgery. Increasing the amounts of fentanyl and muscle relaxants may cause accumulation, thereby delaying postoperative recovery and extubation. In recent years, intravenous Target-Controlled Infusion (TCI) has experienced continuous development, which, with the drug concentration in plasma or effect-site compartment as the goal, can quickly reach the depths of anesthesia, analgesia and sedation, so that the concentration of intravenous anesthetics can be adjusted as easily as the adjustment of inhalant vaporizer and the clinical effects can be achieved rapidly. As two novel short-acting intravenous anesthetic drugs, propofol and remifentanil are very suitable for application in TCI, and their combination can significantly enhance the controllability of intraoperative stress response. Remifentanil, as a new μ-receptor agonist containing ester bond, can be rapidly hydrolyzed into inactive metabolites by specific esterase in plasma and tissues, which is typified by short half-life of continuous infusion, no accumulation, metabolism unaffected by hepatic or renal function, strong analgesic effects as well as rapid onset and elimination. There are a number of studies on the optimum concentration of remifentanil for inhibiting stimulation from tracheal intubation and skin incision [3-5], but the effective concentration of remifentanil for suppressing the circulatory response caused by laparoscopic pneumoperitoneum has rarely been investigated. In this study, remifentanil was combined with propofol whose concentration was adjusted under BIS monitoring, which exerted satisfactory anesthetic effects on either intubation or intraoperative maintenance.
Materials and Methods
Baseline clinical data
ASA grade I/II patients aged 65-80 years old who received elective laparoscopic colon surgery between May and August 2015 in our hospital were selected.
Inclusion criteria
ASA grade I/II; 65-80 years old; without history of mental illness; without history of drug abuse or alcoholism; without allergic history of propofol or remifentanil; without liver or kidney dysfunction; Without receiving anesthesia or surgery within one year; without history of cerebrovascular diseases; without history of hypertension or diabetes, or with history of hypertension or diabetes for 5 years or less but regular medication, with blood pressure and sugar levels well controlled (SBP ≤ 160 mmHg, DBP ≤ 95 mmHg, fasting blood sugar level ≤ 7.0 mmol/l).
Exclusion criteria
The Systolic Blood Pressure (SBP) was higher than 180 mmHg and/or the Diastolic Blood Pressure (DBP) was higher than 100 mmHg before administration; SBP was lower than 90 mmHg and/or DBP was lower than 60 mmHg before administration; obesity (BMI>30); ephedrine was used to elevate blood pressure during induction and before surgery.
Materials
Diprifusor TCI Graseby3500 infusion pump using the Marsh pharmacokinetic model and 500 mg 1% W/V propofol injection (batch number: KJ884) were purchased from AstraZeneca (Italy). TCI-I infusion pump using the Minto pharmacokinetic model was bought from Sigo High-tech Development Co., Ltd. (China). A-200XP BIS monitor was obtained from Aspect (USA). Lyophilized remifentanil powders (1 mg/vial, batch number: 6130603) were provided by Yichang Renfu Pharmaceutical Co., Ltd. (China).
Methods
All patients had no premedication. With ECG and BIS monitoring, the veins of upper extremity were opened, and infused with 5 ml/kg hydroxyethyl starch 130/0.4 at an infusion rate of 20 ml.kg-1.h-1 before induction. Intra-arterial pressure was continuously monitored on the ipsilateral upper extremity by radial arterial catheterization, and anesthesia induction was initiated at the same time of mask inhalation of oxygen.
Induction regimen
When the target plasma concentration (TPC) of propofol was 3.5 μg/ml, and the score of Observer’s Assessment of Alertness/Sedation (OAA/S) scale was equal to 1, the patients were administered with 0.9 mg/kg rocuronium and inserted with laryngeal mask 2 minutes later. BIS was continuously monitored to adjust propofol concentration and maintained between 45 and 55. When BIS was lower than 45 for 10 minutes, TPC of propofol was reduced by 0.5 μg/ml. When BIS was higher than 55 for 10 minutes, TPC of propofol was increased by 0.5 μg/ml. When disinfection began, plasma TCI with remifentanil was conducted, and remifentanil at TPC was administered using the sequential method (Minto pharmacokinetic parameters). The current patient’s TPC was determined by the reaction of the previous one. If Mean Arterial Pressure (MAP) and/or HR of the previous patient was increased by >20% within five minutes after pneumoperitoneum compared with baseline, the current patient was applied with a higher concentration. If MAP and/or HR of the previous patient was increased by <20% within five minutes after pneumoperitoneum, the current patient was applied with a lower concentration. The target concentration ratio of adjacent effect-site compartments was 1.2. The laparoscopic pneumoperitoneum pressure was maintained at 12 mmHg. HR, MAP and BIS were recorded respectively before induction of anesthesia, before laryngeal mask insertion, immediately after insertion, before pneumoperitoneum, as well as the first, second, third, fourth and fifth minutes after pneumoperitoneum. In the induction process, if MAP<55 mmHg for 2 minutes, 10 mg ephedrine was given. If the blood pressure was not elevated a minute later, ephedrine was given repeatedly. The case results were used only for analysis. After surgical suture, the patients were given 0.1 μg/kg body weight for analgesia.
Data collection
SBP, DBP, MAP, HR and BIS were recorded in the induction process respectively immediately before administration (T0), at OAA/S scale score of 1 (T1), immediately before insertion of laryngeal mask (T2), immediately after insertion (T3), before pneumoperitoneum (T4), immediately after pneumoperitoneum (T5), as well as the 1st (T6), 2nd (T7), 3rd (T8), 4th (T9) and 5thminutes (T10) after pneumoperitoneum.
Statistical analysis
All data were analysed using SPSS 13.0 software and expressed as mean ± standard deviation (x ± s). Intra-group comparisons were conducted with the paired t-test and variance analysis of randomized block design. The effective number (r) and ineffective number (s) of each remifentanil TPC for inhibition on stress response were collected to calculate the logarithm (x) and total number of cases (n), effective rate of stress response inhibition (p) and difference between two adjacent logarithmic concentrations (d). EC50 and 95% CI were calculated according to the following sequential method [5,6]. Logarithmic value of EC50: IgEC50=Σnx/Σn, and the antilogarithmic value was used to obtain EC50; standard error of EC50: SIgEC50=d√Σ (p (1-p)/n-1). Logarithmic value of 95% CI of overall EC50: (IgEC50-1.96 SIgEC50, lgEC50+1.96SIgEC50). Each anti-logarithmic value was taken to calculate EC50 and its 95% CI. P<0.05 was considered statistically significant.
Results
Baseline clinical data
Two patients underwent obvious blood pressure reduction (MAP<55 mmHg) before remifentanil infusion, who were treated by ephedrine and excluded. Other patients were free from severe stress reaction, bradycardia or hypotension (Table 1).
| Item | Value |
|---|---|
| Age (year) | 71 ± 4 |
| Height (cm) | 165 ± 9 |
| Body weight (kg) | 65 ± 8 |
| Gender (male/female) | 15/10 |
| MAP (mmHg) | 98 ± 9 |
| HR (bpm) | 72 ± 10 |
| BIS | 96 ± 2 |
Table 1. Baseline clinical data (n=25).
Numbering of patients and corresponding plasma remifentanil concentrations
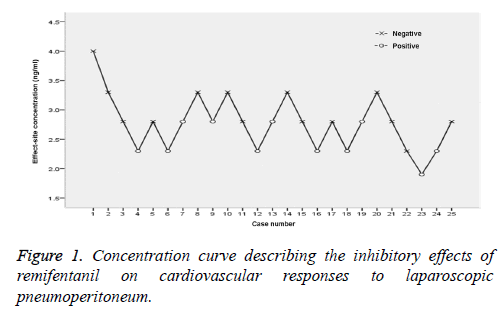
According to the sequential method, all patients were treated with remifentanil at TPC, and the results are shown in Figure 1. For the 25 included patients, the first one received remifentanil TPC of 4 ng/ml, with negative cardiovascular responses. The next patient was treated by the first-level concentration, and the concentration ratio was 1.2. At remifentanil TPC of 2.3 ng/ml, the fourth patient began to suffer from positive responses, and the fifth one was administered with a higher-level concentration. In the calculation of EC50, the concentration for the patient before that having positive responses was used as the initial concentration (i.e. 2.8 ng/ml), so the cases from the 3rd one were included in the equation. Therefore, the concentrations of 23 patients were employed to calculate the inhibitory effects of remifentanil on cardiovascular responses to laparoscopic pneumoperitoneum.
BIS values at different time points
The BIS values at different time points after induction were significantly lower than that before induction (P<0.001), but the results were similar at these time points (Table 2).
| 1 | 2 | 3 | 4 | 5 | |
| BIS | 97.2 ± 0.8* | 48.8 ± 5.0 | 50.5 ± 5.5 | 47.5 ± 4.5 | 49.5 ± 6.0 |
| 6 | 7 | 8 | 9 | 10 | |
| BIS | 48.8 ± 4.9 | 49.6 ± 5.7 | 46.5 ± 4.5 | 48.0 ± 6.5 | 48.3 ± 6.3 |
1: Before induction; 2: before insertion of laryngeal mask; 3: after insertion of laryngeal mask; 4: before pneumoperitoneum; 5: immediately after pneumoperitoneum; 6: 1 minute after pneumoperitoneum; 7: 2 minutes after pneumoperitoneum; 8: 3 minutes after pneumoperitoneum; 9: 4 minutes after pneumoperitoneum; 10: 5 minutes after pneumoperitoneum. *Comparison between BIS values at different time points after induction and that before induction, P<0.001.
Table 2. BIS values at different time points.
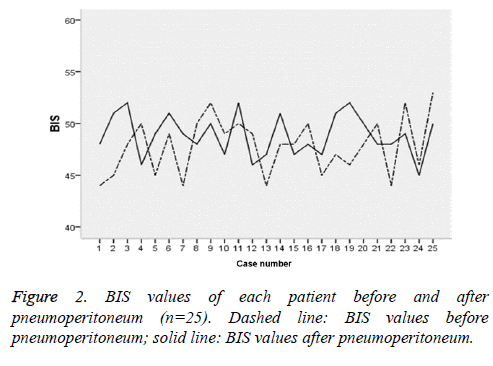
BIS values of each patient before and after pneumoperitoneum
BIS of all patients reached maxima two minutes after pneumoperitoneum (47.5 ± 4.5), which was similar to that before pneumoperitoneum (49.6 ± 5.7) (P=0.377) (Figure 2).
MAP and HR at each time point
MAP and HR, which significantly decreased after induction compared with those before induction (P<0.05), significantly increased after insertion of laryngeal mask compared with those before insertion (P<0.05). The two values were significantly elevated after pneumoperitoneum compared with those before pneumoperitoneum, which were most evident after 1 minute and 2 minutes (P<0.05) (Table 3).
| Time point | MAP (mmHg) | HR (bpm) |
|---|---|---|
| Before induction | 94 ± 9 | 72 ± 10 |
| Before insertion of laryngeal mask | 77 ± 6* | 67 ± 6* |
| After insertion of laryngeal mask | 85 ± 7*△ | 75 ± 7*△ |
| Before pneumoperitoneum | 71 ± 8* | 70 ± 7* |
| Immediately after pneumoperitoneum | 77 ± 10*□ | 69 ± 9*□ |
| 1 minute after pneumoperitoneum | 87 ± 11*□ | 76 ± 10*□ |
| 2 minutes after pneumoperitoneum | 83 ± 8*□ | 71 ± 9*□ |
| 3 minutes after pneumoperitoneum | 79 ± 7*□ | 68 ± 9*□ |
| 4 minutes after pneumoperitoneum | 75 ± 7*□ | 76 ± 6*□ |
| 5 minutes after pneumoperitoneum | 62 ± 7*□ | 65 ± 8*□ |
*Compared with results before induction, P<0.05; △compared with results insertion of laryngeal mask, P<0.05; □compared with results before pneumoperitoneum.
Table 3. MAP and HR at each time point.
Changes of MAP and HR before/after induction/ insertion of laryngeal mask
MAP and HR dropped by 17.1% and 6.9% respectively after induction compared with those before induction, and they rose by 10.4% and 11.9% respectively after insertion of laryngeal mask compared with those before insertion (Table 4). The fluctuations were still clinically acceptable (20%).
| Item | After induction | After insertion of laryngeal mask |
|---|---|---|
| Changing rate of MAP (%) | 17.1 | 10.4 |
| Changing rate of HR (%) | 6.9 | 11.9 |
Table 4. Changes of MAP and HR before/after induction/insertion of laryngeal mask (n=25).
Calculation of EC50 by the sequential method
According to the methods described in the statistical analysis subsection, when BIS was maintained between 45 and 55 for TCI with remifentanil and propofol, EC50 of remifentanil for suppressing the hemodynamic response to laparoscopic pneumoperitoneum was 2.67 ng/ml, and 95% CI was 2.61-2.72 ng/ml (Table 5).
| Concentration (ng/ml) | Logarithm (x) | Effective number (r) | Ineffective number (s) | Total case number (n) | Effective rate (p) | nx |
|---|---|---|---|---|---|---|
| 3.3 | 0.5185 | 4 | 0 | 4 | 1 | 2.074 |
| 2.8 | 0.4472 | 8 | 3 | 11 | 7273 | 4.9192 |
| 2.3 | 0.3617 | 1 | 6 | 7 | 0.1429 | 2.5319 |
| 1.9 | 0.2788 | 0 | 1 | 1 | 0 | 0.2788 |
Table 5. Parameters for calculation of EC50 by the sequential method.
Discussion
In this study, the plasma concentration of remifentanil for inhibiting cardiovascular responses after laparoscopic pneumoperitoneum in 50% of elderly patients was 2.67 ng/ml. In terms of high-positioned epidural anesthesia [6], compared with infusion of remifentanil at a low concentration and constant rate, the infusion of remifentanil at a high concentration (1.0 μg/kg/min) and constant rate can suppress cardiovascular responses induced by pneumoperitoneum. For patients receiving gynecological laparoscopy [7], remifentanil was combined with sevoflurane for intravenous inhalational anesthesia, of which the target concentrations of remifentanil were 2 ng/ml, 4 ng/ml and 6 ng/ml respectively. After pneumoperitoneum, the 4 ng/ml remifentanil group could both maintain stable circulation, and not slow down HR excessively, which was favorable in clinical practice. It is clinically recommended to use 1.5 times to twice of EC50, while 1.5 times of EC50 derived in this study was 4 ng/ml, consistent with the previous results.
BIS is currently considered as an electroencephalogram parameter that can reflect the sleeping stages in the depth of anesthesia and provide continuous real-time monitoring, and compose the mixed information obtained from EEG power and frequency by dual frequency analysis into a parameter value. As BIS contains the EEG quantitative parameters of three kinds of characteristics, i.e. frequency, amplitude and phase, it can reflect all information of EEG signals. Thus, BIS can well reflect the depth of anesthesia, namely the degree of inhibition of anesthetics on the central nervous system and changes in consciousness. As BIS value is more widely applied in monitoring the depth of general anesthesia, its value and significance have received more recognition. Taking into account the pathophysiological characteristics of the elderly, as well as precise anesthesia of today's advocacy, it is particularly important for the application of BIS monitoring in general anesthesia for the elderly. BIS monitoring can reduce the amount of propofol in the induction process of general anesthesia, thereby reducing circulatory fluctuations [8]. The BIS value usually recommended for general anesthesia is 40-65, and 65-85 for sedation [9]. In this study, before administration with muscle relaxants, that is, when OAA/S scale score was<1, BIS was 65 or less, in line with the principle of induced administration, and meanwhile the BIS values during the insertion of laryngeal mask were all<60, showing that the patient was under an effective depth of anesthesia.
In this study, in continuous TCI with propofol, BIS values were decreased with the increase of propofol plasma concentration, and were consistent with the OAA/S scale scores, which was consistent with the results of previous studies [10,11]. It is considered that BIS, propofol blood concentration and OAA/S scale score are correlated, of which BIS has the highest correlation. The BIS values before and after pneumoperitoneum herein were further compared and the results showed no statistically significant differences. The adjustment of remifentanil concentration may not cause changes in BIS values [12]. Also, Albertin et al. [5] found that when patients suffered from noxious stimuli such as tracheal intubation and skin incision, the BIS values did not change significantly, which were consistent with the findings of this study. Hence, analgesia in the induction of general anesthesia cannot be reflected by BIS values. Under anesthesia, some patients do not experience hemodynamic fluctuations during surgery, relying on the effects of opioids, but may have intraoperative awareness due to lack of sedative drugs. In other words, in clinical practice, we cannot just rely on hemodynamic fluctuations to determine the depth of anesthesia, which further reflects the importance of BIS monitoring in general anesthesia.
Conclusion
In summary, this study confirmed that BIS values, remifentanil concentration and hemodynamic fluctuations had no significant correlations, as suggested by the changes of BIS values at each time point of anesthesia induction. When BIS was maintained between 45 and 55 for TCI with remifentanil and propofol, TPC of remifentanil in effect compartment for effective inhibition on circulatory fluctuations after laparoscopic pneumoperitoneum in 50% of elderly patients was determined to be 2.67 ng/ml using the sequential method. Furthermore, the remifentanil concentration for clinical application was recommended to be 4.01 ng/ml, i.e. 1.5 times of EC50, which can be used as a reference for its application in elderly patients for laparoscopic surgery. However, we did not detect the levels of catecholamines, as the limitation of this study. Further studies are on-going in our group.
References
- Fujii S, Ishibe A, Ota M, Yamagishi S, Watanabe K, Watanabe J, Kanazawa A, Ichikawa Y, Oba M, Morita S, Hashiguchi Y, Kunisaki C, Endo I. Short-term results of a randomized study between laparoscopic and open surgery in elderly colorectal cancer patients. Surg Endosc 2014; 28: 466-476.
- Antoniou SA, Antoniou GA, Koch OO, Pointner R, Granderath FA. Laparoscopic colorectal surgery confers lower mortality in the elderly: a systematic review and meta-analysis of 66,483 patients. Surg Endosc 2015; 29: 322-333.
- Wang JF, Xu XP, Yu XY, Li JB, Wu X, Chen JC, Hu XW, Deng XM. Remifentanil requirement for inhibiting responses to tracheal intubation and skin incision is reduced in patients with Parkinsons disease undergoing deep brain stimulator implantation. J Neurosurg Anesthesiol 2016; 28: 303-308.
- Kawaguchi M, Takamatsu I, Masui K, Kazama T. Effect of landiolol on bispectral index and spectral entropy responses to tracheal intubation during propofol anaesthesia. Br J Anaesth 2008; 101: 273-278.
- Albertin A, Casati A, Federica L, Roberto V, Travaglini V, Bergonzi P, Torri G. The effect-site concentration of remifentanil blunting cardiovascular responses to tracheal intubation and skin incision during bispectral index-guided propofol anesthesia. Anesth Analg 2005; 101: 125-130.
- Watanabe K, Kashiwagi K, Kamiyama T, Yamamoto M, Fukunaga M, Inada E, Kamiyama Y. High-dose remifentanil suppresses stress response associated with pneumoperitoneum during laparoscopic colectomy. J Anesth 2014; 28: 334-340.
- Zhou WM. Effect of different concentration remifentanil in clinical anesthesia when hemodynamic. Chinese J Mod Drug Appl 2013; 7: 375-378.
- Gotoda T, Okada H, Hori K, Kawahara Y, Iwamuro M, Abe M, Kono Y, Miura K, Kanzaki H, Kita M, Kawano S, Yamamoto K. Propofol sedation with a target-controlled infusion pump and bispectral index monitoring system in elderly patients during a complex upper endoscopy procedure. Gastrointest Endosc 2016; 83: 756-764.
- Johansen JW, Sebel PS. Development and clinical application of electroen-cephalographic bispectrum monitoring. Anesthesiology 2000; 93: 1336-1344.
- Chen Z, Shao DH, Hang LH. Effects of dexmedetomidine on performance of bispectral index as an indicator of loss of consciousness during propofol administration. Swiss Med Wkly 2013; 143: w13762.
- Deng X, Zhu T. Clinical comparison of propofol-remifentanil TCI with sevoflurane induction/maintenance anesthesia in laparoscopic cholecystectomy. Pak J Med Sci 2014; 30: 1017-1021.
- Yufune S, Takamatsu I, Masui K, Kazama T. Effect of remifentanil on plasma propofol concentration and bispectral index during propofol anaesthesia. Br J Anaesth 2011; 106: 208-214.