ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 7
Evaluation of patients requiring surgical intervention in tuberculosis: A clinical study
Muharrem Cakmak*, Atilla Durkan, Mustafa Yilmaz and Mehmet Cagri Goktekin
Thoracic Surgery Clinic, Gazi Yasargil Education and Research Hospital, Diyarbakir, Turkey
- *Corresponding Author:
- Muharrem Cakmak
Thoracic Surgery Clinic
Gazi Yasargil Education and Research Hospital
Turkey
Accepted date: December 06, 2016
Introduction: Tuberculosis (TBC) is one of the most common forms of pleurisy, pleural effusion and extra pulmonary TBC. Tube thoracostomy is the primary treatment method in massive TBC pleurisy. On the other hand, video-Assisted Thoracoscopic Surgery (VATS) has come to the fore in the diagnosis and treatment of undiagnosed patients. In this study, our aim is to share the results of surgeries in patients with pleural effusion due to TBC or diagnosed with TBC later.
Materials and Methods: Files of patients were analysed retrospectively. Age, gender, symptoms, vital signs, laboratory finding, location of disease, diagnosis, surgical procedure, complications, length of stay, mortality and morbidity were examined. The effects of gender, location of the disease, fluid properties, and surgical procedures on TBC pleurisy were evaluated. The patients treated with surgery were enrolled in the study. Patients who were performed anti-TBC treatment even if they had pleural effusion, underwent relaxing thoracentesis, and did not undergo surgery were excluded from the study. The treatment method which yielded favorable results in surgery was taken into consideration. Tube thoracostomies performed before VATS applications were excluded. Results were analysed using Mann- Whitney U test, Fisher exact test and Multivariate linear regression analysis. P<0.05 was considered significant.
Findings: Sixty-four patients with TBC diagnosed through VATS or thoracotomy and treated with tube thoracostomy were examined. Male gender, right localization and exudative pleural effusion were found to have a significant effect on the development of TBC pleurisy (P<0.05). Furthermore, it was found that tube thoracotomy were more effective in the treatment of TBC pleurisy (P<0.05).
Results: The primary treatment method for TBC pleurisy is tube thoracostomy. Additionally, VATS, which is successful in diagnosis and treatment of undiagnosed TBC, is safe, effective and minimally invasive procedure.
Keywords
Pleurisy, Thoracoscopy, Thoracostomy, Tuberculosis
Introduction
Tuberculosis (TBC) is one of the most common forms of pleurisy [1]. It may occur soon after primary TBC or in 6-12 weeks after primary TBC infections. Delayed type hypersensitivity reaction caused by bacilli that reaches the pleural cavity through lymphatic or haematogenous ways is the main reason of TBC [2]. The incidence is 4-20% in patients with TBC [3]. The main symptoms are fever, chest pain and cough. Other symptoms are fatigue, night sweats, weight loss and dyspnoea. The degree of dyspnoea depends on the amount of accumulated fluid [4]. Diagnosis is made through laboratory examinations, radiological and surgical procedures [1,2,5]. Medical procedures are the primary treatment methods in patients with TBC pleurisy. Even if the patients are not treated, patients may recover spontaneously within a few weeks or months. However, the likelihood of having active tuberculosis in 5 years is high in those patients. Furthermore, residual pleural thickening rate is around 55% [2]. The primary method to relieve breathing in patients diagnosed with massive tuberculosis pleurisy is tube thoracostomy. On the other hand, a number of applications are insufficient for diagnosis and treatment in undiagnosed patients. In these cases, videoassisted thoracoscopic surgery (VATS), which provides the opportunity to receive comprehensive pleural imaging and a sufficient amount of biopsy, has come to the fore. VATS is a highly effective surgical method in the diagnosis and treatment of lung parenchyma, pleura, mediastinum, the main vascular structures and diaphragmatic pathologies [5]. In patients with pulmonary collapse and loculations, thoracotomy is another option. But it is not very preferred due to high complication rates [5]. In this study, we aimed to share the demographic characteristics and surgical methods of patients with TBC pleurisy.
Materials and Methods
Patients
Sixty-four patients suspected or diagnosed with pleurisy and treated with surgical methods in our clinic from 2004-2015 participated in the study.
Procedures: Files of patients were analysed retrospectively. Age, gender, symptoms, vital signs, laboratory findings (leukocyte (WBC), haemoglobin (HB), haematocrit (HTC), sedimentation (sedim), total protein (TP), albumin (ALB), adenosine deaminase (ADA), transudate, exudates), location of disease, diagnosis, surgical procedure, complications, length of stay, mortality and morbidity were examined. The effects of gender, location of the disease, fluid properties, and surgical procedures on TBC pleurisy were evaluated.
Inclusion and exclusion criteria
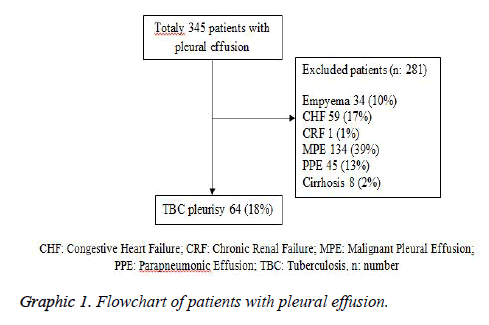
The patients treated with surgery (therapeutic tube thoracostomy, therapeutic or diagnostic thoracotomy or VATS) were enrolled in the study. Patients who were performed anti- TBC treatment even if they had pleural effusion, underwent relaxing thoracentesis, and did not undergo surgery were excluded from the study. The treatment method which yielded favourable results in surgery was taken into consideration. Tube thoracostomies performed before VATS applications were excluded as they changed the number and rate. Flowchart is shown in graphic 1.
Statistical analysis
Data were analysed by Statistical Package for the Social Sciences (SPSS 21, Chicago, IL, USA). Kolmogorov-Smirnov and Shapiro-Wilk tests were used as tests of normality for continuous variables. Parametric data, non-parametric data and categorical data were expressed as mean ± standard deviation and n (%) respectively. Mann-Whitney U test was used for pairwise comparison of data without normal distribution. Fisher exact test was used for non-parametric and categorical data. Additionally, Multivariate linear regression analysis was used to determine the relationship between variables. P<0.05 was considered significant.
Results
Between the years 2004-2014, the number of pleural effusion patients treated with surgical methods in our clinic was 345, while the number of patients with TBC pleurisy was 64 (18.55%). The rate was found as 5.39. The mean age of patients was 44.5 ± 16.6. Forty-five (70%) were male and 19 (30%) were female. It was discovered that TBC pleurisy was more common in males according to women. Additionally, male gender was significantly in the development of TBC pleurisy (p=0.002) Disease was located on the right in 43 (67%) patients, whereas it was on the left in 21 (33%). Right localization was found to be significantly in TBC pleurisy (P=0.008). Three of effusion (5%) were transudative, while 61 (95%) were exudative. In TBC pleurisy, pleural effusion's being exudative was statistically significant (P=0.0001) (Table 1).
| Parameters | Values | P* |
|---|---|---|
| Number | 64 | |
| Gender (Male/Female) | 45 (70.3%)/19 (29.7%) | 0.002 |
| Age | 28.23 ± 12.96 | |
| Leucosyte count | 8879.69 ± 3254.55 | |
| Hemoglobin | 11.7 ± 1.34 | |
| Hematocrit | 37.07 ± 3.44 | |
| Sedimentation | 40.11 ± 14.16 | |
| Pleural total protein | 7.65 ± 2.14 | |
| Pleural albumin | 4.05 ± 1.24 | |
| Pleural ADA | 58.26 ± 7.54. | |
| Effusion type (Exudate/Transuda) | 61 (95.3)/3 (4.7) | 0.0001 |
| Localization (Right/Sol) | 43 (66.2%)/21 (23.8%) | 0.008 |
| Anesthesia (Local/General) | 46 (71.9%)/18 (28.1%) | 0.0001 |
| Cerrahi (VATS/ Thoracotomy) n (%) | 14 (77.8%)/4 (22.2%) | 0.031 |
| *P: Fisher’s exact test; ADA: Adenosine Deaminase; VATS: Video Assited Thoracoscopic Surgery; n: number | ||
Table 1: Demographic distrubation of patients.
In laboratory examinations, it was found that the mean of WBC was 8879.69 ± 3254.55, HB was 11.7 ± 1.34, HTC was 37.07 ± 3.44, sedim was 40.11 ± 14.16, TP was 7.65 ± 2.14, ALB was 4.05 ± 1.24, and ADA was 58.26 ± 7.54 (Table 1). Furthermore; according to results of Mann-Whitney U test analysis, haemoglobin and haematocrit levels were found to be significant in patients undergoing VATS and thoracotomy (general anaesthesia) according to tube thoracostomy (local anaesthesia) (p =0.001, (Table 2). The most common symptoms of patients were cough (n=48.75%), chest pain (n=45.70%), fever (n=39.61%), and dyspnoea (n=22.34%). Other symptoms were fatigue (n=15.23%), palpitations (n=14.22%), nausea and vomiting (n=8.13%).
| Parameters | Local anesthesia (Tube thoracostomy) | General anestehesia (VATS and Thoracotomy) | p |
|---|---|---|---|
| Number | 46 | 18 | 0.0001 |
| Gender (Male/Female) | 30/16 | 15/3 | 0.226* |
| Age | 28.11 ± 13.94 | 28.56 ± 10.39 | 0.902** |
| Leucosyte conut | 8843.48 ± 3494.61 | 8972.22 ± 2629.43 | 0.875** |
| Hemoglobin | 11.35 ± 1.27 | 12.61 ± 1.04 | <0.001** |
| Hematocrit | 36.11 ± 3.21 | 39.56 ± 2.75 | <0.001** |
| Sedimentation | 41.85 ± 12.88 | 35.67 ± 16.58 | 0.117** |
| Localization (Right/Left) | 30/16 | 13/5 | 0.769*** |
| Effusion type ((Exudate/Transuda) | 43/3 | 18/0 | 0.553*** |
| *P: Nonparametric binominal test; **P: Mann-Whitney U test; ***P: Fisher’s exact test; VATS: Video assited thoracoscopic surgery | |||
Table 2: Comparison of patients who underwent tube thoracostomy and vats or thoracotomy.
The first diagnostic method used in patients was chest radiography. The second method preferred was computed thoracic tomography. It was observed that ultrasonography (USG) was used less than the other two methods. The most common concomitant diseases were diabetes and diseases related to mental retardation. In treatment, it was found that 46 patients with tuberculosis pleurisy (72%) underwent tube thoracostomy, 14 (22%) underwent VATS, and 4 (6%) were applied thoracotomy. It was seen that tube thoracostomy was primary and the most effective treatment method in TBC pleurisy (P=0.0001). When VATS and thoracotomy are compared, It was seen that VATS was the most effective diagnosis and treatment in TBC pleurisy according to thoracotomy (P=0.031). In patients who cannot diagnose by other methods, VATS was accepted as prior surgical method for both diagnosis and treatment (Table 1).
According to results of multivariate linear regression analysis, a significant correlation was found between general anaesthesia and HTC values (p=0.01), Standardized regression coefficient beta=0.477, 95% Confidence Interval (CI)= 0.226-0.639), R2=0.206, t=4.183 and male patients (p=0.025, Standardized regression coefficient beta=0.255, 95% Confidence Interval (CI) =-0.33 -0.469), R2=0.270, t=-2.518). The most common postoperative problems in patients were expansion defect and atelectasis. However, no mortality was observed. The average length of stay was 6 ± 2.5 days.
Discussion
Tuberculosis pleurisy is one of the most common forms of pleural effusion and extra pulmonary tuberculosis in many countries [1]. It was reported in various studies that the incidence was higher than prevalence of tuberculosis and reported to develop around 4-20% in patients with tuberculosis [3,6]. In this study, the rate of patients with TBC pleurisy was 18.55% and the rate was found as 5.39. The incidence of tuberculosis pleurisy varies according to geographic region and immunity. The status of the immune system is an effective factor as hypersensitivity reaction is one of the main hypotheses regarding to disease. The reaction is seen 2-3% in the United States, 20-25% in Africa, 11% in patients with suppressed immune system, and about 20-38% in HIV-positive patients [7]. In the present study, the most common associated diseases were diabetes and mental retardation.
Tuberculosis pleurisy is clinically acute and sub-acute. Additionally fever, chest pain, cough are seen in more than half of patients. Fatigue, night sweats, weight loss, haemoptysis, and dyspnoea are the other symptoms [8,9]. The most common symptoms of our patients were cough (n=48), chest pain (n=45), fever (n=39), and dyspnoea (n=22). Other symptoms were fatigue (n=15), palpitations (n=14), nausea and vomiting (n=8). Acute disease is more common in young patients having high immunity. Symptoms imitate pneumonia. However, leukocytosis is not seen. The fluid is usually one-sided, moderate or less and loculated. Long-term symptoms are encountered in the elderly. Even if the disease is not treated, patients heal spontaneously within a few weeks or months. However, the likelihood of having active tuberculosis in 5 years is high. Pleural thickening rate is around 55% [2].
In the diagnosis of effusions, chest radiography, computed tomography, thoracic ultrasound and magnetic resonance imaging are the main methods. At standard chest x-ray, fluid is usually unilateral and moderate. Massive fluid is rare. Effusion may be accompanied by nodules, fibrosis at the apex, hilar, and paratracheal and mediastinal lymphadenopathy. Computed tomography is very use for demonstrating pleural effusion, thickening, parenchymal nodules, lymphadenopathy and parenchymal tuberculosis. On the other hand, magnetic resonance imaging is useful in the distinction between malignancy and infection [2]. The main diagnostic methods used in our patients were lung X-rays and computed tomography.
In the diagnosis of tuberculosis pleurisy, the first procedure to be applied is to take samples from fluid and examine biochemically and microbiologically, and search for ARB (acid-fast bacilli) in sputum and fluid. ADA from fluid must be studied. When the cut-off value of ADA is accepted as 40 U/L, specificity becomes 90% and sensitivity becomes 92% for the diagnosis of tuberculosis pleurisy. It was reported that TBC did not develop in patients with effusion having low ADA level and high lymphocytes during the 5-year follow-up. If ADA level is 70 U/L and above, and lymphocyte/neutrophil level is over 0.75, there is a high possibility of developing TBC pleurisy. Additionally, if lymphocyte/neutrophil ratio is>0.75 while ADA level is 40-70 U/L, there is the likelihood of TBC pleurisy. Also high number of ADA, and low C - reactive protein levels have a diagnostic value over 90%. In TBC pleurisy the amount of protein may be 5 g/dL, lactate dehydrogenase levels may be more than serum levels, lower than glucose levels, and may be around pH 7.30 or less. In cytological examination, lymphocyte predominance existed about 50-90% [1,4,10,11]. In our study, the mean WBC was 8879.69 ± 3254.55, HB was 11.7 ± 1.34, HTC was 37.07 ± 3.44, sedim was 40.11 ± 14.16, TP was 7.65 ± 2.14, ALB was 4.05 ± 1.24, and ADA was 58.26 ± 7.54.
In some patients, sputum, cytological study of the pleural fluid, laboratory tests such as culture seeding and ADA level, or pathological examination of materials obtained through closed pleural biopsy may be inadequate for diagnosis. This group of patients who cannot be diagnosed constitutes 20-40% of patients with pleural effusion [5]. The causes of this situation may be the small number bacilli in sputum or pleural fluid, or pleural biopsy which cannot point to infected nodules. In most of these cases which cannot diagnosed and treated, serious parenchymal disease may develop in the near future. The most extensive area of VATS application is pleural effusion. VATS is a surgical method which allows thoracic manipulation with a few small skin incisions, accompanied by video imaging, performed with specially designed endoscopic instruments. Additionally, it is safe and minimally invasive surgical procedure that increases the postoperative patient comfort [5]. Undiagnosed patients with TBC pleurisy should be evaluated through VATS. Moreover, VATS will provide detailed information about lung parenchyma, mediastinal structures, main vascular formations and diaphragmatic [5]. In this study, fourteen patients were diagnosed and treated with VATS.
In the treatment of tuberculosis pleurisy, the main objective is to prevent the emergence of active tuberculosis, eliminating symptoms, and preventing the development fibrothorax. Pleural thickening is seen in 50% of patients despite the treatment. Loculations the pleural fluid, low glucose and high LDH are the risk factors for active tuberculosis [12]. Draining the fluid without diagnosis does not benefit in the long term. However, therapeutic drainage is recommended in patients with severe dyspnoea. In 1/4 of patients, thickening more than 1 cm occurs after treatment. There are some studies showing that fibrinolytic application reduces pleural thickening [13,14].
Recently, VATS and medical thoracoscopy have been compared. Medical thoracoscopy can be performed without general anaesthesia and outside the operating room and often provides enough information for the diagnosis. On the other hand, despite its risk of general anaesthesia, VATS allows therapeutic intervention in addition to the diagnostic usage. This aspect is superior to medical thoracoscopy [15]. Although surgical methods have a limited importance for the treatment of active pulmonary tuberculosis, they are able to play an integral role in the loculated fluid and some cases. VATS is a favourable method in terms of removal of pleural adhesions, performing a partial decortication, the removal of the pouch, ensuring the lung expansion, minimal morbidity, pain control and patients' stress [16]. Thoracotomy should be preferred if intense localization, lung trapping, and pleural fistulas are present. In our study, tube thoracostomy was sufficient for drainage of fluid inpatients diagnosed TBC pleurisy, whereas VATS and thoracotomy contributed 28% in undiagnosed patients developing loculations, experiencing expansion difficulties due to adhesions and requiring decortication.
As a result, Tube thoracostomy was primary and the most effective treatment and diagnosis method in TBC pleurisy. When VATS and thoracotomy are compared, it was seen that VATS was the most effective diagnosis and treatment in TBC pleurisy according to thoracotomy. In patients who cannot be diagnosed by other methods, VATS was accepted as prior surgical method for both diagnosis and treatment.
Study Limitation
The retrospective nature of the work constitutes a fundamental limitation. Other limiting factors were the absence of patient control information, the absence of medical treatment periods, Lack of sociocultural features, No family story and some patients do not have laboratory tests.
References
- Light RW. Update on tuberculosis pleural effusion. Respirology 2010; 15: 451-458.
- Udwadia ZF, Sen T. Pleural tuberculosis: an update. Curr Opin Pulm Med 2010; 16: 399-406.
- Seiscento M, Vargas FS, Rujula MJ, Bombarda S, Uip DE, Galesi VM. Epidemiological aspects of pleural tuberculosis in the state of Sao Paulo, Brazil (1998-2005). J Bras Pneumol 2009; 35: 548-554.
- Özdülger A, Uluba? B. Plevrale füzyonlar ve plevra tüberkülozu. In: Yüksel M, Balc? AE, editors. Gö?üs Cerrahisi. ?stanbul, Turkey: Nobel T?p Kitabevi; 2015. Pp. 529-539.
- Kürkçüo?lu C, Karao?lano?lu N, Ero?lu A, Ünlü M. Plevral efüzyonlarda videotorakoskopi: 47 olgunun de?erlendirilmesi. Türk Gö?üs Kalp Damar Cer Derg 2000; 8: 712-714.
- Baumann MH, Nolan R, Petrini M, Lee YC, Light RW, Schneider E. Pleural tuberculosis in the United States: incidence and drug resistance. Chest 2007; 131: 1125-1132.
- Queipo JA, Broseta E, Santos M, Sánchez-Plumed J, Budía A, Jiménez-Cruz F. Mycobacterial infection in a series of 1261 renal transplant recipients. Clin Microbiol Infect 2003; 9: 518-525.
- Yataco JC, Dweik RA. Pleural effusions: Evaluation and management. Clevel and Clinic Journal of Medicine 2005; 72: 854-872.
- Porcel JM, Light RW. Pleural effusions: Diseases-a-month 2013; 59: 29-57.
- Porcel JM, Alemán C, Bielsa S, Sarrapio J, Fernández de Sevilla T, Esquerda A. A decision tree for differentiating tuberculosis from malignant pleural effusions. Respir Med 2008; 102: 1159-1164.
- Daniil ZD, Zintzaras E, Kiropoulos T. Papaioannou AI, Koutsokera A, Kastanis A. Discrimination of exudative pleural effusions based on multiple biological Parameters. EurRespir J 2007; 30: 957-964.
- Candela A, Andujar J, Hernández L, Martín C, Barroso E, Arriero JM, Romero S. Functional squeal of tuberculosis pleurisy in patients correctly treated. Chest 2003; 123: 1996-2000.
- Porcell JM, Rubio-Caballero M. Squeal of tuberculosis pleural effusion. Med Clin 2005; 124: 494-496.
- Han DH, Song JW, Chung HS, Lee JH. Resolution of residual pleural disease according to time course in tuberculosis pleurisy during and after the termination of antituberculosis medication. Chest 2005; 128: 3240-3245.
- Dikensoy Ö. Plevra hastal?klar?nda tan?. Journal of Clinicaland Analytical Medicine 2010; 1: 1-3.
- Beshay M, Dorn P, Kuester JR, Carboni GL, Gugger M, Schmid RA. Video thoracoscopic surgery used to manage tuberculosis in thoracic surgery. Surg Endosc 2005; 19: 1341-1344.