ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2016) Volume 27, Issue 3
Is there a relationship between mean platelet volume and the severity of coronary ectasia?
Department of Cardiology, Faculty of Medicine, Mevlana University, Konya, Turkey
Accepted Date: March 15, 2016
Mean platelet volume (MPV) is an indicator of platelet activation that is elevated in patients with coronary artery ectasia (CAE). We aimed to research relationship between MPV and the severity of coronary ectasia. The reports of 6,377 patients who underwent elective coronary angiography screening between January 2011 and January 2015 were reviewed. After exclusion, 117 patients with isolated CAE were included in this study. The severity of CAE was divided into four types according to the Markis classification. There was no significant difference in age, sex, hypertension, diabetes mellitus, smoking, or family history between the CAE and normal angiogram groups (P>0.05). MPV was significantly higher in patients with CAE than the control group (11.14 ± 1.13 vs. 9.82 ± 0.90 fL, P<0.001). MPV was significantly higher in Markis type 1 than in type 2, and in type 2 than in type 4 (both P<0.001). In the multiple logistic regression analysis, MPV (OR=3.555, 95% CI 2.282–5.538, P<0.01) and red blood cell distribution width (RDW) (OR=2.393, 95% CI 1.573–3.639, P<0.01) were identified as independent predictors of CAE. The MPV cutoff value was found to be 10.85 femtoliters (fL) (82.1% sensitivity, 81.8% specificity). MPV and RDW are both increased in CAE. MPV and RDW are positively correlated with each other. An increased MPV is associated with the severity of CAE. MPV values >10.85 fL may indicate the presence of CAE.
Keywords
Mean platelet volume, Coronary artery ectasia, Red blood cell distribution width, Markis, Hematological indices, Blood count.
Abbreviations
MPV: Mean Platelet Volume, CAE: Coronary Artery Ectasia, RDW: Red Blood cell distribution Width, fL: femtoliters BMI: Body Mass Index, AST: Aspartate Amino Transferase ALT: Alanine amino Transferase WBC: White Blood Cell, RBC:Red Blood Cell, LMCA: Left Main Coronary Artery, LAD: Left Anterior Descending artery, LCx: Left Circumflex artery, RCA: Right Coronary Artery, MACE: Major Adverse Cardiovascular Events SD: Standard Deviation OR: Odds Ration; CI: Confidence Interval.
Introduction
Coronary artery ectasia (CAE) is defined as dilatation of segment of a coronary artery exceeding the diameter of contiguous segments or the diameter of the largest coronary artery more than 1.5 times [1]. In angiographic series, the reported incidence of CAE ranges from 1.5 to 5% [2]. The pathogenesis of CAE is not clear, although connective tissue diseases are congenital causes of CAE. Acquired causes of CAE include atheromatous disease, arteritis (Kawasaki disease, syphilis, and Takayasu’s arteritis), trauma or dissection, and complications of coronary intervention [3,4]. CAE is observed most frequently in the right coronary artery (RCA), and occurs less frequently in the left main coronary artery (LMCA). Atherosclerosis is the main cause of CAE in adults [1]. The most serious consequence of CAE is thrombus formation with distal embolization, vasospasm, or vessel disruption at the site of wall injury [4].
The mean platelet volume (MPV) is the average volume (size) of a patient’s platelets and is an indicator of platelet activation. Platelet activation plays an important role in the pathogenesis of atheromatous diseases [5]. Platelets with a large volume have a higher thrombotic potential [6]. An increased MPV is an independent predictor of a large intracoronary thrombus burden in acute myocardial infarction and the severity of coronary artery disease [7,8].
Isolated CAE is defined as CAE without significant coronary artery disease [9]. Several studies have shown that an increased MPV is associated with the presence and prognosis of CAE [10-12]. In this study, we investigated the relationship between the severity of isolated CAE and MPV in patients who underwent elective coronary angiography for suspected coronary artery disease.
Materials and Methods
Patients and procedure
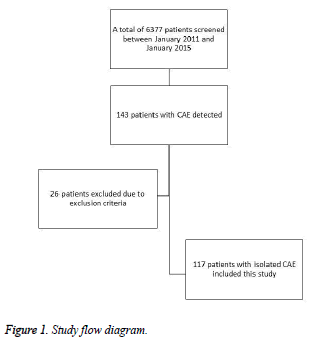
This study examined the reports of 6,377 consecutive patients who underwent elective angiography for diagnosing coronary artery disease between January 2011 and January 2015 at Mevlana (Rumi) University Private Hospital, a tertiary cardiac center. Of the 6,377 patients, 143 were diagnosed with CAE. Patients with any of following were excluded: significant coronary artery disease, an ejection fraction less than 40%, valvular heart disease, hemodialysis for chronic renal failure, malignancy, active bleeding, or anemia. Ultimately, 117 patients with isolated CAE and 70 sex- and age-matched patients with normal coronary angiograms were enrolled in this cross-sectional study (Figure 1). Angiographic images of patients with CAE observed by two experienced interventional cardiologists and determined the severity of CAE by consensus according to the Markis classification [13] (Table 2).
On admission and before coronary angiography, blood samples were taken from all patients for laboratory analysis in standard tubes containing ethylenediaminetetraacetic acid (EDTA). All samples were analyzed on a Sysmex K-X-21N auto-analyzer. The following biochemical parameters were analyzed with a Siemens ADVIA 2400 instrument (Tarrytown, NY, USA): fasting glucose (70–105 mg/dL), urea (10–50 mg/dL), creatinine (0.50–1.2 mg/dL), uric acid (3.4–7.0 mg/dL), aspartate transaminase (AST; 0–38 U/L), and alanine aminotransferase (ALT; 0–41 U/L). Transthoracic echocardiography was performed on all patients on admission using a System V (GE Vingmed; Horten, Norway). The left ventricular ejection fraction was measured using the modified Simpson’s rule [14].
Experienced cardiologists performed the coronary angiography using a standard technique with a Siemens Axiom Artis dBA catheterization system (Siemens Healthcare, Forchheim, Germany). Patient characteristics, height, and weight, and cardiovascular risk factors were obtained from angiography reports and medical records. Body mass index (BMI) was calculated by dividing the patient’s weight in kilograms by the square of height in meters (kg/m2).
The diagnosis of diabetes was based on a history of diabetes with or without drug therapy. Hypertension was based on a history of hypertension with or without treatment. Hyperlipidemia was defined as a total cholesterol ≥ 200 mg/dL, low-density lipoprotein (LDL)-cholesterol >130 mg/dL, or triglycerides >150 mg/dL, or a history of using lipid-lowering drugs. Current smokers and those who smoked until the past month were classified as smokers. From the coronary angiography results, significant coronary artery stenosis was defined more than 50% stenosis in the coronary arteries. A positive family history of coronary artery disease was based on evidence such as a history of myocardial infarction or sudden cardiac death in first degree relatives before 60 years of age. The study protocol was approved by the university ethics committee.
Statistical analysis
Continuous variables are given as the median ± SD, and categorical variables are defined as percentages. Student t-test or Mann-Whitney U test was used to compare continuous variables. Categorical variables were compared with the chisquare test. The data in the four groups were compared with one-way ANOVA followed by the Tukey HSD test for multiple comparisons. Significant variables (p<0.05) were included in a multivariate model. Values of p<0.05 were considered to indicate significance. A cutoff point for MPV, RDW and MPVRDW multiply to predict the severity of CAE was calculated with a receiver operating characteristics (ROC) curve analysis and is expressed as the area under the curve (AUC) and sensitive-specific values with95% confidence intervals (CIs). Statistical significance was defined as p <0.05. The SPSS for Windows ver. 16.0 statistical software (SPSS Inc, Chicago, IL, USA) was used for all statistical calculations.
Results
Table 1 summarizes the baseline characteristics and laboratory parameters of 117 patients with CAE and 70 age- and sexmatched patients with normal coronary angiograms. The baseline age, sex, diabetes mellitus, hypertension, smoking, hyperlipidemia, and family history were statistically similar in the CAE and normal groups, as were glucose, blood urea nitrogen, creatinine, AST, ALT, white blood cell count, hemoglobin (Hb), hematocrit, red blood cell count, and platelet count. The MPV and red blood cell distribution width (RDW) were significantly higher in the CAE group than the normal coronary artery group (both P<0.001).
| Variables | Ectasia (n=117) | Normal (n=70) | P values |
|---|---|---|---|
| Age | 64.32±10.42 | 65.39±10.46 | 0.502 |
| Sex n (%) | |||
| Male | 50 (42.7) | 31 (44.3) | 0.836 |
| Female | 67 (57.3) | 39 (55.7) | 0.956 |
| Diabetes mellitus n (%) | 35 (29.9) | 19 (27.1) | 0.741 |
| Hypertension n (%) | 83 (70.9) | 43 (61.4) | 0.119 |
| Hyperlipidemia n (%) | 42 (35.9) | 26 (37.1) | 0.410 |
| Smoking n (%) | 31 (26.5) | 10 (14.3) | 0.670 |
| Family History n (%) | 37 (31.6) | 17 (24.3) | 0.320 |
| BMI (kg/m2) | 25.8±2.6 | 25.6±2.5 | 0.770 |
| Glucose (mg/dl) | 117.09±44.53 | 115.20±41.22 | 0.773 |
| Urea (mg/dl) | 19.18±9.11 | 19.37±10.86 | 0.889 |
| Creatinine (mg/dl) | 0.83±0.33 | 0.80±0.38 | 0.713 |
| AST (U/L) | 24.38±29.82 | 26.98±40.17 | 0.632 |
| ALT (U/L) | 22.11±14.45 | 23.72±18.22 | 0.520 |
| WBC (x103) | 8.06±2.17 | 7.91±2.18 | 0.660 |
| Hemoglobin (g/dl) | 14.07±1.58 | 14.24±1.48 | 0.479 |
| Hematocrit (%) | 42.37±4.31 | 42.42±3.98 | 0.937 |
| RBC (x106) | 4.88±0.58 | 4.86±0.51 | 0.839 |
| Platelet (x103) | 233.18±63.91 | 236.86±66.54 | 0.709 |
| MPV (fL) | 11.14±1.13 | 9.82±0.90 | <0.001 |
| RDW (%) | 15.02±1.89 | 13.41±0.72 | <0.001 |
| BMI: body mass index, Family history: for coronary artery disease, AST: aspartate amino transferase ALT: alanine amino transferase WBC: White blood cell, RBC: Red blood cell, MPV: Mean platelet volume, RDW: Red cell distribution width, SD, standard deviation, Bolded data indicate significance | |||
Table 1: Baseline characteristics and laboratory parameters of patients with coronary artery ectasia and normal coronary angiograms.
After classifying the patients with CAE into four types according to the Markis classification, there were 48 (41%), 39 (33.3%), 6 (5.1%), and 24 (20.55%) patients with types 1 to 4, respectively (Table 2). The CAE most frequently involved the RCA (80 patients, 68.4%), and CAE affected two vessels in 50.4% of patients (Table 3).
| Markis classification | n (%) | |
|---|---|---|
| Type 1 | Diffuse ectasia of two or three vessels | 48 (41) |
| Type 2 | Diffuse ectasia in one vessel and localized disease in another | 39 (33.3) |
| Type 3 | Diffuse ectasia in one vessel only | 6 (5.1) |
| Type 4 | Localized or segmental involvement | 24 (20.5) |
Table 2: Classification of the severity of coronary ectasia.
| Number of ectasic vessels n% | ||
|---|---|---|
| 1 vessel | 30 | 25.6 |
| 2 vessels | 59 | 50.4 |
| 3 vessels | 28 | 23.9 |
| Distribution of ectasic vesselsn % | ||
| LMCA | 49 | 41.9 |
| LAD | 68 | 58.1 |
| LCx | 51 | 43.6 |
| RCA | 80 | 68.4 |
| LMCA: Left main coronary artery, LAD: Left anterior descending artery, LCx: left circumflex artery, RCA right coronary artery. | ||
Table 3: Number and distribution of coronary vessels with ectasia.
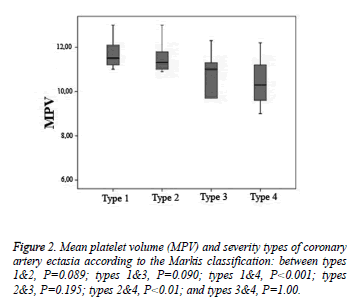
The MPV was similar in Markis types 1 and 2 (P=0.089), types 1 and 3 (P=0.09), types 2 and 3 (P=0.195), and types 3 and 4 (P=1.0).The MPV was significantly higher in type 1 than in type 4 and in type 2 than in type 4 (both P<0.001) (Figure 2).
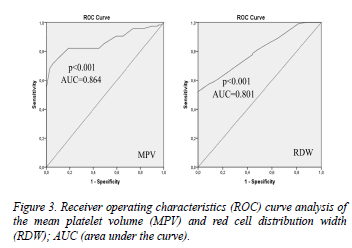
In the multiple logistic regression analysis, MPV (OR=3.555, 95% CI 2.282–5.538, P<0.01) and RDW (OR=2.393, 95% CI 1.573–3.639, P<0.01) were identified as independent predictors of CAE (Table 4). Receiver operating characteristic (ROC) curve analyses were performed for MPV and RDW. The MPV cutoff value was 10.85 fL (AUC=0.864, P<0.001, 95% CI 0.812–0.916, 82.1% sensitivity, 81.8% specificity). The RDW cutoff value was 13.85 (AUC=0.800, P<0.001, 95% CI 0.739–0.861, 69.2% sensitivity, 69.6% specificity) (Figure 3). There was a strong, significant positive correlation between MPV and RDW (r=0.282, P<0.01).
| Variables | Multivariate Analysis | ||
|---|---|---|---|
| OR | %95 CI | P value | |
| Hypertension | 2.577 | 0.996-6.668 | 0.51 |
| Smoking | 3.584 | 1.171-10.973 | 0.24 |
| MPV | 3.555 | 2.282-5.538 | <0.01 |
| RDW | 2.393 | 1.573-3.639 | <0.01 |
| MPV, Mean platelet volume; RDW, Red blood cell distribution width; OR, odds ration; CI, confidence interval. | |||
Table 4: Independent predictors of coronary artery ectasia in the multivariate logistic regression analysis.
Discussion
Platelets play important role in the pathophysiology of thrombogenesis and arteriogenesis. The MPV is the volume of the average circulating platelet in femtoliters and reflects platelet function and activation [15]. An increased MPV is related both metabolically and enzymatically to more active platelets, which have a greater effect on homeostasis than smaller platelets [16]. Numerous recent studies have assessed the association between MPV and coronary artery disease. There is an association between acute coronary syndromes and MPV [17], and an increased MPV is associated with a poor prognosis in acute thrombotic events [18, 19]. Atheromatous diseases and cardiovascular risk factors also frequently accompany CAE [9]. Several studies have demonstrated a relationship between MPV and CEA [10-12].
In our present study, we investigated the relationship between MPV and the severity of CAE. MPV was significantly higher in the CAE group than in the normal angiogram group. In addition, MPV was significantly higher in diffuse ectasia (Markis type 1) than in localized ectasia (type 4). In our study, CAE frequently affected more than one vessel, and the RCA was affected more often than other coronary arteries. In parallel to our study, Demir et al. stated that MPV increases with atherosclerotic process and severity of CAE [11]. They also wrote that cardiovascular risk factors such as diabetes, hypertension, obesity, and smoking were associated with an increased MPV. In our study, we compared patients with similar baseline characteristics and without significant coronary artery disease. Interestingly, the largest study on CAE by Sarlı et al. found no relationship between MPV and coronary ectasia. Those authors divided their patients into four groups: patients with CAE, patients with CAE and coronary artery disease, patients with only coronary artery disease, and patients with normal angiograms. They emphasized that MPV increased with coronary artery disease rather than CAE [20]. However, the main limitation of their study was that they did not classify the severity of CAE, although they wrote that their CAE group patients had less severe, focal CAE.
Varol et al. evaluated the prognostic value of MPV in patients with CAE and followed 258 patients for major adverse cardiovascular events (MACE) for 49 ± 21 months. They found that MPV had prognostic value for MACE in patients with CAE, and that the rate of MACE was higher in CAE patients with a MPV >9 fL [21]. The RDW indicates increased variability in red blood cell size, which is also called anisocytosis. RDW is typically used in the differential diagnosis of anemia. Many studies have reported a relationship between RDW and the presence and severity of CAE [22,23]. We also found that RDW was significantly higher in the CAE group (P<0.01). In the multivariate analysis, we found a positive correlation between MPV and RDW. However, MPV was a stronger predictor of CAE than RDW (OR=3.555 and 2.393, respectively). A MPV >10.85 fL predicted CAE with 82.1% sensitivity and 81.8% specificity.
The main limitation of this study was its retrospective nature and that no clinical follow-up data were recorded. Second, in patients with isolated CAE, we ruled out significant coronary artery disease with coronary angiography and determined the stenosis degree by eye. The use of the fractional flow reserve and intravascular ultrasonography would probably be beneficial for ruling out significant CAD. In conclusion, our study demonstrates that both MPV and RDW are increased in CAE. MPV and RDW are positively correlated. An increased MPV is associated with the severity of CAE. A MPV >10.85 fL may indicate the presence and severity of CAE. Increased MPV may indicate the need of more aggressive antiplatelet therapy in patients with CAE.
Acknowledgements
We thank the staff in the Hospital Catheter Laboratory (Halit Unal, Yahya Imran Kara, Osman Tasoluk, Salih Uyanik, and Fahrettin Karbeyaz) for their support
References
- Syed M, Lesch M. Coronary artery aneurysm: a review. ProgCardiovasc Dis. 1997; 40: 77-84.
- Boles U, Eriksson P, Zhao Y, Henein MY. Coronary artery ectasia: remains a clinical dilemma. Coron Artery Dis. 2010; 21: 318-320.
- Liu R, Gao F, Huo J, Yi Q. Study on the relationship between mean platelet volume and platelet distribution width with coronary artery lesion in children with Kawasaki disease. Platelets. 2012; 23: 11-16.
- Gziut AI, Gil RJ. Coronary aneurysms. Pol Arch Med Wewn. 2008; 118: 741-746.
- Sansanayudh N, Anothaisintawee T, Muntham D, McEvoy M, Attia J, Thakkinstian A. Mean platelet volume and coronary artery disease: a systematic review and meta-analysis. Int J Cardiol. 2014; 175: 433-440.
- Gasparyan AY, Ayvazyan L, Mikhailidis DP, Kitas GD. Mean platelet volume: a link between thrombosis and inflammation? Curr Pharm Des. 2011; 17: 47-58.
- Lai HM, Xu R, Yang YN, Ma YT, Li XM, Zhao Q, Chen QJ, Zhai H, Liu F, Chen BD. Association of mean platelet volume with angiographic thrombus burden and short-term mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Catheter CardiovascInterv. 2015; 85: 724-733.
- Akin F, Ayca B, Kose N, Altun I, Avsar M, Celik O, Satilmis S, Eksik A, Okuyan E. Relation of platelet indices to severity of coronary artery disease in patients undergoing primar y percutaneous coronary intervention. Perfusion. 2015; 31: 216-222
- Swaye PS, Fisher LD, Litwin P, Vignola PA, Judkins MP, Kemp HG, Mudd JG, Gosselin AJ. Aneurysmal coronary artery disease. Circulation. 1983; 67: 134-138.
- Bitigen A, Tanalp AC, Elonu OH, Karavelioglu Y, Ozdemir N. Mean platelet volume in patients with isolated coronary artery ectasia. J Thromb Thrombolysis. 2007; 24: 99-103.
- Demir S, Avsar MK, Karakaya Z, Selcuk M, Tosu AN, Abal G, Tokuccu E, Demir M. Increased mean platelet volume is associated with coronary artery ectasia. PostepyKardiolInterwencyjnej. 2013; 9: 241-245.
- Varol E, Akcay S, Ozaydin M, Erdogan D, Dogan A. Mean platelet volume in patients with coronary artery ectasia. Blood Coagul Fibrinolysis. 2009; 20: 321-324.
- Markis JE, Joffe CD, Cohn PF, Feen DJ, Herman MV, Gorlin R. Clinical significance of coronary arterial ectasia. Am J Cardiol. 1976; 37: 217-222.
- Schiller NB, Shah PM, Crawford M, DeMaria A, Devereux R, Feigenbaum H, Gutgesell H, Reichek N, Sahn D, Schnittger I. Recommendations for quantitation of the left ventricle by two-dimensional echocardiography. American Society of Echocardiography Committee on Standards, Subcommittee on Quantitation of Two-Dimensional Echocardiograms. J Am SocEchocardiogr. 1989; 2: 358-367.
- Bath PM, Butterworth RJ. Platelet size: measurement, physiology and vascular disease. Blood Coagul Fibrinolysis. 1996; 7: 157-161.
- Martin JF, Trowbridge EA, Salmon G, Plumb J. The biological significance of platelet volume: its relationship to bleeding time, platelet thromboxane B2 production and megakaryocyte nuclear DNA concentration. Thromb Res. 1983; 32: 443-460.
- Chu SG, Becker RC, Berger PB, Bhatt DL, Eikelboom JW, Konkle B, Mohler ER, Reilly MP, Berger JS. Mean platelet volume as a predictor of cardiovascular risk: a systematic review and meta-analysis. J ThrombHaemost. 2010; 8: 148-156.
- Estevez-Loureiro R, Salgado-Fernandez J, Marzoa-Rivas R, Barge-Caballero E, Perez-Perez A, Noriega-Concepcion V, Calviño-Santos R, Vázquez-Rodríguez JM, Vázquez-González N, Castro-Beiras A, Kaski JC. Mean platelet volume predicts patency of the infarct-related artery before mechanical reperfusion and short-term mortality in patients with ST-segment elevation myocardial infarction undergoing primary percutaneous coronary intervention. Thromb Res. 2009; 124: 536-540.
- Kostrubiec M, Labyk A, Pedowska-Wloszek J, Hrynkiewicz-Szymanska A, Pacho S, Jankowski K, Lichodziejewska B, Pruszczyk P. Mean platelet volume predicts early death in acute pulmonary embolism. Heart. 2010; 96: 460-465.
- Sarli B, Baktir AO, Saglam H, Arinc H, Kurtul S, Karadag Z, Katlandur H, Akpek M, Kaya MG. No relevant association between coronary artery ectasia and mean platelet volume, gamma-glutamyltransferase and uric acid levels. Turk KardiyolDernArs. 2013; 41: 598-603.
- Varol E, Uysal BA, Dogan A, Ozaydin M, Erdogan D. Mean platelet volume has a prognostic value in patients with coronary artery ectasia. ClinApplThrombHemost. 2012; 18: 387-392.
- Dogdu O, Koc F, Kalay N, Yarlioglues M, Elcik D, Karayakali M, Ozbek K, Kaya MG. Assessment of red cell distribution width (RDW) in patients with coronary artery ectasia. ClinApplThrombHemost. 2012; 18: 211-214.
- Isik T, Kurt M, Ayhan E, Uyarel H, Tanboga IH, Korkmaz AF, Kaya A, Sevimli S. Relation of red cell distribution width with presence and severity of coronary artery ectasia. ClinApplThrombHemost. 2012; 18: 441-447.