ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2011) Volume 22, Issue 4
Evaluation of the effect of Guided Tissue Regeneration with or without te-tracycline root conditioning in the treatment of intrabony defects-A Clini-cal and Radiographic study
1Department of Periodontics and Community Dentistry, Dr. Ziauddin Ahmed Dental College, Aligarh Muslim Univer-sity, Aligarh
2Department of Oral & Maxillofacial surgery, Dr. Ziauddin Ahmed Dental College, Aligarh Muslim University,.
3Department of Community Medicine, Jawaharlal Nehru Medical College, Aligarh Muslim University, Aligarh
Accepted Date: June 2011
The present study was designed to comparatively evaluate the effect of G.T.R. with or with-out tetracycline root conditioning in the treatment of intrabony defects using a resorbable membrane. To achieve these aims, the following objectives were followed: Evaluation of pre surgical probing depths (PD) and it’s comparison post operatively. Comparison of the clini-cal attachment levels (CAL) pre surgically and post surgically. Assessment of the change in the overall area of the intrabony defect after the periodontal surgical treatment. The test group (n = 10) received resorbable barrier membrane with tetracycline root conditioning, while the control group (n=10) received the same membrane without tetracycline root condi-tioning for treating the intrabony defects. Both the treatment modalities resulted in a sig-nificant reduction in pocket depth and significant gain in both clinical attachment levels and bone levels post operatively after six months. Intergroup comparison of the parameters, re-vealed no statistically significant differences. Combining GTR. technique with the tetracy-cline root conditioning does not seem to improve the results following surgical treatment of intrabony defects.
Keywords
Guided tissue regeneration, tetracycline hydrochloride, root conditioning, resorbable membrane, intrabony defects.
Introduction
The main objective of traditional periodontal treatment is to resolve the inflammatory lesion in the periodontal tis-sues. This therapy involves the elimination of plaque and calculus from tooth surfaces, either with scaling and root planing alone or combined with periodontal surgery. With proper postoperative maintenance care, periodontal therapy results in resolution of gingival inflammation and in the arrest of disease progression. A contemporary goal of periodontal therapy, however, has become the regeneration of the lost attachment apparatus [1]
The first clinical device which allowed regeneration of cementum, periodontal ligament and alveolar bone was a cellulose acetate laboratory filter. The use of this filter paper provided the first human histological evidence of periodontal regeneration in response to guided tissue re-generation (G.T.R.) [2].
G.T.R. is based on the exclusion of gingival connective tissue cells and the prevention of the epithelial down-growth into the wound. By excluding epithelium, cells with regenerative potential (periodontal ligament, bone cells and possible cementoblasts) can enter the wound site first and promote regeneration [3]
Minabe [4] in a review study clarified the concept of methods to create an advantageous environment for periodontal regeneration using physical means, focusing on the method of selective tissue regeneration through nonre-sorbable or resorbable barriers and coronally placed flap technique.
It has been reported that periodontal ligament cells can be induced to proliferate and migrate on biochemically conditioned dentin surfaces [5]. This proliferation and movement have been shown to be increased when tetracycline is used to precondition the dentin surface. The tetracycline preconditioning of dentin removes the surface smear layer and partially demineralizes the dentin surface to expose collagen fibers [5].
Research has demonstrated, independently, the possible therapeutic values of tetracycline hydrochloride (TCN-HCl) conditioning of the root surfaces with the use of membranes for G.T.R. to enhance new connective tissue attachment on the root surface [6].
Thus, the present study was designed to comparatively evaluate the effect of G.T.R. with or without tetracycline root conditioning in the treatment of intrabony defects using a resorbable membrane.
To achieve these aims, the following objectives were followed:
1} Evaluation of pre surgical probing depths (PD) and it’s comparison post operatively.
2} Comparison of the clinical attachment levels (CAL) pre surgically and post surgically.
3} Assessment of the change in the overall area of the intrabony defect after the periodontal surgical treatment.
Materials and Method
Study population
For this study, subjects belonging to both the sexes and in the age group of 20-46 years were selected from the undergraduate clinic, Department of Periodontics. The in-clusion criteria was- patients displaying an interproximal intrabony defect in a posterior tooth, which was evident radiographically and manually probed ≥ 6mm. The exclu-sion group consisted of patients with any medical condi-tion contraindicating surgery, tooth mobility > 1mm, width of attached gingiva at defect site ≤ 1mm, furcation involvement and generalized horizontal bone resorption.
After pre-experimental treatment involving instructions in proper oral hygiene techniques, scaling and root planing and one month follow up period, the study involved twen-ty patients, with ten sites being treated with bioresorbable membrane and tetracycline root conditioning comprising the test group (group A), and another ten sites treated with bioresorbable membrane only comprising the control group (group B).
Pre-surgical preparation
A freshly prepared solution of 100 mg. of tetracycline powder dissolved in 1 ml. of distilled water, with a pH of 2 was taken [7] The bioresorbable membrane Healiguide® (Advanced Biotech Ltd. Chennai) available in the size of 15 X 20mm was cut into two halves of equal sizes (7.5 X 10mm) in the laminar flow unit and sealpacked in differ-ent eppendorff tubes, from where it could be taken out afterwards for the surgical procedure.
Surgical technique [3]
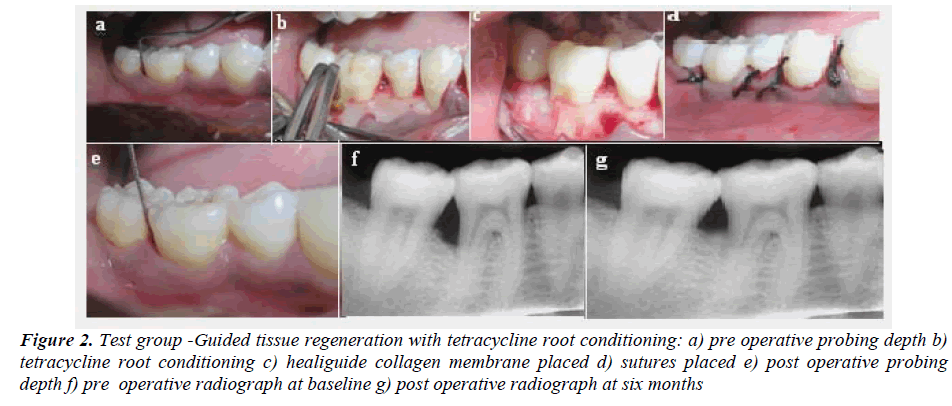
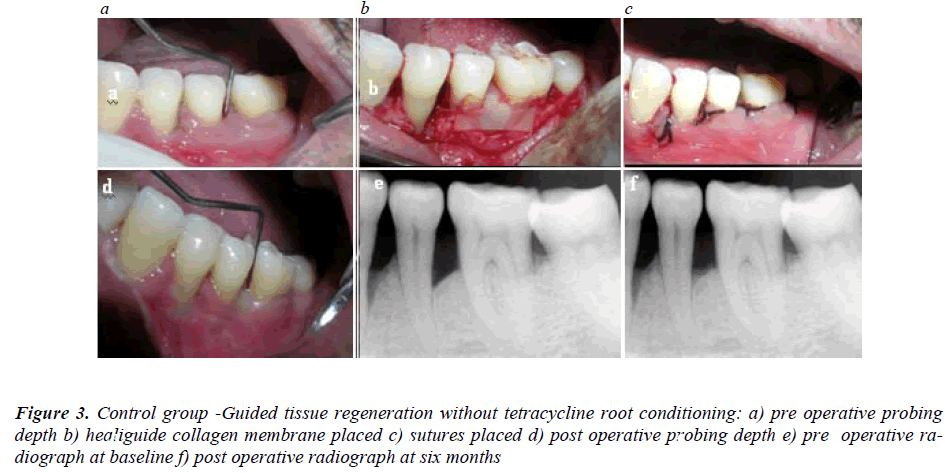
The area selected for surgery was anaesthesized with 2% xylocaine containing adrenaline 1:100,000 (Astra, Sweden). Initial incision was made away from defect, extend-ing at least one tooth mesial and distal to the tooth to be treated, so that closure was not directly over the defect. A full thickness mucoperiosteal flap was reflected 2-3mm beyond the defect. Apical to the mucogingival junction, a partial thickness flap was continued by blunt dissection to free the flap from tension. Granulation tissue was re-moved and curettes were used to root plan the tooth. Epi-thelium was removed from the inner side of the flap with a sharp curette. A template was prepared from autoclaved piece of mackintosh extending 2-3mm beyond the mar-gins of defect in all directions and the membrane was trimmed according to this template at the time of surgery. The flap was also trimmed where required to achieve primary tension free closure. Root conditioning was done only in Group A, with freshly prepared TCN-HCl solution for 3 minutes followed by generous irrigation with a ster-ile saline solution.(Figure no.2) The G.T.R. membrane was adapted in both group A and group B and sutured to the root surface by using a 5-0 resorbable suture. In cases where adequate adaptation was possible due to the defect anatomy, the membrane was adapted without the use of sutures using the pouch technique as advocated by Matt-son et al.[8]. The mucoperiosteal flap was repositioned to cover the membrane completely. The flaps were sutured with 3-0 silk suture. (Figure no.3)
Figure 2: Test group -Guided tissue regeneration with tetracycline root conditioning: a) pre operative probing depth b) tetracycline root conditioning c) healiguide collagen membrane placed d) sutures placed e) post operative probing depth f) pre operative radiograph at baseline g) post operative radiograph at six months
Post operative instructions
Following the surgery, antibiotic (Amoxicillin-500mg-thrice a day) and anti inflammatory drug (Diclofenac Potassium-twice a day) were prescribed for seven days. Warm salt water rinses for the first 2 weeks followed by Chlorhexidine digluconate 0.12% mouthrinse (10 ml twice a day) for four weeks were also advised. Subjects were instructed to refrain from mechanical oral hygiene measures for this period. At one week interval sutures were removed and subsequent follow up was done after an interval of 1 week, 1 month, 3 months and 6 months. The oral prophylaxis was performed at each recall appointment.
Parameters recorded
A. Clinical parameters
Probing depth (PD) and clinical attachment level (CAL) were measured at baseline, three months and six months postoperatively.
B. Radiographic parameters:
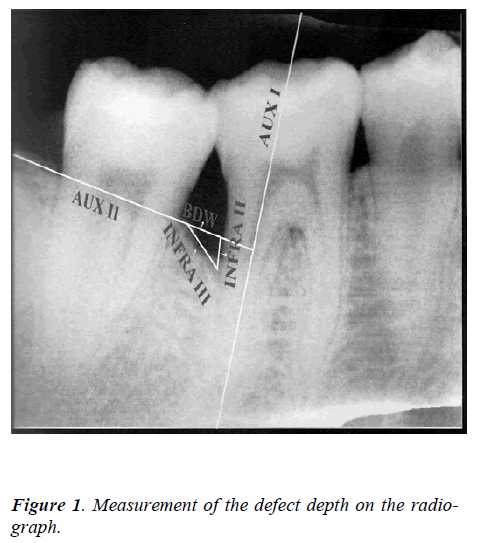
These were taken pre operatively at baseline and post operatively at 6 month time. Radiographic images were obtained in a digitized format by the RV3 digital radiography software version 305 Apeteryx Inc. In order to cali-brate measurement digitally the distance from the cusp tip to the cementoenamel junction was measured clinically after flap reflection and recorded. The same was meas-ured radiographically and all further radiographic meas-urements were calibrated according to this scale. The fol-lowing landmarks were identified on the radiographs :
• Cemento enamel junction (CEJ), if the CEJ was destroyed by restorative treatment, the apical margin of restoration was taken as a landmark.
• Bony defect was defined as the most coronal point where the periodontal ligament space showed a continuous width (BD).
• Alveolar crest was defined as the crossing of the silhouette of the alveolar crest with the root surface. (AC)
The intrabony component was assessed on the following parameters [9].
1. Infra I: Difference of the distance CEJ to BD mi-nus CEJ to AC.
2. Infra II: An auxillary line (AUX I) was drawn in the direction of the tooth axis. Then a second auxil-lary line (Aux II) perpendicular to the tooth axis was drawn through the most coronal extension of the lat-eral wall of the intrabony defect. Infra II was meas-ured from the point where AUX II crossed the con-tour of the root to BD.
3. BDW: i.e. the width of bony defect was meas-ured from the lateral margin of the intrabony defect to the point where AUX II crossed to root surface.
4. Infra III: The third side of the defect triangle was measured as Infra III i.e. the distance from BD to AC of the lateral wall of the defect.
5.
Defect area: calculated as Infra II X Infra III X BDW.
Osseous fill was calculated by subtracting the defect area preoperatively at baseline and postoperatively at six months. (Figure 1)
Statistical analysis
The difference between the preoperative baseline, three and six months postoperative measurements within each group were examined by using stu-dent’s unpaired t test.
Results
Throughout the study period, the patients maintained a good standard of supragingival plaque control. Statistically the following clinical and radiographic results were obtained:
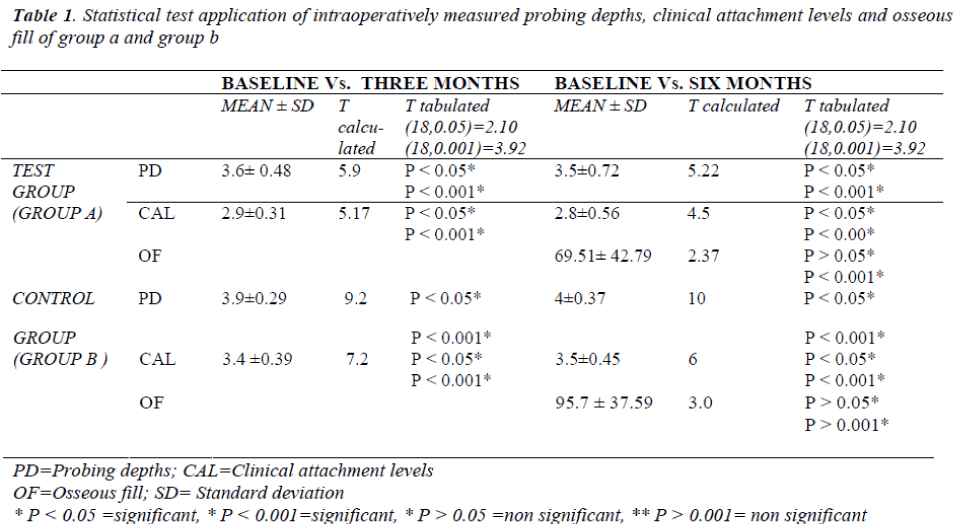
The findings suggested that the patients showed a reduc-tion in the pocket depths of the treated site after the sur-gery in both the test (group A) and the control (group B) groups. Gain in clinical attachment levels was also ob-served in both the groups. Moreover, it was seen that in both the groups, there was a decrease in the defect area after the treatment, thus reporting a favourable outcome of the therapy of G.T.R. (Table 1)
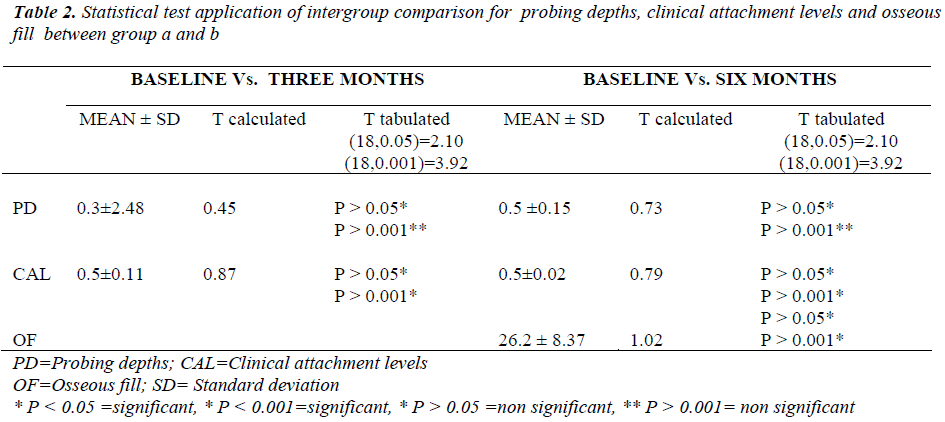
On comparing the treatment outcomes by applying the statistical unpaired “t” test to the probing depths, clinical attachment levels and osseous fill between the test and the control groups, it was observed that the difference in these parameters was not statistically significant. i.e. P > 0.05 and P > 0.001. (Table 2).
Discussion
The purpose of the present study was to comparatively evaluate the effect of G.T.R. with or without tetracycline root conditioning in the treatment of intrabony defects using a resorbable membrane.
It has been reported that selective repopulation of root surfaces previously exposed to periodontal disease by periodontal ligament cells results in formation of new connective tissue attachment, which is achieved by means of a biodegradable material interposed between the gingival tissue and the dental surface. [10] In this study collagen membrane was used because collagen mem-branes have the capacity to support regeneration of perio-dontal tissues and collagen membranes are either incor-porated within the healing tissues or degraded by these during the healing process. These properties of collagen membranes are of value in reconstructive periodontal therapy [11]
The results obtained in the study indicate that the use of the collagen membrane modified the modality of wound healing of the experimental sites with the formation of new cementum, bone and periodontal ligament. The im-provement in mean OHI – S score in the present study support the observed treatment effects obtained under a strict plaque control regimen. It is in confirimity with the study of Cortelleni et al [12] who explained that the long term clinical trials have demonstrated that good clinical results can be obtained and maintained over time only if an optimal plaque control regimen is instituted. Con-versely, deterioration of the root hygiene levels result in impairment of obtained therapeutic effect.
Real comparison of treatment outcomes by GTR is a little difficult because of the variation in data collection meth-ods among the published studies. Some studies state that the deepest site of the defect was measured [13] while others state that the sites were averaged [14] and still oth-ers do not specifically state the method of data collection [12].
It is clear that regenerative clinical trials require standardization of data analysis so that valid comparison between studies can be made (This study presented data as the average of all sites encompassing the defect). Consid-ering these factors the following observations compare the results of this study with those reported in the literature.
The patient inclusion criteria in the present study was the presence of at least one proximal area with a residual pocket depth, ≥ 6 mm and an associated intrabony defect confirmed by pretreatment radiograph. The resulting date compared favorably to those reported by earlier workers [15,19].
These studies demonstrated PD reduction, CAL gain and bone fill almost same as that obtained in the present study. These findings can be explained on the basis of the similarities in pretreatment PD, CAL and the intrabony component of the osseous defects which was almost simi-lar to the values reported in the these studies [15] [9]. These workers have explained the importance of selection of the defect site as well as the patient oral hygiene per-formance, smoking etc. in treatment outcomes.
Cortellini et al [12] stratified the baseline data obtained in 1993 publication according to CAL gained after GTR treatment Those sites which achieved less than 2 mm of attachment gains were observed to have PD and CAL similar to those found in our study. Thus, if one was to compare only those sites which had comparable defect dimension prior to surgical therapy, similar treatment re-sults would be found.
In the present study in the test group, treated with barrier membrane and TCN-HCl root conditioning, reduction in PD, CAL gain and defect fill was 4.0mm, 3.5 mm and 1.61 mm respectively. These results are somewhat better in comparison to Kersten et al [14] who reported reduc-tion in PD 1.8mm, CAL gain 0.8mm and defect fill 1.7 mm. They had also concluded that root conditioning did not show any improvement over ePTFE membranes.
Nagata et al [16] treated surgically created dehiscence defects on buccal aspect of lateral incisors in adult male monkeys by flap surgery with and without tetracycline root conditioning. Computer assisted histometric analysis was used to evaluate the formation of new cementum, new bone and new connective tissue attachment and length of epithelium. No statistically significant differ-ence was observed between the two groups. The results were almost same as have been shown in our study.
The similarity in the results with other reports can be ex-plained on the basis of that the clinical effect of the acid conditioning may have been overshadowed by the healing potential generated by the barrier membrane.
It was also suggested that the nonsignificant difference between treatment modalities could be because of, that both modalities draw upon similar regenerative mecha-nisms in the periodontium i.e. favoring a specific line of cells, which makes a synergistic effect an unlikely result.
Thus, the combined effect of the two is that of the one with the best effect. (non synergistic effect).[17]
Root conditioning with 10mg/ml. of TCN-HCl for 4 min-utes resulted in smear layer removal, opening of dentinal tubules and exposure of collagen fibrils. Evidence sug-gests that high concentration of tetracycline in the tissues may impair the initial stages of wound healing, preventing the formation of new periodontal connective tissue attachment [12].
It has been reported that the use of TCN-HCl to enhance new attachment formation in vivo is observed only with the use of low concentrations of the solution. Also, it has been shown that root surface demineralization can be increased by repeated application of demineralizing agents.[18] Therefore, if thorough demineralization is an important factor in exposing collagen for enhanced periodontal regeneration, the use of a low TCN-HCl concentra-tion (10-20 mg/ml.) with repeated application and a longer total application time is recommended. The subjects did not show significant improvement for osseous fill in the present study.
Finally, it can be suggested that the success of GTR in the treatment of intrabony defects may not be related to the type of barrier device used. The device must accomplish the necessary functions of excluding the gingival connec-tive tissue and gingival epithelium from the defect area, maintain space within the defect for blood clot formation and growth of progenitor cells from the surrounding peri-odontal ligament and bone.[10] Factors other than barrier composition may play a more significant role in affecting the regenerative responses to GTR. Any or all of the fol-lowing factors may influence periodontal regeneration: depth and width of the defect and attachment level prior to treatment, thickness of the gingival flap, membrane exposure with accompanying plaque accumulation, cov-erage of the newly regenerated tissues, smoking habits, quality of the recall maintenance programme, periodontal history of the affected tooth, healing response of the sub-ject and clinicians’ surgical skill. The decision to treat a defect with a regenerative technique must be based on consideration of these factors, which in turn will deter-mine the predictability of a successful result.
References
- Caton J, Greenstein G, Zappa U. Synthetic Bioab-sorbable Barrier for Regeneration in Human Perio-dontal Defects. J Periodontol 1994; 65: 1037-1045
- Tatakis DN, Promsudthi A and Wikesjö UME: De-vices for Periodontal Regeneration. Periodontology 2000, 1999; 19: 59-73
- Wang HL, Cooke J. Periodontal Regeneration Tech-niques for Treatment of Periodontal Diseases. Dent Clin N Am 2005; 49: 637-659
- Minabe M. A Critical Review of the Biologic Ration-ale for Guided Tissue Regeneration. J Periodontol 1991;62: 171-179
- Terranova V, Hic S, Franzetti L, Lyall R, Wikesjö U. A Biochemical Approach to Periodontal Regenera-tion. AFSCM: Assays for Specific Cell Migration. J Periodontol 1987; 58: 247-257
- Dyer BL, Caffesse RG, Nasjleti CF, Morrison EC: Guided Tissue Regeneration With Dentin Modifica-tion. J Periodontol 1993; 64: 1052-1060
- Trombelli L, Scabbia A, Zangari F, Griselli A, Wikes-jo UME, Calura G. Effects of Tetracycline HCL on Periodontally Affected Human Root Surfaces. J Pe-riodontol 1995; 66: 685-691
- Mattson JS. Lanny LM, Mansoor HJ. Treatment of Intrabony Defects With Collagen Membrane Barri-ers. Case Reports. J Periodontol 1995; 66: 635-645
- Eickholz P, Horr T, Klein F, Hassfeld S, Kim TS: Ra-diographic parameters for prognosis of periodontal healing of infrabony defects: two different definitions of defect depth. J Periodontol 2004; 75: 399-407.
- Scantlebury TV. A Decade of Technology Develop-ment for Guided Tissue Regeneration. J Periodontol 1993; 64: 1129-1137.
- Pitaru S, Tal H, Soldinger M, Grosskopf A, Noff M: Partial Regeneration of Periodontal Tissues Using Collagen Barriers-Initial Observations in the Canine. Journal Periodontol 1988; 380-386.
- Cortellini P, Pini Prato G and Tonetti MS: Periodontal Regeneration of Human Infrabony Defects. I. Clini-cal Measures. J Periodontol 1993;64:254-260
- Weltman R, Trejo PM, Morrison E, and Caffesse R: Assessment of Guided Tissue Regeneration Proce-dures in Intrabony Defects With Bioabsorbable and Non-Resorbable Barriers. J Periodontol 1997;68:582-591
- Kersten BG, Chamberlain ADH, Khorsandi S: Heal-ing of the Intrabony Periodontal Lesion Following Root Conditioning With Citric Acid and Wound Clo-sure Including Expanded ePTFE Membranes. J Pe-riodontol 1992; 63:876?882.
- Aimetti M, Romano F, Pigella E, Pranzini F and De-bernardi C: Treatment of Wide, Shallow And Pre-dominantly 1 Wall Intrabony Defects With a Bioab-sorbable Membrane. A Randomized Controlled Clin-ical Trial .J Periodontol 2005;76: 1354-1361
- Nagata MJH, Basco AF, Leite CM, Luiz GN Melo, Maria LMM, Feld S: Healing of Dehiscence Defects Following Root Surface Demineralization With Tet-racycline: A Histologic Study in Monkeys. J Perio-dontol 2005; 76: 908-914
- Machtei EE, Dunford RG, Norderyd OM, Zambon JJ and Genco RJ: Guided Tissue Regeneration and Anti-Infective Therapy in the Treatment of Class II Furca-tion Defects. J Periodontol 1993; 64: 968-973.
- Madison JS, Hokett SD. The effect of different tetra-cyclines on the dentin root surface of instrumented, periodontally involved human teeth: A Comparative Scanning Electron Microscope study. J Periodontol. 1997; 68: 739-745.