ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 16
Impact of the disease management model of "treatment-education-follow-up"Âť on anticoagulant therapy in patients with stroke and atrial fibrillation
Tieyu Tang1,2, Xinjiang Zhang2, Lihong Tao2, Anxiu Sun3, Shenggang Qiu4, Fushan Zhang4, Bing Xie5, Xiaodong Jiao6, Xuhong Liu7 and Lan Tan1*
1Department of Neurology, Qingdao Municipal Hospital, Nanjing Medical University, Nanjing, PR China
2Department of Neurology, the Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, PR China
3Department of Pharmacy, the Affiliated Hospital of Yangzhou University, Yangzhou University, Yangzhou, PR China
4Department of Neurology, Jiangdu People's Hospital, Yangzhou, PR China
5Department of Neurology, Gaoyou People's Hospital, Yangzhou, PR China
6Department of Neurology, the Second People's Hospital of Yangzhou, Yangzhou, PR China
7Department of Neurology, Jiangsu Armed Police General Hospital, Yangzhou, PR China
- *Corresponding Author:
- Lan Tan
Department of Neurology
Qingdao Municipal Hospital
Nanjing Medical University
PR China
Accepted on July 25, 2017
Long-term anticoagulant therapy is the most effective measure to prevent ischemic stroke in patients with Atrial Fibrillation (AF). However, the current anticoagulant therapy in Chinese patients with AF is unsatisfactory compared to those in developed countries. Disease management may help improve the treatment rate, reduce adverse events, and improve the compliance to warfarin anticoagulant therapy. The aim of this study was to compare and observe the impact of the disease management model of “Treatment-Education-Follow-up” (TEF) on anticoagulant therapy in patients with Stroke with AF (SAF). The patients and their families in group TEF were educated on anticoagulant therapy by providing them S-AF prevention and anticoagulant therapy handbooks and performing regular post-discharge telephone follow-up and outpatient observation. Conversely, the patients in the control group (group N) only received simple education; no other education and intervention from the doctors were provided during hospitalization. The mean follow-up duration was 1.5 y. The clinical data, 8-item Morisky Medication Adherence Scale scores, and anticoagulant knowledge questionnaire scores were compared between the two groups. The persistence rate of long-term anticoagulant therapy (84.5% vs. 56.0%, P<0.05), international normalized ratio compliance rate (55.2% vs. 28.0%, P<0.05), and recurrence rate of thrombotic events (4.0% vs. 16.0%, P<0.05) in group TEF were statistically significant compared with those of group N. The medication compliance and anticoagulant knowledge in group TEF significantly improved. Clinical anticoagulation service-based TEF can significantly improve the efficacy and safety of and compliance to warfarin anticoagulant therapy.
Keywords
Ischemic stroke, Atrial fibrillation, Anticoagulation.
Introduction
Long-term anticoagulant therapy is the most effective measure to prevent ischemic stroke in patients with Atrial Fibrillation (AF). The use of the congestive heart failure, hypertension, age>75 y, diabetes mellitus, prior stroke, or Transient Ischemic Attack (TIA) (CHADS2) score or the CHA2DS2-VASc score is recommended in the guidelines for the risk stratification of stroke in patients with non-valvular AF and for guiding anticoagulant therapy [1,2]. However, the stability of the international Normalized ratio (INR) is impacted by many factors owing to the very narrow safety and efficacy window of warfarin, as well as the large individual dose difference; thus, routine monitoring of coagulation and adjusting of the dose are needed. Furthermore, the current anticoagulant therapy of patients with AF in China has two major problems owing to insufficient knowledge and fear of bleeding among physicians and patients: 1: The guidelines recommend that patients with AF with a high risk of stroke should take oral anticoagulants, and warfarin has been accepted widely; however, the compliance rate of many patients is still very low. There is also insufficient anticoagulation in patients with high-risk stroke with AF (S-AF); the data from the China National Stroke Registry [3] have shown that only 19.4% of the patients with acute ischemic stroke plus non-valvular AF receive anticoagulant therapy when discharged. The rate of anticoagulant therapy in China is significantly lower than that reported in the global data [4,5]. Developed countries, such as Europe and the United States (US), have established a variety of chronic disease management models, including the chronic disease community and self-management, which includes the (1) Essen Score and HAS-BLED Score, and anticoagulant therapy should be based on risk factors and underlying diseases balanced with the risk of bleeding; such models also include (2) physician and patient education and (3) active patient follow-up.
The long-term treatment compliance rate is even lower; thus, the number of patients who can achieve standard effective anticoagulant intensity is very small. Therefore, short education and intervention from doctors toward anticoagulant behaviors in hospitalized patients lack long-term constraint force and lasting supportive effects [6]. The purpose of this study is to explore the improvement of anticoagulant therapy in actual clinical settings to determine whether the model of Treatment-Education-Follow-up (TEF) in patients with S-AF would improve the compliance and anticoagulant therapy effect.
Disease management is usually performed by a team composed of specialists, nurses, and disease management staff; this involves health education, follow-up management planning, and management effectiveness assessment according to patients’ individual situations and is a method used to improve treatment compliance and treatment effects and to reduce adverse events [7,8]. In developed countries, such as in Europe and the US, multiple chronic disease management models, including mature community management or self-management, have been established and greatly improved the treatment rate and patient compliance to warfarin anticoagulant therapy [9-12]. Large Chinese tertiary hospitals have also adopted various methods to improve the effects of warfarin anticoagulant therapy, such as disease management, selfefficacy, medication education, telephone follow-up, and pharmacist management, which consequently improve the treatment rate and compliance to warfarin anticoagulant therapy; however, there still exists a huge gap when compared to European countries and the US [4,13,14]. As for research studies on anticoagulant therapy compliance and effects, most of the researchers involved are physicians in the department of cardiology or thoracic surgery, and a considerable proportion of patients with AF receive anticoagulant therapy in the department of neurology when stroke occurs; further, there is still a lack of special training among physicians in the department of neurology and research on educating and managing patients under anticoagulant therapy in China and abroad [15].
Our preliminary studies randomly divided neurologists from 10 Yangzhou hospitals into the disease management group and control group (n=5); the former was provided with a 6-month special knowledge training on ischemic stroke/TIA-AF screening and warfarin anticoagulant therapy, while the latter did not participate in the training. After the training, the physicians’ anticoagulant knowledge and awareness significantly increased. The aim of this study was to further investigate whether the disease management model of TEF can improve long-term anticoagulant therapy compliance and treatment outcomes in patients with S-AF in the actual clinical setting [7,9]. Although the advantage of using new oral anticoagulants (NOACs) has been confirmed in different studies, there was only one kind of NOAC, i.e., dabigatran (110 mg), that could be bought in Yangzhou; it is very expensive, since it has not been listed in the medical insurance in China, making warfarin the most widely used oral anticoagulant in the country. Since only few patients used dabigatran in the study, we have excluded them.
Materials and Methods
Subjects
This study was a multicenter, prospective, and controlled clinical cohort study, and the patients enrolled were admitted owing to acute ischemic stroke/TIA combined with AF and underwent warfarin anticoagulant therapy from October 2014 to September 2015. All the patients had a history of hospitalization. The inclusion criteria were as follows: 1) age>18 y; 2) acute cerebral infarction or TIA; 3) ECG evidence of AF (paroxysmal, persistent, or permanent); 4) agreement to receive warfarin anticoagulant therapy and informed consent; and 5) ability to cooperate with the data collection and follow-up. The exclusion criteria were as follows: 1) anticoagulant allergy, S-AF combined with hemorrhagic cerebrovascular diseases, hemorrhagic diseases, brain/central nervous system tumors, aortic dissection, systemic/metastatic tumors, active peptic ulcer, or other anticoagulant contraindications; 2) serious heart, liver, or renal insufficiency or end-stage diseases; 3) S-AF combined with pulmonary infection or severe systemic infection; and 4) severe mental illness, cognitive dysfunction, or inability to understand and sign the informed consent. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Nanjing Medical University. Written informed consent was obtained from all participants.
TEF
The patients in group TEF were managed by specialists and disease management staff (Masters, PhDs, clinical pharmacists, and trained nurses with a clinical background), who were mainly responsible for the implementation of the disease management. The clinicians provided warfarin anticoagulant therapy to the patients according to their individual risk stratification scores (CHA2DS2-VASc ≥ 2 points) as well as simple anticoagulant therapy education. The patients were provided with stroke prevention and anticoagulant therapy handbooks for patients with AF (edited by the disease management specialists) upon discharge; they were still managed by the specialists and disease management staff even after discharge, who used the following methods: outpatient follow-up, telephone or text alert for the monitoring, medication adjustment, health education, and patient needs management. The control group was only provided with simple education without other education or intervention from the doctors during hospitalization.
Data collection
The data of the patients in group TEF were collected by the doctors via inquiry and reviewing of case records; the data of group N were collected via reviewing of their case records, questionnaire scores, and hospital treatment information. The demographic data (including social, economic, and cultural data), medical history, clinical signs and symptoms, laboratory test results, radiographic data, and other treatment information of all the patients were collected and recorded. The patients were enrolled for 6 months to one and a half years, with an average of 1 y. At the end of March 2016, the treatment compliance and anticoagulant therapeutic effects in the two groups were evaluated via outpatient follow-ups and questionnaires.
Clinical observation indicators
1) Warfarin anticoagulant compliance, endpoint events, INR monitoring rate and standard achieving rate, and patients’ knowledge level; 2) effectiveness indicators: ischemic event recurrence, including cerebral infarction, TIA, myocardial infarction, or other ischemic vascular events (i.e., pulmonary embolism, deep vein thrombosis, or peripheral arterial occlusive disease); and 3) safety indicators: hemorrhagic events, including cerebral hemorrhage and subarachnoid hemorrhage, hemoptysis, gastrointestinal bleeding, hematuria, or other major bleeding events.
Compliance measurement
The questionnaire used the 8-item Morisky Medication Adherence Scale (Chinese version) [16]; this uses eight questions to determine the patients’ compliance to anticoagulant therapy. The answers to Questions 1 to 7 were only “yes” or “no”; “no” were recorded as 1 point and “yes” as 0 points. Question 5 was reversely scored; the answer to Question 8 used the Likert rating score, namely “never,” “rarely,” “sometimes,” “often,” or “always,” with the score recorded as 1, 0.75, 0.5, 0.25, and 0 points, respectively. The total scale score was 8 points and higher scores indicated better compliance. The compliance scores of the patients with S-AF were divided into three levels according to their INRs predicted based on their warfarin compliance: 8 points indicated a high compliance; 6-7.75 points indicated a moderate compliance; and <6 points indicated a low compliance. Our previous study showed that the Cronbach's coefficient was 0.82 (8-item Morisky Medication Adherence Scale, Chinese version); the consistency coefficient among assessors was 0.93; the retest coefficient was 0.95; the scale’s surface validity was 1.01; and the correlation coefficient between the items and the total score was 0.40-0.85.
Knowledge on warfarin anticoagulant therapy
The knowledge questionnaire on warfarin anticoagulant therapy was self-designed on the basis of relevant literature [17] and expert opinions; it had a total of 15 items. The sum score of the first 12 items was used to assess the patients’ knowledge on warfarin anticoagulant therapy upon discharge; each item required a “yes” or “no” answer (recorded as 1 or 0 points, respectively). Higher scores indicated better knowledge mastery of anticoagulant therapy. The 13th and 14th items reflected the patients’ satisfaction with the follow-up; the last item was a multiple-choice question for assessing the patients’ ways of understanding anticoagulant therapy; these three items were not included in the statistical analysis of anticoagulant therapy knowledge.
Statistical analysis
SPSS version 16.0 was used for the statistical analysis. The measurement data were expressed as means ± standard deviations, and the t-test was used for the intergroup comparison. The count data were expressed as frequencies or percentages, and the χ2 test or the Fisher’s exact test was used for the intergroup comparison, with P<0.05 considered as statistically significant.
Results
Enrolment information
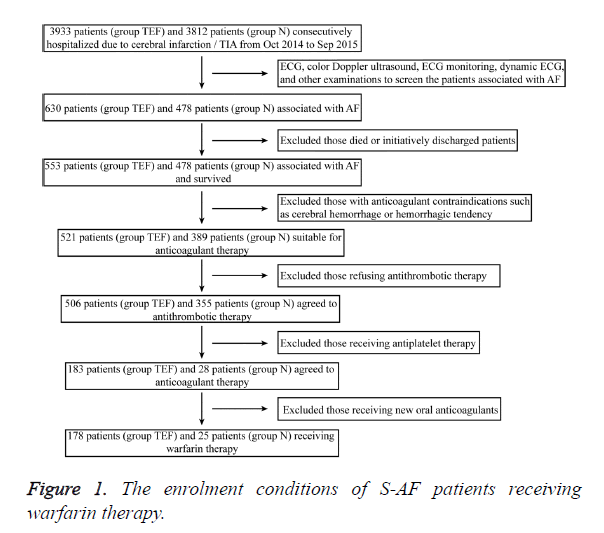
A total of 3,933 patients with acute cerebral infarction or TIA were enrolled in group TEF within 1 y, including 630 patients with AF (16.0%); of them, 178 patients received warfarin, and five patients received dabigatran. A total of 3,812 patients with acute cerebral infarction or TIA were enrolled in group N, including 478 patients with AF (12.5%); of them, 25 patients received warfarin, and three patients received dabigatran. The enrolment conditions for warfarin anticoagulant therapy in the two groups are shown in Figure 1.
A total of 178 patients with S-AF in group TEF underwent warfarin anticoagulant therapy upon discharge; four of them were lost to follow-up. Twenty-five patients in group N underwent warfarin anticoagulant therapy during the same period, and all their endpoint events, 8-item Morisky Medication Adherence Scale scores, and warfarin anticoagulation knowledge questionnaire scores were assessed. Among the 174 patients with complete information in group TEF, 60.3% were men aged 36-91 y. Among the 25 patients in group N, 56.0% were men aged 39-89 y. There was no statistically significant difference in sex, age, and history and type of AF between the two groups (Table 1).
| Group | n | Male (%) | Age (%) | History of AF (%) | Type of AF (%) | |||
|---|---|---|---|---|---|---|---|---|
| <65 y | 65-75 y | ≥ 75 y | Paroxysmal | Persistent or permanent | ||||
| TEF | 174 | 60.3 | 13.8 | 22.4 | 63.8 | 74.1 | 23.6 | 76.4 |
| N | 25 | 56 | 16 | 24 | 60 | 68 | 20 | 80 |
| Note: *P<0.05. | ||||||||
Table 1. Basic information of the two groups.
Conditions of anticoagulant therapy
The average 1.5 y follow-up revealed that 84.5% and 56.0% of the patients in group TEF and group N insisted on taking warfarin, respectively; thus, the compliance in group TEF was higher than that in group N. There were statistically significant differences in the ratios of achieving the INR standard (2.0-3.0) and recurrent thromboembolic events between the two groups; however, there was no statistically significant difference between the two groups in the ratios of monthly monitoring of INR more than once and bleeding events (Table 2).
| Group | n | Medication compliance | Monthly INR monitoring value | INR (2.0-3.0) | Events of thrombus | Events of bleeding | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| n | Percentage (%) | n | Percentage (%) | N | Percentage (%) | n | Percentage (%) | n | Percentage (%) | ||
| TEF | 174 | 147 | 84.5* | 108 | 62.1 | 96 | 55.2* | 7 | 4.0* | 5 | 2.9 |
| N | 25 | 14 | 56 | 11 | 44 | 7 | 28 | 4 | 16 | 1 | 4 |
| Note: *P<0.05. | |||||||||||
Table 2. Comparison of anticoagulant therapy between the two groups.
Eight-item Morisky medication adherence scale-based self-evaluation of medication compliance
The results are shown in Table 3. The ratios of good and low compliance in group TEF were 58.0% and 16.7% and those in group N were 36.0% and 48.0%, respectively. The differences were significant (P<0.05). However, there was no statistically significant difference in the patients with moderate compliance between the two groups.
| Group | n | Cases with good compliance (%) | Cases with moderate compliance (%) | Cases with low compliance (%) |
|---|---|---|---|---|
| TEF | 174 | 101 (58.0)* | 44 (25.3) | 29 (16.7)* |
| N | 25 | 9 (36.0) | 4 (16.0) | 12 (48.0) |
| Note: *P<0.05 | ||||
Table 3. Comparison of anticoagulant therapy compliance in S-AF patients between the two groups.
Comparison of anticoagulant knowledge mastery
The results are shown in Table 4. The patients in group N had greater awareness on AF and are more prone to develop stroke; warfarin has the side effect of bleeding, and the INR needs to be monitored; however, these patients had a low awareness on warfarin’s antithrombotic effect, reasonable indicators of INR, and diet attention after warfarin administration. The knowledge awareness rate in group TEF was higher than that in group N (P<0.01).
| Related knowledge | TEF, n=174 | N, n=25 | χ2 | P | ||
|---|---|---|---|---|---|---|
| Cases | Rate of knowing (%) | Cases | Rate of knowing (%) | |||
| Purposes of anticoagulant therapy | 156 | 89.7* | 16 | 64 | 12.3 | <0.01 |
| Impact factors of drugs | 143 | 82.2* | 11 | 44 | 18.2 | <0.01 |
| Frequency and target of INR monitoring | 161 | 92.5* | 15 | 60 | 22.6 | <0.01 |
| Medication instructions | 159 | 91.4* | 10 | 40 | 45.1 | <0.01 |
| Note: *P<0.01. | ||||||
Table 4. Comparison of anticoagulant therapy-related knowledge between the two groups.
Discussion
Cerebral embolism is the most serious complication in patients with AF; such patients should receive early secondary prevention of stroke. Owing to various reasons, Chinese doctors and patients are less willing to use warfarin, making the latter more prone to require antiplatelet therapy or nonantithrombotic therapy [3,4,18]. Developed countries in Europe and the US have launched community-based chronic disease management and treatment-related exploration and have made remarkable achievements, which establish such chronic disease management models as mature chronic disease community management or self-management and greatly improve the treatment efficacy and patients’ compliance to warfarin therapy [9-12]. However, post-discharge follow-up, inspection, drug dose adjustment, etc. in China are still mainly performed by doctors in secondary and tertiary hospitals, and no specific disease management personnel can be assigned for high-quality chronic disease management, which is the main cause of the large difference in the coagulation status of AF between China and other developed countries. Many studies found that a low prescription rate is the major barrier of anticoagulant therapy, which may be related to the fear of hemorrhagic complications and underestimation of the benefit of anticoagulant therapy. The causes of patients’ low compliance included the following: socioeconomic characteristics, medical team and system characteristics, disease-related characteristics, therapy-related characteristics, and patient-related characteristics. The aim of this study was to determine the compliance of TEF to anticoagulant therapy in patients with S-AF and avoid any bias in sex, age, and history and type of AF.
We are conducting education programs for patients with AF, learning from foreign chronic disease management models, forming disease management teams, and establishing anticoagulant clinics; on one hand, we educate patients using anticoagulation handbooks and on the other hand, patients are followed-up via telephone, text, and personal follow-up management information system, so that INR monitoring and drug dose adjustment can be performed in the patients. This study found that the compliance rate in group TEF was 30% higher than that in group N; the persistence rate of long-term anticoagulant therapy (84.5% vs. 56.0%, P<0.05), INR compliance rate (55.2% vs. 28.0%, P<0.05), and recurrence rate of thrombotic events (4.0% vs. 16.0%, P<0.05) all statistically increased, suggesting that the disease management model of TEF can significantly improve not only the patients’ compliance to anticoagulant therapy but also the anticoagulant effects and knowledge on anticoagulant therapy. After mastery of the related knowledge, the patients learned to understand their monitoring results, diet, and methods of self-protection and bleeding prevention, thus benefitting from the standardized warfarin therapy. There was no significant difference in bleeding between the two groups, suggesting that adjusting the dose of warfarin did not increase the risk of bleeding. Anticoagulation clinics are generally accepted by patients, and most patients want to have a face-to-face communication opportunity with doctors once a month. In addition, the patients in this study also praised the establishment of a special telephone in the hospital, which facilitated their consult.
In this study, the score of the post-discharge warfarin compliance in group TEF was 7.3 ± 0.9 points, which was in a moderate level, and 58.0% of the patients exhibited a high compliance, which was lower than foreign reports (80%) [19]. In addition, the results of this study showed that 25.3% and 16.7% of the patients still exhibited moderate and low warfarin compliance, respectively. The analysis of each item in the warfarin compliance table revealed that considering on insisting on life-long warfarin administration to be difficult and forgetting to take warfarin are the main reasons for poor warfarin compliance.
This study found that 21 patients in group TEF initiatively discontinued warfarin; 21 patients discontinued within 1 month of discharge (77.8%); the reason for discontinuing warfarin in 22 patients (81.5%) was because of the large fluctuations in the INR, making the dosage difficult to be adjusted. Only three patients (11.1%) and two patients (7.4%) discontinued because of their fear of bleeding and feeling cumbersome to monitor their INR, respectively. This indicates that warfarin discontinuation is more frequent in an early stage, and INR fluctuations are the main reason, which are consistent with those of foreign studies [6,19,20]. To improve the compliance to anticoagulant therapy, early post-discharge supervision is very important; such a method would let the patients learn that warfarin is prone to being affected by food or drugs, especially blood circulation-activating and blood stasis-dissipating drugs, such as Naoxintong or Sanqi powders, to reduce INR fluctuations. In addition, small-dose-based gradual increment, individual gene screening-based dosage adjustment, or combination with NOACs, such as dabigatran, can improve the compliance to anticoagulant therapy.
Anticoagulant outpatient treatment-based TEF is suitable for disease management in hospitals and communities. Our group is spreading the knowledge on anticoagulation and follow-up management among communities. This chronic disease management model is suitable for the management of not only patients undergoing anticoagulant therapy but also those with hypertension, diabetes, coronary heart disease, etc.
Limitations
First, self-comparison of anticoagulant therapy in the same group before and after treatment was not performed. Second, the anticoagulant therapy efficacy and compliance of the two groups in different hospitals varied significantly; however, no further stratification analysis was performed. We will continue to work further on improving anticoagulant therapy in actual clinical settings.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Vallakati A, Lewis WR. Underuse of anticoagulation in patients with atrial fibrillation. Postgrad Med 2016; 128: 191-200.
- Culebras A, Messe SR, Chaturvedi S, Kase CS, Gronseth G. Summary of evidence-based guideline update: prevention of stroke in nonvalvular atrial fibrillation: report of the Guideline Development Subcommittee of the American Academy of Neurology. Neurology 2014; 82: 716-724.
- Yang X, Li Z, Zhao X, Wang C, Liu L, Wang C, Pan Y, Li H, Wang D, Hart RG, Wang Y, Wang Y, China National Stroke Registry II Investigators. Use of warfarin at discharge among acute ischemic stroke patients with nonvalvular atrial fibrillation in China. Stroke 2016; 47: 464-470.
- Chang SS, Dong JZ, Ma CS, Du X, Wu JH, Tang RB, Xia SJ, Guo XY, Yu RH, Long DY, Bai R, Liu N, Sang CH, Jiang CX, Liu XH, Pan JH, Lip GY. Current status and time trends of oral anticoagulation use among chinese patients with nonvalvular atrial fibrillation the Chinese atrial fibrillation registry study. Stroke 2016; 47: 1803-1810.
- Wehbe RM, Yadlapati A. Underuse of oral anticoagulants for nonvalvular atrial fibrillation: past, present, and future. Tex Heart Inst J 2016; 43: 287-290.
- Wang ZZ, Du X, Wang W, Tang RB, Luo JG, Li C, Chang SS, Liu XH, Sang CH, Yu RH, Long DY, Wu JH, Bai R, Liu N, Ruan YF, Dong JZ, Ma CS. Long-term persistence of newly initiated warfarin therapy in chinese patients with nonvalvular atrial fibrillation. Circ Cardiovasc Qual Outcomes 2016; 9: 380-387.
- Clarkesmith DE, Pattison HM, Lip GY, Lane DA. Educational intervention improves anticoagulation control in atrial fibrillation patients: the TREAT randomised trial. PLoS One 2013; 8: 74037-74047.
- Karamichalakis N, Letsas KP, Vlachos K, Georgopoulos S, Bakalakos A, Efremidis M, Sideris A. Managing atrial fibrillation in the very elderly patient: challenges and solutions. Vasc Health Risk Manag 2015; 11: 555-562.
- Jones S, McLoughlin S, Piovesan D, Savoia H, Monagle P, Newall F. Safety and efficacy outcomes of home and hospital warfarin management within a pediatric anticoagulation clinic. J Pediatr Hematol Oncol 2016; 38: 216-220.
- Bengtson LG, Lutsey PL, Loehr LR, Kucharska-Newton A, Chen LY, Chamberlain AM, Wruck LM, Duval S, Stearns SC, Alonso A. Impact of atrial fibrillation on healthcare utilization utilization in the community: the atherosclerosis risk in communities study. J Am Heart Assoc 2014; 3: 001006.
- Donoghue OA, Jansen S, Dooley C, De Rooij S, Van Der Velde N, Kenny RA. Atrial fibrillation is associated with impaired mobility in community-dwelling older adults. J Am Med Dir Assoc 2014; 15: 929-933.
- Blann AD, Banerjee A, Lane DA, Torp-Pedersen C, Lip GY. Net clinical benefit of edoxaban versus no treatment in a real world atrial fibrillation population: A modelling analysis based on a nationwide cohort study. Int J Cardiol 2015; 201: 693-698.
- Choi HY, Seo JH, Yang JH, Kim YD, Jung YH, Cho HJ, Nam HS, Heo JH. Beneficial effects of stroke-unit care in stroke patients with atrial fibrillation. Yonsei Med J 2013; 54: 301-305.
- Chen CH, Chen MC, Gibbs H, Kwon SU, Lo S, On YK, Rosman A, Suwanwela NC, Tan RS, Tirador LS, Zirlik A. Antithrombotic treatment for stroke prevention in atrial fibrillation: The Asian agenda. Int J Cardiol 2015; 191: 244-253.
- Van der Sand CR, Leiria TL, Kalil RA. Assessment of the adherence of cardiologists to guidelines for the treatment of atrial fibrillation. Arq Bras Cardiol 2013; 101: 127-133.
- Wang Y, Kong MC, Ko Y. Psychometric properties of the 8-item Morisky Medication Adherence Scale in patients taking warfarin. Thromb Haemost 2012; 108: 789-795.
- Van Damme S, Van Deyk K, Budts W, Verhamme P, Moons P. Patient knowledge of and adherence to oral anticoagulant therapy after mechanical heart-valve replacement for congenital or acquired valve defects. Heart Lung 2011; 40: 139-146.
- Kakkar AK, Mueller I, Bassand JP, Fitzmaurice DA, Goldhaber SZ, Goto S, Haas S, Hacke W, Lip GY, Mantovani LG, Turpie AG, van Eickels M, Misselwitz F, Rushton-Smith S, Kayani G, Wilkinson P, Verheugt FW, GARFIELD Registry Investigators. Risk profiles and antithrombotic treatment of patients newly diagnosed with atrial fibrillation at risk of stroke: perspectives from the international, observational, prospective GARFIELD registry. PLoS One 2013; 8: 63479.
- Mayet AY. Patient adherence to warfarin therapy and its impact on anticoagulation control. Saudi Pharm J 2016; 24: 29-34.
- Murphy SJ, Coughlan CA, Tobin O, Kinsella J, Lonergan R, Gutkin M, McCabe DJ. Continuation and adherence rates on initially-prescribed intensive secondary prevention therapy after Rapid Access Stroke Prevention (RASP) service assessment. J Neurol Sci 2016; 361: 13-18.