ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2017) Volume 28, Issue 12
Miller fisher syndrome associated with serum IgM anti-cardiolipin antibody: A case report
Xueliang Qi*,#, Rui Chen#, Jiaomei Jiang and Ming Zhang
Department of Neurology, the Second Affiliated Hospital of Nanchang University, Nanchang, Jiangxi, P.R. China
#These authors contributed equally to the manuscript
- *Corresponding Author:
- Xueliang Qi
Department of Neurology
The Second Affiliated Hospital of Nanchang University, P.R. China
Accepted on March 31, 2017
Miller Fisher syndrome (MFS) is a variant of Guillain-Barre syndrome (GBS) characterized by acute onset of ophthalmoplegia, ataxia and areflexia. Diplopia, altered ocular motility, pupillary dysfunction and blepharoptosis have been reported in MFS patients. However, the relationship between antiphospholipid antibody and MFS remains largely unclear. Here we report the first Chinese patient with MFS who showed proptosis and pain and had serum anti-GQ1b antibodies and IgM anticardiolipin antibody. A 64-year-old woman presented with numbness of distal limbs, proptosis and pain after upper respiratory tract infection. Her bilateral eye pain got exacerbated, along with blepharoptosis, ophthalmoplegia and horizontal binocular diplopia. Ophthalmological exam revealed normal pressure in both eyes. The neurological examination revealed bilateral ptosis, proptosis with serious tenderness, ophthalmoplegia with dull pupil reaction to light, and areflexia. There was no ataxia. Serum anti-GQ1b antibodies and IgM anti-cardiolipin antibody were positive. Our case suggests that MFS presenting with proptosis and pain may be associated with serum anti-GQ1b antibodies and IgM anti-cardiolipin antibody.
Keywords
Miller fisher syndrome, Proptosis, Anti-cardiolipin antibody, GQ1b antibody, Chinese.
Introduction
Miller Fisher syndrome (MFS) is a variant of Guillain-Barre syndrome (GBS) characterized by acute onset of ophthalmoplegia, ataxia and areflexia, and positive serum anti- GQ1b antibodies. MFS is difficult to be diagnosed due to varied clinical manifestations [1]. Diplopia, altered ocular motility, pupillary dysfunction, blepharoptosis have been reported in MFS patients. However, seldom case report has been reported for MFS patients presenting with proptosis and pain. Previous observations provide strong but still inconclusive evidence that autoantibodies play an important pathogenic role in GBS. Anti-ganglioside antibodies including GM1a, GM1b, GD1a, GalNAc-GD1a, GD1b, GD3, GT1a and GQ1b antibodies have been studied intensively, and anti-GQ1b antibody is considered as a specific antibody for MFS [2].
Anti-cardiolipin antibodies are implicated in the pathogenesis of thrombotic diseases and systemic lupus erythematosus (SLE) [3]. Moreover, antiphospholipid antibodies were found in some GBS patients [4,5]. However, the relationship between antiphospholipid antibody and MFS remains largely unclear. Ishida et al. described a Japanese MFS patient with low titer of serum anti-GQ1b antibodies and increased IgG anti-cardiolipin antibody [6]. Here we report the first Chinese patient with MFS who showed proptosis and pain and had serum anti- GQ1b antibodies and IgM anti-cardiolipin antibody.
Case Report
A 64-year-old Chinese woman, without any significant medical history, presented with four-day numbness of distal limbs, three-day proptosis and pain after upper respiratory tract infection. She was afebrile and recovered from a mild cough without any drug therapy. Her numbness of limbs got better but bilateral pain got exacerbated when she lay down, accompanied by proptosis, blepharoptosis, ophthalmoplegia, horizontal binocular diplopia. Ophthalmological exam revealed normal pressure in both eyes. The general physical examination showed pharyngeal hyperemia and tonsils II° swelling, while neurological examination revealed bilateral ptosis, proptosis with serious tenderness, and ophthalmoplegia with dull pupil reaction to light. Examination of the rest of cranial nerves was negative and symmetrical. Muscle strength and sensation of four limbs were normal. There was no ataxia. Tendon hyporeflexia in both the upper and lower extremities were observed, and the bilateral Babinski sign was negative.
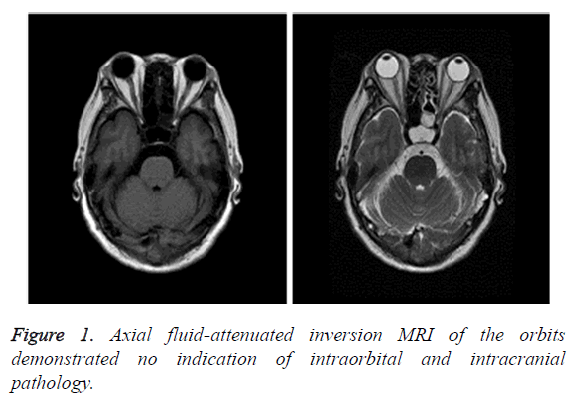
On admission, laboratory examinations showed that blood routine, urinalysis and feces tests were normal. The results of biochemistry tests, including electrolytes, liver and kidney function tests, hemoglobin A1c, coagulation function, thyroid function, cobalamine, folic acid, tumor marker screen test, test for infectious etiologies, and C-reactive protein were within normal ranges. Lumbar puncture showed opening pressure of 17 cm, leukocytes 2/mm3, elevated protein level 801.81 mg/L and normal glucose level. Tumor cell, bacterial, viral and fungal testing of cerebrospinal fluid (CSF) were negative. Serum IgG against GQ1b was detected but GQ1b antibody was not detected in CSF. Additional examinations showed that anti-nuclear antibody, extractable nuclear antigen and anti-neutrophil cytoplasmic antibodies were negative, but serum IgM anti-phospholipid antibody was positive. Magnetic resonance imaging (MRI) and magnetic resonance angiography of the brain showed unremarkable changes, other than nonspecific white matters (Figure 1). Electromyography and nerve conduction analysis showed normal results.
The diagnosis of MFS was made based on clinical findings. The patient was treated with synchronous intravenous immunoglobulin at 25 g/day and methylprednisolone at 500 mg/day for 5 days, then treated with methylprednisolone at 250 mg/day for 3 days and at 120 mg/day for another 3 days, and then treated with oral prednisolone 60 mg/day. On the tenth day, her pain and proptosis improved obviously, and ophthalmoplegia improved mildly. Numbness of distal limbs become better and deep tendon reflexes returned. A gradual dosage reduction for oral prednisolone was performed. When the patient stopped oral prednisolone 3 months later, she recovered completely and all clinical symptoms disappeared.
Discussion
Most MFS patients have a preceding infection history, and the typical symptoms include ophthalmoplegia, ataxia and areflexia, while some patients may have paresthesia, weakness and multiple cranial nerve lesions [7]. A review of 223 cases of MFS showed that the incidence of diplopia was 38.6%, the incidence of ataxia was 20.6% and the incidence of areflexia was 81.6%, and cranial nerves involvement was present in 56.9% of MFS patients [8]. In this patient, the diagnosis of MFS was supported by paresthesia in limbs endings as the first symptom, ophthalmoplegia and areflexia, CSF albuminocytological dissociation and positive serum anti- GQ1b antibodies. Different from typical MFS patients, this patient presented with pain and proptosis which to our knowledge rarely have been reported in the literature. Waung et al. report a case of MFS similar to ours, and suggested that idiopathic thin extraocular muscles may lead to the development of proptosis when ophthalmoplegia and oculomotor nerve dysfunction make globe position laxity [9].
To the best of our knowledge, autoimmune-mediated demyelinating is primary pathogenesis of MFS. It has been reported that 90% of patients with MFS have IgG antibodies against GQ1b and anti-GQ1b antibody is considered to be a specific marker of MFS, but some patients are negative for this antibody [10,11]. It is postulated that anti-GQ1b antibodies generate after the infection of the pathogens and they attack ganglioside GQ1b to cause clinical symptoms [12,13].
Most striking, this patient was positive for serum IgM anti-cardiolipin antibody. Ishida et al. described a MFS case with low titer of serum anti-GQ1b antibodies and increased IgG anti-cardiolipin antibody [2]. The relationship between antiphospholipid antibody and MFS has not been noticed previously. Anti-cardiolipin IgM antibody may promote early stage of the disease. Alternatively, as anti-cardiolipin antibodies have been shown to alter prostanoid synthesis in endothelial cells [14], and prostanoids are synthesized in peripheral nerves [15], anti-cardiolipin antibodies could cause functional nerve impairment.
It is not well understood whether anti-cardiolipin antibodies play a role in the pathogenesis of the polyneuropathy or represent a part of an extensive immunoreaction that occurs in MFS. The immune attack is directed against the components of Schwann cell membrane and is accompanied by the characteristic feature of vesicular demyelination [16]. Anti-cardiolipin and anti-phosphatidylinositol antibodies could be useful markers for the response of MFS patients to treatment. Unfortunately, re-examination of autoimmune function was declined by the patient.
In conclusion, we report the first case of Chinese MFS patient presenting with proptosis and pain associated with both serum anti-GQ1b antibodies and IgM anti-cardiolipin antibody. The clinician should pay attention to anti-cardiolipin antibodies associated with atypcial clinical presentations of MFS.
References
- Lo YL. Clinical and immunological spectrum of the Miller Fisher syndrome. Muscle Nerve 2007; 36: 615-627.
- van den Berg B, Walgaard C, Drenthen J, Fokke C, Jacobs BC, van Doorn PA. Guillain-Barré syndrome: pathogenesis, diagnosis, treatment and prognosis. Nat Rev Neurol 2014; 10: 469-482.
- Harris EN, Gharavi AE, Hughes GR. Anti-phospholipid antibodies. Clin Rheum Dis 1985; 11: 591-609.
- Frampton G, Winer JB, Cameron JS, Hughes RA. Severe Guillain-Barré syndrome: an association with IgA anti-cardiolipin antibody in a series of 92 patients. J Neuroimmunol 1988; 19: 133-139.
- Nakos G, Tziakou E, Maneta-Peyret L, Nassis C, Lekka ME. Anti-phospholipid antibodies in serum from patients with Guillain-Barré syndrome. Intensive Care Med 2005; 31: 1401-1408.
- Ishida S, Ura M, Kameoka K, Furukawa K, Tagami M. A case of atypical Miller Fisher syndrome associated with antiphospholipid antibodies. Rinsho Shinkeigaku 1999; 39: 448-451.
- Hall DJ, Bazaraa T. A rare case of complete bilateral ophthalmoplegia and ptosis. Age Ageing 2014; 43: 145-147.
- Berlit P, Rakicky J. The Miller Fisher syndrome. Review of the literature. J Clin Neuroophthalmol 1992; 12: 57-63.
- Waung MW, Singer MA. An unusual case of Miller Fisher syndrome presenting with proptosis and chemosis. Muscle Nerve 2012; 45: 764-766.
- Kim KW, Kim YH, Kim BH, Lee CY, Oh MS, Yu KH, Lee BC. Miller Fisher syndrome related to Orientia tsutsugamushi infection. J Clin Neurosci 2014; 21: 2251-2252.
- Yis U, Bayram E, Topcu Y, Karakaya P, Hiz Kurul S. A case of atypical Miller Fisher syndrome with negative anti-GQ1b immunoglobulin G and importance of H reflex. Turk J Pediatr 2013; 55: 235-236.
- Yuki N, Hartung HP. Guillain-Barré syndrome. N Engl J Med 2012; 366: 2294-2304.
- Fokke C, van den Berg B, Drenthen J, Walgaard C, van Doorn PA, Jacobs BC. Diagnosis of Guillain-Barré syndrome and validation of Brighton criteria. Brain 2014; 137: 33-43.
- Carreras LO, Defreyn G, Machin SJ, Vermylen J, Deman R, Spitz B, Van Assche A. Arterial thrombosis, intrauterine death and 'lupus anticoagulant': detection of immunoglobulin interfering with prostacyclin production. Lancet 1981; 1: 244-246.
- Goswami SK, Gould RM. Prostanoid synthesis in peripheral nerve. Biochim Biophys Acta 1985; 834: 263-266.
- Hafer-Macko CE, Sheikh KA, Li CY, Ho TW, Cornblath DR, McKhann GM, Asbury AK, Griffin JW. Immune attack on the Schwann cell surface in acute inflammatory demyelinating polyneuropathy. Ann Neurol 1996; 39: 625-635.