ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 17
Impact of backward treadmill training on balance in children with juvenile rheumatoid arthritis: A randomized controlled study
Heba Gaber Abd El Aziz1, Hamada Ahmed Hamada2* and Ayman El Khatib3
1Department of Physical Therapy for Pediatric and its Surgery, Faculty of Physical Therapy, Cairo University, Egypt
2Department of Biomechanics, Faculty of Physical Therapy, Cairo University, Egypt
3Department of Physical Therapy, Faculty of Health Sciences, Beirut Arab University, Beirut, Lebanon
- *Corresponding Author:
- Hamada Ahmed Hamada Ahmed
Department of Biomechanics
Faculty of Physical Therapy
Cairo University
Egypt
Accepted date: August 21, 2017
Background: Juvenile Rheumatoid Arthritis (JRA) is one of the most common chronic rheumatologic diseases in children under 16 years of age, causing repeated falls due to decrease in joint development and impairment of balance control.
Objective: To investigate the effect of additional backward walking training on postural control in children with polyarticular Juvenile Rheumatoid Arthritis (pJRA).
Materials and Methods: Thirty children with pJRA (18 girls and 12 boys) were assigned randomly into two equal groups (control and study). Both group received selected physical therapy program for three months. Study group additionally received backward walking training which was provided 20 min/d, 3 d/w for 3 successive months. They were assessed and treated at the Faculty of Physical Therapy, Cairo University. Biodex balance system was used to measure overall, anteroposterior, and mediolateral stability indices and Berg's balance scale were used to assess balance performance before and after treatment.
Results: There was significant improvement in all measured variables of the control and study groups after treatment. However, significant improvement was marked in the study group when comparing the post-treatment mean values of this group with the control group.
Conclusions: Backward treadmill training can be used as an adjuvant therapeutic modality to improve balance in children with JRA.
Keywords
Juvenile rheumatoid arthritis, Balance, Backward treadmill training, Biodex balance system
Introduction
Juvenile Rheumatoid Arthritis (JRA) is the most common chronic rheumatologic disease in children, causing major chronic disability among the pediatric patients group [1]. It is a chronic autoimmune disorder that has considerable effects on the quality of life. Studies confirmed that rheumatic diseases may cause substantial physical disability prompting high societal and economic costs [2]. Patients with JRA usually present complaining of joint stiffness and swelling, decreased physical activity, joint pain, and fatigue [3,4]. Synovitis alone can lead to instability of the structures which support the joint affecting the overall biomechanical function of the joint. With time, and as the disease progresses, deterioration and deformities in the joint occurs leading to articular instability [5].
Children with JRA may suffer from both proprioceptive deficits and impairments in the motor responses, making them vulnerable to balance distresses. Inflammation of the lower limb joints may be accompanied with loss of muscle strength, especially if affecting the weight-bearing joints, where impairment in ambulation, mobility, exercise tolerance, and postural control occurs [6].
An essential entity required for performing tasks at all levels from infancy through adulthood is postural control. While postural control permits us to be mobile, balance deficits constraint this mobility [7].
Maintenance of postural control is essential to enhance postural stability in children. Physical therapists utilize backward walking on a treadmill to restore patients’ ability to participate in different sports. This new therapy had been shown to be safe enough to enhance poor motor function, postural stability, and muscle and joint strengths of the lower limbs in stroke patients [8,9] and for healthy children as well [9,10].
Nevertheless, studies evaluating the efficiency of additional backward walking training on balance in JRA are still scarce. The purpose of this study is to assess the effect of backward walking combined with traditional physical therapy program on postural control in children with JRA.
Materials and Methods
Study design
The study was designed as a prospective, randomized, single-blind, pre–post-test, controlled trial.
Study participants and setting
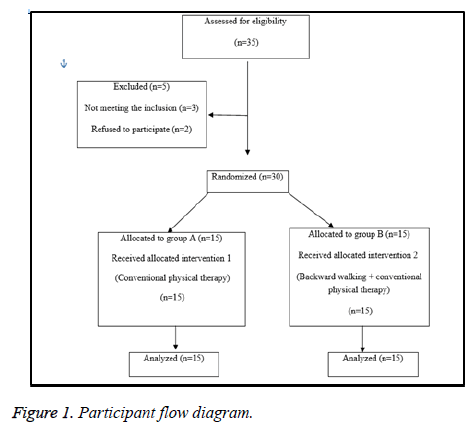
Thirty-five children with polyarticular Juvenile Rheumatoid Arthritis (pJRA) from both genders were selected from the National Institute of Neuro-motor disorders and El-Kasr Elainy (collagen clinic). They were enrolled and assessed for their eligibility to participate in the study. Their age ranged from 6 to 10 y. They were assessed and treated in labs and outpatient clinics of the Faculty of Physical Therapy, Cairo University. Before randomization, five children were excluded, two children with height less than one meter, one child with severe osteoporosis; two children chose to withdraw their consent for participation in the study (Figure 1). After a brief orientation session about the nature of the study and the tasks to be accomplished, they were randomly assigned into two equal groups (control group (A) and study group (B)) by a blinded and an independent research assistant who opened sealed envelopes that contained a computer generated randomization card. No subjects dropped out of the study after randomization. Written informed consent was obtained from all participants before the baseline evaluation. Ethical approval was obtained from the institutional review board at Faculty of physical therapy, Cairo University before study commencement. The study was followed the Guidelines of Declaration of Helsinki on conduction of human research. The study was conducted between September 2015 and October 2016.
The inclusion criteria were children age ranged from 6 to 10 y old; diagnosed with pJRA (moderate severity, preschool onset; Child had balance problems as confirmed by a tilt board balance test with average sum of the maximum degrees of tilt with both eyes opened and eyes closed were less than 32.1 and 25.8 respectively [11]; can walk both forward and backward without assistance; and their heights were 1 meter and more to be able to see the screen of Biodex balance system. Exclusion criteria were children with systemic oroligoarthritis onset, advanced radiographic changes as (bone destruction, bone ankylosis, severe osteoporosis and epiphyseal fracture), skin disease (juvenile psoriatic arthritis) and who had any experience of backward training before the trial.
Sample size
The sample size and power calculations were performed using G power 3.1 Software. The calculations were based on the results from the unpublished pilot study on postural control in children with pJRA. With a power of 80% and a significant level of 5%, the total number of participants needed for this study was calculated to be 30.
Instrumentation
Biodex balance system: Biodex Balance System (Biodex medical system, Shirly, New York) was used for the assessment of the dynamic postural control of all children’s in the two tested groups. The system utilizes dynamic multi axial platform. This platform allows approximately 20 degrees’ inclination in 360 degrees range and is interfaced with computer software. It measures the child’s ability to control the platform's angle of tilt, which is quantified as a variance from the center, as well as the degree of deflection over time at various stability levels [12]. Stability levels allowed by the system ranged from one to eight. Stability level eight, allows the highest level of stability as it makes the platform to be the least tilted and is easier for the subject to maintain stability on. On the other hand, stability level one represents the least level of stability as it makes the platform to be the highest tilted and is more difficult for the subject to maintain stability [13,14].
The child's performance was noted as a stability index. A high number is an indicative of a lot of motion, which indicates balance problem. The data regarding the balance of the tested participant include Overall Stability Index (OSI) (representing the child's ability to control the balance in all directions), Antero-Posterior Stability Index (APSI) (representing the child's ability to control the balance in front to back directions (sagittal plane)), and Medio-Lateral Stability Index (MLSI) (representing the participant's ability to control the balance in side to side directions (frontal plane)) [15].
Berg's balance scale: The Berg Balance Scale (BBS) is a validated scale to assess balance performance in neurological cases. It is made out of 14 items that expect subjects to maintain positions of various difficulty and perform specific missions such as standing and sitting unsupported, transfers (sit to stand and stand to sit), turn to look over shoulders, pick up an object from the floor, turn 360° and place alternate feet on a stool. Scoring depends regarding the matter's capacity to play out the 14 assignments autonomously and additionally meet certain time or separation prerequisites. Every item is scored on a 5-point ordinal scale extending from 0 (unfit to perform) to 4 (typical execution) with the goal that the total score ranges from 0 to 56 [16].
Treatment
Both groups received 60 min traditional physical therapy exercise program, three sessions/w for three successive months. The program included stretching exercises for the tightened muscles (hamstring muscles, hip adductor muscles, calf muscles, back muscles and wrist flexor and extensor muscles) to the limit of pain without vigorous pressure followed by passive ROM exercises for (ankle, knee, hip and wrist) joints, active-assistive exercises for (ankle, knee, hip and wrist) joints as well as active exercises (ankle, knee, hip and wrist) joints. In addition to the ROM exercises, facilitation of standing from supine and prone positions as well as standing facing the stand bar was performed. Followed the facilitation technique, strengthening exercises for weak muscles particularly knee extensors, hip abductors and ankle dorsiflexors muscles were performed. Gait training activities were also essential elements for balance training including; sideway, forward and backward walking between parallel bars and walking training using stepper. The physical therapy program included, as well, gait training in open environment by placing obstacles including rolls, wedges across walking tract and walking training on different surfaces like soft mat, sponge, carpet, or hard surface. In addition, Balance training exercises were added to the program using balance board performing both static balance from different positions and dynamic balance associated with movement. The rehabilitation program of study group (B) they delivered the previously mentioned physical therapy program and backward walking on treadmill by the following manner, at beginning the child walk on treadmill as a warm-up session for 5 min at a self-selected speed and then they were given a 1 min rest before the training session started [17]. The authors informed the child to start off slow, as this is a completely new sensation for him/her and it will take some time getting used to it. The child should take it slow and increase speed only when feeling comfortable, during the training session, the child walked backward on the treadmill at speed which is started from 1.2 up to 1.6 m/s and when the child progresses speed could be increased. Instructions were given to the child to catch the rails during walking if they felt balance disturbance [18], duration of treadmill was 20 min for backward walking with rest periods about 5 min between every 10 min.
Outcomes
Primary outcome (Dynamic balance testing): Before the testing procedures, the child’s weight, height and age were introduced into the system. All children were tested on stability level 5 for 30 s according to Aydog et al. [19]. Firstly, each child received verbal explanation about the testing steps. The child was asked to assume the test position and try to control his/her balance as much as possible during the testing procedures [20]. Each child was asked to perform two test trials before the actual testing procedures for the purpose of instrument familiarity prior to data collection [21]. Finally, after conducting the actual test at the stability level 5, a printout report was obtained. This report included the information regarding the OSI, APSI and MLSI. The mean values were recorded for each child at the two tested groups.
Secondary outcome (Berg balance scale): All children were evaluated with the BBS by the same therapist before and after a physical therapy program for both groups. A change of 8 points is required to reveal a genuine change in function between 2 assessments [16].
Statistical analyses
All statistical measures were performed using the Statistical Package for Social science (SPSS) program version 20 for windows. Descriptive analyses showed that the data were normally distributed and not violates the parametric assumption for the all measured dependent variables (OSI, APSI, MLSI and berg balance scale). Additionally, testing for the homogeneity of covariance using Box's test revealed that there was no significant difference with p values of >0.05. The box and whiskers plots of the tested variables were done to detect the outliers. Normality test of data using Shapiro-Wilk test was used, that reflect the data was normally distributed for all dependent variables. All these findings allowed the researchers to conduct parametric analysis. So, 2 × 2 mixed design MANOVA was used to compare the tested variables of interest at different tested groups and measuring periods. The alpha level was set at 0.05.
Results
The 30 included children were divided into two groups A and B each consisted of 15 children. No significant differences (p>0.05) were found between both groups in the mean values of their ages, weights, and heights (Table 1).
| Characteristics | Group A (n=15) | Group B (n=15) | t-value | P-value |
|---|---|---|---|---|
| Age (y) | 7.38±1.18 | 7.06±1.24 | -0.736 | 0.252 |
| Weight (Kg) | 28.73 ±2.6 | 27.73 ±3.1 | -0.956 | 0.347 |
| Height (cm) | 122.06±13.19 | 117.6±12.83 | -0.94 | 0.355 |
| *Significant level is set at alpha level<0.05. | ||||
Table 1: Demographic characteristics of patients in both groups.
Statistical analysis using mixed design MANOVA to analyse the differences between the two groups revealed significance within subject effect (F=371.109, p=0.0001) and treatment time effect (F=64.759, p=0.0001), as well as between subject effect (F=2.591, p=0.04). Table 2 represents descriptive statistics (mean ± SD) and multiple pairwise comparison tests (Post hoc tests) for the all dependent variables. In the same context, regarding within subject effect, the multiple pairwise comparison tests revealed that there was significant decrease (p<0.05) in OSI, APSI, and MLSI in the post-treatment condition compared with the pre-treatment in both groups and significant increase (p<0.05) in berg balance scale in the post-treatment condition compared with the pre-treatment in both groups. Regarding between subject effects, multiple pairwise comparisons revealed that there was significant reduction (p<0.05) in OSI, APSI, and MLSI and significant increase (p<0.05) in berg balance scale in favor to group B than group A.
| Group A | Group B | |||
|---|---|---|---|---|
| Variables | Pre- | Post- | Pre- | Post- |
| Overall stability | 1.96 ± 0.44 | 1.71 ± 0.46 | 2.12 ± 0.32 | 1.3 ± 0.28 |
| AP stability | 1.62 ± 0.34 | 1.32 ± 0.32 | 1.65 ± 0.20 | 0.98 ± 0.22 |
| ML stability | 1.69 ± 0.32 | 1.36 ± 0.36 | 1.77 ± 0.24 | 1.04 ± 0.23 |
| Berg balance scale | 38.66 ± 2.91 | 43.26 ± 2.89 | 39.26 ± 3.28 | 49.26 ± 3.12 |
| Within groups (Pre vs. Post) | ||||
| p-value | Overall stability | AP stability | ML stability | Berg balance scale |
| Group A | 0.0001* | 0.0001* | 0.0001* | 0.0001* |
| Group B | 0.0001* | 0.0001* | 0.0001* | 0.0001* |
| Between groups (group A vs. group B) | ||||
| p-value | Overall stability | AP stability | ML stability | Berg balance scale |
| Pre-treatment | 0.252 | 0.8 | 0.455 | 0.601 |
| Post-treatment | 0.008* | 0.003* | 0.009* | 0.0001* |
| *Significant at the alpha level (p<0.05). | ||||
Table 2: Descriptive statistics and multiple pairwise comparison tests (Post hoc tests) for the all dependent variables for both groups at different measuring periods.
Discussion
This study was conducted to investigate the effect of backward treadmill training as an adjuvant therapy to conventional physiotherapy program on dynamic balance in children with pJRA. Results revealed enhancement in APSI, MLSI, OSI and berg balance scale for both groups. However, the significant improvement obtained in the post-treatment mean values of the measured variable especially for the study group may be attributed to the effect of backward gait training. This comes in agreement with Chen et al. [22] who stated that muscles working during the backward walking on a treadmill differ from those when walking forwards. Backward walking on the treadmill (especially on an incline) involves the quadriceps muscles and calves to a great extent.
Study group results showing greater improvement might be attributed to the different motor learning theories that accentuate the significance of concentrated and repetitive training of motor skills in improving motor functions and skill potentials [23,24].
Backward walking acts to improve the patient’s balance and proprioception and will act to condition hip, knee and ankle stabilizers. This increase at the speed of walking is related also to the increase at lower limb activity that occurs with backward walking as when the activity of lower limb muscles is improved so the patient can move at faster speed [25]. Kramer et al. reported that backward walking induce leg muscles to be active for a longer period, resulting in greater muscle strength [26].
Moreover, when studying the effect of backward walking as compared to forward walking on activation of areas in the brain, it was shown that backward walking promotes stimulation of larger areas in the cerebrum with less activation in the cerebellum and brainstem [27]. This is accompanied by presence of more oxygenated haemoglobin in the activated areas as confirmed by Kurz et al. [28]. Indeed, in human bipedal gait, there is crucial role for the motor cortex due to the added need for control of stability [29].
The improvement in the measured parameters can be also attributed to the mechanical and neural responses to backward walking. These are based on two primary modifications. A reduction in hip movement which probably increases constancy by decreasing the anterior-posterior shifting of the center of gravity, and shorter absolute swing/stance duration. Plantar flexion and doriflexion angles were found also to be greater during forward than backward walking. This marked change in ankle movement alters the functional demands placed upon the ankle joint. These modifications imply differential effects of afferent input on the neural circuits controlling ankle movements in comparison to the mechanical aspect of the movements affecting the hip and knee joints. This alteration at ankle joint influences proprioceptive responses through backward walking as related to forward walking [30].
The improvement in OSI of study group after three months of backward gait training can be attributed to the effect of the backward gait training using treadmill which can be explained on the basis that prolonged backward walking exercise causes neural adaptations [31]. In forward walking, stance begins with heel strike and ends at toe-off, whereas in backward walking, toes touch the ground first and the heel is lifted off the ground at the end [32,33].
There are some limitations of this study. Firstly, the lack of follow-up for children in group B for several months’ post rehabilitation program to evaluate the long lasting effect of additional effect of backward walking training on postural control in children with polyarticular Juvenile Rheumatoid Arthritis (pJRA). Secondly, certain secondary outcome variables such as, pain, functional activity, and muscle strength were not assessed. In conclusion, this study shows that backward treadmill training can be used as a supplementary therapeutic modality to improve balance in children with JRA.
Funding
Not funded.
Conflict of Interest
Authors declare no potential conflicts of interest.
Acknowledgements
We would like to thank all individuals who contributed to the completion of this work, especially study participants.
References
- Harrison P. Antibiotics in children increase risk for juvenile arthritis Medscape 2014; 2.
- Cassidy JT, Petty RE, Laxer RM, Lindsley CB. Textbook of pediatric rheumatology. Elsevier Health Sciences 2010.
- Bromberg MH, Connelly M, Anthony KK, Gil KM, Schanberg LE. Self-reported pain and disease symptoms persist in juvenile idiopathic arthritis despite treatment advances. an electronic diary study. Arthritis Rheumatol 2014; 66: 462-469.
- Stanley LC, Ward-Smith P. The diagnosis and management of juvenile idiopathic arthritis. J Pediatr Health Care 2011; 25: 191-194.
- Philips CA. Rehabilitation of the patient with rheumatoid hand involvement. Phys Ther 1989; 69: 1091-1098.
- Klepper SE. Exercise and fitness in children with arthritis: evidence of benefits for exercise and physical activity. Arthritis Rheum 2003; 49: 435-443.
- Hale SA. Postural control in children and young adults, in kinesiology. Pennsylvania State University, Pennsylvania, United States of America 2004.
- Weng CS, Wang J, Pan XY, Yu ZZ, Wang G, Gao LP,. Huo CN. Effectiveness of backward walking treadmill training in lower extremity function after stroke. Zhonghua Yi Xue Za Zhi 2006; 86: 2635-2638.
- Threlkeld AJ, Horn TS, Wojtowicz G, Rooney JG, Shapiro R. Kinematics, ground reaction force, and muscle balance produced by backward running. J Orthop Sports Phys Ther 1989; 11: 56-63.
- Zhang S, Lin Z, Yuan Y, Wu Xf. Effect of backward-walking on the static balance ability and gait of the aged people. Chinese J Sports Med 2008; 27: 304-307.
- Broadstone BJ, Westcott SL, Deitz JC. Test-retest reliability of two tiltboard tests in children. Phys Ther 1993; 73: 618-625.
- Testerman C, Vander Griend R. Evaluation of ankle instability using the Biodex Stability System. Foot Ankle Int 1999; 20: 317-321.
- Hinman MR. Factors affecting reliability of the Biodex Balance System: a summary of four studies. J Sport Rehab 2000; 9: 240-252.
- Pereira HM, de Campos TF, Santos MB, Cardoso JR, de Camargo Garcia M, Cohen M. Influence of knee position on the postural stability index registered by the Biodex Stability System. Gait Posture 2008; 28: 668-672.
- Rowe A, Wright S, Nyland J, Caborn DN, Kling R. Effects of a 2-hour cheerleading practice on dynamic postural stability, knee laxity, and hamstring extensibility. J Orthop Sports Phys Ther 1999; 29: 455-462.
- Berg K, Wood-Dauphinee S, Williams JI. The balance scale: reliability assessment with elderly residents and patients with an acute stroke. Scandinavian J Rehab Med 1995; 27: 27-36.
- Spendiff O, Longford NT, Winter EM. Effects of fatigue on the torque-velocity relation in muscle. Br J Sports Med 2002; 36: 431-435.
- Li JX, Hong Y. Kinematic and electromyographic analysis of the trunk and lower limbs during walking in negative-heeled shoes. J Am Podiatr Med Assoc 2007; 97: 447-456.
- Aydog E, Bal A, Aydog ST, Çakci A. Evaluation of dynamic postural balance using the Biodex Stability System in rheumatoid arthritis patients. Clin Rheumatol 2006; 25: 462.
- Rozzi SL, Lephart SM, Sterner R, Kuligowski L. Balance training for persons with functionally unstable ankles. J Orthop Sports Phys Ther 1999; 29: 478-486.
- Pincivero DM, Lephart SM, Henry T. Learning effects and reliability of the Biodex Stability System. J Athl Train 1995; 30): 35.
- Chen CL, Yeung KT, Wang CH, Chu HT, Yeh CY. Anterior ankle-foot orthosis effects on postural stability in hemiplegic patients. Arc Phys Med Rehab 1999; 80: 1587-1592.
- Larin H. Motor learning. theories and strategies for the practitioner; in Physical Therapy for Children (3rd Ed.). Saunders Elsevier Philadelphia PA 2006; 131-160.
- Schmidt RA, Wrisberg CA. Motor learning and performance: A situation-based learning approach. Human Kinetics 2008.
- Hooper TL, Dunn DM, Props JE, Bruce BA, Sawyer SF, Daniel JA. The effects of graded forward and backward walking on heart rate and oxygen consumption. J Orthop Sports Phys Ther 2004; 34: 65-71.
- Kramer JF. Backward walking: a cinematographic pilot study. Physiother Can 1981; 33: 77-86.
- Godde B, Voelcker-Rehage C. More automation and less cognitive control of imagined walking movements in high-versus low-fit older adults. Front Aging Neurosci 2010; 2.
- Kurz MJ, Wilson TW, Arpin DJ. Stride-time variability and sensorimotor cortical activation during walking. Neuroimage 2012; 59: 1602-1607.
- Yang JF, Gorassini M. Spinal and brain control of human walking: implications for retraining of walking. Neuroscientist 2006; 12: 379-389.
- Flynn TW, Soutas-Little RW. Mechanical power and muscle action during forward and backward running. J Orthop Sports Phys Ther 1993; 17: 108-112.
- Ung RV, Imbeault MA, Ethier C, Brizzi L, Capaday C. On the potential role of the corticospinal tract in the control and progressive adaptation of the soleus H-reflex during backward walking. J Neurophysiol 2005; 94: 1133-1142.
- Winter DA, Pluck N, Yang JF. Backward walking: a simple reversal of forward walking? J Mot Behav 1989; 21: 291-305.
- Grasso R, Bianchi L, Lacquaniti F. Motor patterns for human gait: backward versus forward locomotion. J Neurophysiol 1998; 80: 1868-1885.