ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 5
Evaluation of determinants of acute kidney injury and mortality among patients attending intensive care unit: A retrospective study
Department of Intensive Care Unit, the Affiliated Yancheng Hospital of Southeast University Medical College, Yancheng Third People's Hospital, Yancheng 224001, Jangsu Province, PR China
- *Corresponding Author:
- Qi- Yin Zou
Department of Intensive Care Unit
The Affiliated Yancheng Hospital of Southeast University Medical College
Yancheng Third People's Hospital, PR China
Accepted date: October 26, 2016
Introduction: Acute Kidney Injury (AKI) in intensive care unit (ICU) portends worse outcomes and attendant with high mortality. Early identification of high risk patients can improve their outcomes and may reduce ICU mortality rate.
Methodology: A retrospective data review of patient attending ICU during 1 year was performed. All the patients were divided into two groups based upon their outcomes (AKI/non-AKI, fatal/non-fatal cases). Risk factors of AKI and mortality were identified by using regression analysis.
Results: A total 906 patients (mean age: 53.6 ± 15.3, male: 58.2%) were included into the study. The mean length of ICU stay was 14.4 ± 3.3 days. AKI was observed in 487 (53.8%) patients with varying severity including AKIN-I in 89/487 (18.3%), AKIN-II in 137/487 (28.2%) and AKIN-III in 261/487 (53.5%) cases. Old age (OR 2.8) diabetic patients (OR 1.9) with high SOFA (OR 2.7) and APACHE-II scores (OR 3.1) requiring IMV on admission (OR 4.2) were found to be significantly associated with AKI. Overall mortality in our study was 29.5%. Pulmonary (OR 1.7) and neurological (OR 3.3) causes of ICU admission, AKI (OR 6.2), AKIN-III (OR 3.2), high SOFA (OR 1.6) and APACHE II scores (OR 2.3), need of IMV (OR 7.2) and dialysis (OR 4.6) were significant predictors of mortality in our study.
Conclusion: AKI was found among half of the patients attending ICU and significantly associated with in hospital mortality. Early identification of high risk patients can be useful to reduce the burden of AKI and mortality in ICU.
Keywords
Acute kidney Injury, Glomerular filtration rate.
Introduction
Acute Kidney Injury (AKI), previously known as acute renal failure (ARF), is described as sudden decline in renal function and glomerular filtration rate (GFR) that may cause wide range of clinical manifestations due to accumulation of nitrogenous metabolites and water/electrolyte disturbances [1]. It has been estimated that 5% to 20% patients attending intensive care unit (ICU) experience at least one episode of AKI with multiple organ failure (MOF) [2].
A wide variation in incidence, characteristics and risk factors of AKI has been observed across published literature that might be contributed to methodological differences and lack of consensus to define AKI [3-6]. AKI is more prevalent in hospital (4.9% to 7.2%) than in community (0.4% to 9%) while incidence of AKI in ICU ranges from 20% to 40% depending upon presence and severity of comorbid illnesses [7]. About 80% patients with AKI in ICU died and among those who survived, 13% require dialysis [8]. More recently AKIN and RIFLE criteria were introduced in an attempt to identify early cases of AKI and to homogenize research findings so that they can be compared to draw firm conclusions [9]. Despite of several measures to combat this highly morbid and fatal complication in ICU, the incidence rates and mortality remained virtually unchanged.
More recently, it has been proposed that the patients who survived an episode of AKI have significant risk for progression to advanced stages of chronic kidney disease (CKD) that may further increase global burden of CKD [10]. AKI is a multifactorial syndrome which can be categorized into pre-renal, intrinsic/renal and post-renal based upon location of renal insult. Sepsis is considered major causative factor of AKI among critically ill patients, accounting for nearly 50% of cases [11,12]. Several efforts have been made to evaluate incidence, characteristics and risk factors of AKI as well as mortality in ICU [13,14] but more studies from different regions of the world are still needed.
Current study was aimed to evaluated determinants of AKI and mortality among patients attending ICU. This study will also supplement previously published literature in China [15-18].
Methodology
Ethical approval
Written ethical approval to conduct current study was obtained from committee of research on human being of Yancheng hospital of Southeast University Medical College Hospital. Waiver of consent form was granted by said committee due to retrospective nature of study.
Study population
A retrospective study was conducted on patients attending ICU of Yancheng hospital of Southeast University Medical College Hospital during the period of 1 year (January 2014 - Dec 2014). During the defined study period, a total 1866 patients were admitted to ICU. Patients with ICU stay <48 hours (n=256), those who were readmitted to ICU (n=87), patients admitted after uncomplicated surgery (n=104), those having CKD requiring dialysis (n=131) and having incomplete data (n=381) were excluded from the study. Total 906 patients having age >18 years were included in final analysis.
Data collection
Demographic, laboratory and outcome data for all the included patients were recorded by using structured data collection form. All the data were retrieved via patient`s record file and hospital online database. Patient`s having missing data that was necessary for the current study were excluded e.g. serum creatinine, renal and liver function tests etc. All the data were collected from their ICU admission to discharge or death, whichever occurred first. All possible efforts were made to find required patient`s information in order to avoid missing data.
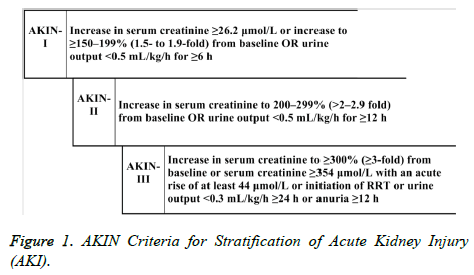
Definition of AKI
Patients with AKI were identified by using AKIN criteria [9] as described in Figure 1. Most of the patients in current study did not have urine output data for each day of ICU stay, therefore we relied on serum creatinine (Scr) values to stratify AKI. Baseline Scr values were not available for 377/906 (35.5%) patients in our study for which baseline Scr was estimated with Modification of Diet in Renal Disease (MDRD) equation by assuming glomerular filtration rate as 75 ml/min/ 1.73m2 [3]. For patients with CKD, lowest Scr value during three months prior to ICU admission was served as baseline. Serum creatinine values were recorded for each day of hospitalization and worst AKI stage during ICU stay was served as final diagnostic stage for the study purpose. For example, if patients with AKIN-I on ICU admission progressed to AKIN-III or patients with AKIN-II recovered to AKIN-I then worst stages e.g. AKIN-III and AKIN-II were recorded as final stages of patients.
Statistical analysis
A statistical software package SPSS version 20 was used for the purpose of analysis in current study. Continuous data were presented as mean (standard deviation) while categorical variables were described as frequency and proportion. Student t-test and Chi-square test were used to compare groups. Logistic regression was performed to identify risk factors of AKI and mortality (dependent variables). Previously recognized risk factors and variables with significant statistical results were selected (stepwise) for logistic regression as independent covariates. Variables with p values <0.25 were subjected to multivariate analysis where variables with p values <0.05 were considered as independent determinants of dependent variable [19]. 95% confidence interval as calculated and p values <0.05 were deemed to indicate statistical significant.
Results
A total 906 (mean age: 53.6 ± 15.3, male: 58.2%) patients were evaluated in current study. The mean length of ICU stay was 14.4 ± 3.3 days. Out of the total patients, 801 (88.4%) were admitted to hospital due to some medical causes including 183 (20.2%) with cardiovascular diseases, 159 (17.6%) pulmonary diseases, 101 (11.1%) gastrointestinal diseases, 111 (12.2%) infectious diseases, 101 (11.2%) obstetrics and gynecological causes, 92 (10.1%) neurological and endocrinological disorders, 62 (6.8%) malignancies, 67 (7.4%) trauma, 16 (1.8%) accidental toxicities and 14 (1.6%) with other causes. Surgery was performed in 129 (14.2%) patients before ICU admission while 194 (21.4%) patients underwent surgery during their stay in ICU.
According to AKIN classification, AKI was observed in 487 (53.8%) patients with varying severity including AKIN-I in 89/487 (18.3%), AKIN-II in 137/487 (28.2%) and AKIN-III in 261/487 (53.5%) cases. Out of total patients with AKI, 111 (22.8%) patients progressed to more severe stage of AKI thus accounting considerable proportion of progressive AKI in our cohort. Out of total patients with AKI, dialysis was required by 75/487 (15.4%) patients. We compared clinical and laboratory characteristics of patients with and without AKI as described in Table 1. Patients with AKI were older than non-AKI and prevalence of co-morbidities including diabetes mellitus (DM) and hypertension was significantly higher among AKI patients. Similarly SOFA, APACHE-II and Glasgow Coma scores on ICU presentation were significantly higher among patients with AKI. Need of vasoactive drugs and aminoglycosides did not differ between patients with and without AKI even presence of sepsis on admission was significantly higher in AKI patients while on the other hand, need for invasive mechanical ventilation (IMV) was significantly higher among AKI patients. Patients with AKI had longer stay in ICU as compared to patients without AKI (p=0.002).
| Variables | All patients N=906 |
Patients without AKI N=419 |
Patients with AKI N=487 |
P value |
|---|---|---|---|---|
| Age (years) | 60.2 ± 9.4 | 57.3 ± 11.2 | 63.1 ± 7.3 | 0.014 |
| Male | 528 (58.3%) | 233 (55.6%) | 295 (60.6%) | 0.211 |
| Scr (µmol/L) | 137.6 ± 23.2 | 88.6 ± 16.8 | 186.6 ± 34.4 | <0.001 |
| BUN (mmol/L) | 18.2 ± 4.7 | 24.1 ± 6.3 | 11.9 ± 3.8 | <0.001 |
| Co-morbidities | ||||
| DM | 184 (20.3%) | 73 (17.4%) | 111 (22.8%) | 0.032 |
| HTN | 347 (38.3%) | 116 (27.7%) | 231 (47.4%) | 0.003 |
| IHD | 174 (19.2%) | 76 (18.1%) | 98 (20.1%) | 0.216 |
| SOFA score | 18 ± 4 | 17 ± 3 | 20 ± 5 | 0.032 |
| APACHE II score | 46 ± 3 | 40 ± 5 | 52 ± 4 | 0.001 |
| GCS | 10 ± 2 | 9 ± 3 | 13 ± 2 | 0.015 |
| MODs | 101 (11.1%) | 23 (5.5%) | 78 (16%) | 0.011 |
| Sepsis on admission | 276 (30.5%) | 98 (23.4%) | 178 (36.6%) | 0.042 |
| Vasoactive drugs on admission | 112 (12.4%) | 45 (10.7%) | 67 (13.8%) | 0.083 |
| Use of aminoglycosides | 95 (10.5%) | 39 (9.3%) | 56 (11.5%) | 0.379 |
| Need of IMV | 511 (56.4%) | 189 (45.1%) | 322 (66.1%) | <0.001 |
| Urine output <400 mL | 37 (4.1%) | 5 (1.2%) | 32 (6.6%) | 0.041 |
| Hypokalemia | 136 (15%) | 64 (15.3%) | 72 (14.8%) | 0.845 |
| Hyperkalemia | 114 (12.6%) | 9 (2.1%) | 105 (21.6%) | <0.001 |
| Acidosis on admission | 346 (38.2%) | 108 (25.8%) | 237 (48.7%) | 0.009 |
| ICU stay (days) | 10.4 ± 3.3 | 7.4 ± 4.6 | 13.2 ± 7.7 | 0.002 |
| Mortality | 267 (29.5%) | 32 (7.6%) | 235 (48.3%) | <0.001 |
| Continuous data was presented as mean ± standard deviation, categorical variables were presented as frequency and proportion, p value was calculated between patients with and without AKI. | ||||
Table 1. Baseline Characteristics of patients according to presence or absence of acute kidney injury (AKI).
Statistically tested and previously known determinants of AKI were assessed by using logistic regression where variables with p value <0.25 in univariate analysis were subjected for multivariate analysis. Old age diabetic patients with high SOFA and APACHE-II scores requiring IMV on admission were found to be significantly associated with AKI in our study (Table 2). Hypertension and sepsis were not found as risk factors of AKI in multivariate analysis while in unadjusted analysis both indicated association with AKI i.e. 2.2 (p=0.031) and 3.1 (p=0.042) respectively. In univariate analysis, GCS was associated with AKI (1.8, p=0.211) but such association was not observed in multivariate analysis (1.5, p=0.566). Acidosis had p value >0.25 (p=0.41) hence not included in multivariate analysis.
| Determinants | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Age >60 years | 2.8 | 1.5 to 9.6 | 0.001 |
| Diabetes Mellitus | 1.9 | 1.2 to 4.3 | 0.021 |
| High SOFA score | 2.7 | 1.6 to 5.7 | 0.042 |
| High APACHE-II score | 3.1 | 2.7 to 11.6 | 0.015 |
| Need of IMV | 4.2 | 2.1 to 8.3 | <0.001 |
| SOFA: Sepsis Related Organ Failure Assessment Score; APACHE-II: Acute Physiology And Chronic Health Evaluation; IMV: Invasive Mechanical Ventilation; OR: Odds Ratio; CI: Confidence Interval. Selection of variables for multivariate analysis was performed by forward selection method. | |||
Table 2. Determinants of AKI among patients attending intensive care unit by logistic regression.
Overall mortality in our study was 29.5% (267/906). The mortality rate was higher among patients with AKI (48.3%) as compared to non-AKI patients (7.6%). Out of the total patients with AKI (n=487), mortality was higher among AKIN-III (59.3%) as compared to AKIN-II (30.2%) and AKIN-I (10.5%). We found stepwise increase in mortality rate with increasing severity of AKI in our study where highest mortality rate was observed among severe AKI (AKIN-III) and lowest mortality rate was observed among mild AKI (AKIN-I). Pulmonary, neurological, cardiovascular and malignancies reasons to ICU admission were more common among patients with AKI than those without AKI while co-morbidities including DM, HTN and IHD were equally distributed among fatal and non-fatal cases (Table 3).
| Variables | All patients N=906 |
Fatal cases N=267 |
Non-fatal cases N=639 |
P value |
|---|---|---|---|---|
| Age (years) | 60.2 ± 9.4 | 61.8 ± 9.6 | 59.7 ± 8.8 | 0.046 |
| Male | 528 (58.3%) | 151 (56.6%) | 377 (59%) | 0.582 |
| Diagnosis on ICU admission | ||||
| Pulmonary | 190 (21%) | 78 (29.2%) | 112 (17.5%) | 0.021 |
| Neurological | 55 (6.7%) | 34 (12.7%) | 21 (3.3%) | 0.042 |
| Gastrointestinal | 141 (15.6%) | 43 (16.1%) | 98 (15.3%) | 0.896 |
| Cardiovascular | 127 (14%) | 51 (19.1%) | 76 (11.9%) | 0.043 |
| Malignancy | 116 (12.8%) | 67 (25.1%) | 49 (7.7%) | 0.004 |
| Infection | 62 (6.8%) | 23 (8.6%) | 39 (6.1%) | 0.082 |
| Trauma | 99 (10.9%) | 30 (11.2%) | 69 (10.8%) | 0.716 |
| Co-morbidities | ||||
| DM | 184 (20.3%) | 61 (22.8%) | 123 (19.2%) | 0.541 |
| HTN | 347 (38.3%) | 108 (40.4%) | 239 (37.4%) | 0.094 |
| IHD | 174 (19.2%) | 53 (19.9%) | 121 (18.9%) | 0.088 |
| AKI | 487 (53.8%) | 235 (88%) | 252 (39.4%) | <0.001 |
| AKIN-I | 89 (9.8%) | 31 (11.6%) | 58 (9.1%) | 0.351 |
| AKIN-II | 137 (15.1%) | 83 (31.1%) | 54 (8.5%) | 0.032 |
| AKIN-III | 261 (28.8%) | 121 (45.3%) | 140 (21.9%) | 0.001 |
| SOFA >9 | 490 (54.1%) | 201 (75.3%) | 289 (45.2%) | <0.001 |
| APACHE II score | 46 ± 3 | 57 ± 5 | 39 ± 2 | <0.001 |
| GCS | 10 ± 2 | 11 ± 2 | 9 ± 4 | 0.026 |
| Sepsis on admission | 276 (30.5%) | 109 (40.8%) | 167 (26.1%) | 0.028 |
| Vasoactive drugs on admission | 112 (12.4%) | 42 (15.7%) | 70 (11.8%) | 0.055 |
| Need of IMV | 511 (56.4%) | 198 (74.2%) | 313 (49%) | <0.001 |
| Need of dialysis | 75 (8.3%) | 65 (24.3%) | 10 (1.6%) | <0.001 |
| ICU stay (days) | 10.4 ± 3.3 | 14.7 ± 7.8 | 7.3 ± 2.3 | <0.001 |
| Continuous data was presented as mean ± standard deviation, categorical variables were presented as frequency and proportion, p value was calculated between patients with and without AKI. | ||||
Table 3. Comparison of baseline characteristics among fatal and nonfatal cases.
In order to evaluate possible determinants of mortality logistic regression was applied to statistically tested and previously known variables of mortality (Table 4). AKI, need of dialysis and mechanical ventilation were found strong determinant of mortality in our study. Among three stages of AKI, patients with AKIN-III had about 3 times more risk to die than patients with other stages. Neurological and pulmonary diagnoses were found to be associated with mortality in our study cohort. Furthermore, high scores on SOFA and APACHE-II scale were also found as risk factors of fatality among patients attending ICU. Old age (OR 1.3), cardiovascular (OR 1.9) and malignancy (OR 2.2) reasons of ICU admission, sepsis (OR 2.7) and AKIN-II (OR 3.8) were found to be significant predictors of mortality in unadjusted analysis but indicated insignificant p value in multivariate analysis (p>0.05). GCS and gastrointestinal causes of had p value >0.25 in univariate analysis hence these variables were not included in multivariate analysis.
| Determinants | Odds ratio | 95% CI | P value |
|---|---|---|---|
| Pulmonary causes | 1.7 | 1.1 to 3.5 | 0.031 |
| Neurological causes | 3.3 | 1.8 to 6.3 | 0.001 |
| AKI | 6.2 | 2.8 to 17.9 | <0.001 |
| AKIN-III | 3.2 | 1.4 to 12.8 | 0.002 |
| SOFA score >9 | 1.6 | 0.9 to 3.4 | 0.029 |
| High APACHE-II score | 2.3 | 1.4 to 5.8 | 0.035 |
| Need of IMV | 7.2 | 4.5 to 15.3 | <0.001 |
| Need of dialysis | 4.6 | 3.6 to 9.1 | <0.001 |
| SOFA: Sepsis Related Organ Failure Assessment Score; APACHE-II: Acute Physiology And Chronic Health Evaluation; IMV: Invasive Mechanical Ventilation; OR: Odds Ratio; CI: Confidence Interval. Selection of variables for multivariate analysis was performed by forward selection method. | |||
Table 4. Determinants of mortality among patients attending intensive care unit by Logistic regression.
Pulmonary and neurological causes of ICU admission, AKI, greater severity of illness and need for IMV and dialysis were found independent determinants of mortality in our study cohort attending ICU.
Discussion
The development of AKI presents a difficult challenge to the clinicians. Onset of AKI is often silent and patients may not notice AKI symptoms for days or weeks. Clinical and laboratory markers of its presence can be subtle and are often overlooked. Despite its often insidious presentation, AKI can be one of the most serious consequences that can occur, especially in hospitalized patients [3]. The highest incidence of AKI is in hospitalized patients in the ICU, even the incidence rate of ICU-acquired AKI (6%-25%) is much higher than hospital-acquired or community acquired AKI. Alarmingly, ICU-acquired AKI is associated with poor outcomes and survival rate (10-30%). Identification of high risk patients for AKI and mortality in ICU and managing such patients on priority basis will be useful to combat the burden of this silent acute illness [1,9]. Current study was an attempt to assess determinants of AKI and mortality among patients attending intensive care unit. About one half of the participants (54%) had AKI in our study with varying severity. The incidence of AKI in ICU varies widely among studies and it might be contributed to unavailability of unifying definition of AKI, methodological differences and heterogeneous nature of studied population [4]. Incidence of AKI reported in our study is higher than reported a Korean study i.e. 41.3% [13]. It might be due to use of different diagnostic criteria used to identify AKI. Park et al. used RIFLE (risk, injury, failure, loss of function, end stage renal disease) criterion to define AKI that requires 50% increased levels of serum creatinine from baseline while AKIN criteria used in current study can identify AKI even with small changes in Scr levels (0.3 mg/dl within 48 hours). Several studies have also been proposed that AKIN criterion is more sensitive than RIFLE criterion [3,20]. Besides these facts, comparison of prognosis and sensitivity of RIFLE and AKIN criteria have conflicting results as to which method is superior [20]. The incidence reported in recent investigation by Peres et al by using RIFLE criterion (53.2%) is comparable to incidence reported in our study by using AKIN criterion [11]. High incidence reported by Peres et al might be due to high proportion of the surgeries among patients (48%) while 36% patients in our study underwent surgery before ICU admission and during their stay in ICU. Mandelbaum et al. described the occurrence of AKI in 57% patients of total cohort by using AKIN criterion and these findings are consistent with incidence reported in our study [21]. These findings require further multicenter controlled studies in order to evaluate diagnostic and prognostic powers of these two criteria. It has been documented that AKI is predominant among males [6] but our study failed to demonstrate such prepordance. We found equal distribution (p=0.211) of males and females between two groups with and without AKI (Table 1). We also found that patients with AKI were older than patients without AKI (p=0.014) and patients with age greater than 60 years were found to have 2.8 times higher chances of having AKI than patients with age less than 60 years (Table 2). These findings are consistent with other reports describing that patients with AKI are 10 years older on an average than patients without AKI [11,13]. Overall, 8.3% study participants in our study required dialysis and most of them had AKI (Table 3). Peres et al reported the need of dialysis in 12.5% patients, comparatively higher than reported by our study [11]. It may be due to differences in patient`s demographics and cutpoints defined to initiate dialysis in both studies. Multivariate analysis revealed the presence of diabetes mellitus, high SOFA and APACHE-II scores and need of mechanical ventilation to be associated with AKI in ICU (Table 2). Sepsis and hypertension have been demonstrated to be associated with AKI [6,22] but our study failed to demonstrate them as independent predictors of AKI, though they were found risk factors of AKI in univariate analysis. These results suggest that old age diabetic patients with high SOFA and APACHE-II score requiring invasive mechanical ventilation should be managed on priority basis in order to avoid worse outcomes of AKI. A mild increase in serum creatinine has been found to be associated with mortality [23,24]. In the present study, the overall mortality rate was 29.5% that was significantly higher among AKI patients (48.3%) than non AKI (7.6%). Patients with AKIN-III had highest mortality rate in our study. Out of the 75 patients requiring dialysis, 65 (86.7%) patients died and dialysis need was found to be an independent predictor of mortality in our study (Table 4). Furthermore, AKI and its severe stage AKIN-III was also associated with mortality in our study (OR: 6.2 and 3.2 respectively). Other determinants of mortality in our study include pulmonary and neurological causes of ICU admission, high SOFA and APACHE-II scores and need of invasive mechanical ventilation. These findings are consistent with previous reports [11,13,25,26]. Interestingly, we found linear increase in mortality rate with AKIN staging from 9.8% to 28.8%. AKIN-II was also found as significant predictor of mortality in univariate analysis but failed to demonstrate any association in multivariate regression. Stepwise increase in mortality with increasing severity of AKI has also been reported in previous literature [3,25]. These findings demonstrate that even mild form of kidney dysfunction pose significant hospital mortality. Despite therapeutic and diagnostic advances, the incidence of AKI and mortality in ICU remained high in recent years. Early identification of high risk patients and managing them in priority manners may reduce incidence and progression of AKI as well as associated mortality.
Study Limitations
Our study has some major limitations needed to be addressed. Being a retrospective nature of study, reporting biasness and difficulty to assess AKI exist. Urine output data was missing for most of the patients therefore we relied on serum creatinine criteria to define AKI. Baseline serum creatinine values were not available for all patients and were estimated by using MDRD equation. It may cause over or under estimation of AKI cases due to the impact of confounders. Comparison of RIFLE and AKIN criteria was not performed in our study. Current study also lacks histopathological studies to elaborate causes of AKI i.e. pre-renal, renal or post renal. Patients with AKI were not followed up in our study in order to evaluate long term outcomes among AKI survivors. However, current study analyzed large number of patients and has strong statistical power by excluding patients with missing values. Standardized procedure of data collection in our institution ensures good reliability. Additionally, our study also evaluated patients by using sensitive AKIN criterion by including patients with increase in Scr as low as 0.3 mg/dL thus providing actual burden of AKI.
Conclusion
Our study showed that AKI was found among half of the patients attending ICU and significantly associated with in hospital mortality. Old age, diabetes mellitus, severe illness indicated by high SOFA and APACHE-II scores and need of mechanical ventilation were found significant determinants of AKI. On the other hand, pulmonary and neurological causes of ICU admission, AKI, high SOFA and APACHE-II scores and need of dialysis and mechanical ventilation were significantly associated with mortality in ICU. Early identification of high risk patients can be useful to reduce the burden of AKI and mortality in ICU.
References
- Wald R, Quinn RR, Luo J, Li P, Scales DC, Mamdani MM, Ray JG. University of Toronto Acute Kidney Injury Research Group. Chronic dialysis and death among survivors of acute kidney injury requiring dialysis. JAMA 2009; 302: 1179-1185.
- Lameire N, Van Biesen W, Vanholder R. The changing epidemiology of acute renal failure. Nat Clin Pract Nephrol 2006; 2: 364-377.
- Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Jummaat F. Incidence, Characteristics and Risk Factors of Acute Kidney Injury among Dengue Patients: A Retrospective Analysis. PloS one 2015; 10: e0138465.
- Mallhi TH, Khan AH, Sarriff A, Adnan AS, Khan YH, Jummaat F. Defining acute kidney injury in dengue viral infection by conventional and novel classification systems (AKIN and RIFLE): a comparative analysis. Postgraduate Med J 2016.
- Han SS, Kim S, Ahn SY, Lee J, Kim DK, Chin HJ, Chae DW, Na KY. Duration of acute kidney injury and mortality in critically ill patients: a retrospective observational study. BMC Nephrol 2013; 14: 133.
- Piccinni P, Cruz DN, Gramaticopolo S, Garzotto F, Dal Santo M, Aneloni G, Rocco M, Alessandri E, Giunta F, Michetti V, Iannuzzi M. Prospective multicenter study on epidemiology of acute kidney injury in the ICU: a critical care nephrology Italian collaborative effort (NEFROINT). Minerva Anestesiologica 2011; 77: 1072.
- Bellomo R, Ronco C, Kellum JA, Mehta RL, Palevsky P. Acute renal failure–definition, outcome measures, animal models, fluid therapy and information technology needs: the Second International Consensus Conference of the Acute Dialysis Quality Initiative (ADQI) Group. Critical Care 2004; 8: R204.
- Druml W, Metnitz B, Schaden E, Bauer P, Metnitz PG. Impact of body mass on incidence and prognosis of acute kidney injury requiring renal replacement therapy. Intensive Care Med 2010; 36: 1221-1228.
- Mehta RL, Kellum JA, Shah SV, Molitoris BA, Ronco C. Acute Kidney Injury Network: report of an initiative to improve outcomes in acute kidney injury. Crit Care 2007; 11: R31.
- Chawla LS, Amdur RL, Amodeo S, Kimmel PL, Palant CE. The severity of acute kidney injury predicts progression to chronic kidney disease. Kidney Int 2011; 79: 1361-1369.
- Peres LA, Wandeur V, Matsuo T. Predictors of acute kidney injury and mortality in an Intensive Care Unit. J Bras Nefrol 2015; 37: 38-46.
- Singbartl K, Kellum JA. AKI in the ICU: definition, epidemiology, risk stratification, and outcomes. Kidney Int 2012; 81: 819-825.
- Park WY, Hwang EA, Jang MH, Park SB, Kim HC. The risk factors and outcome of acute kidney injury in the intensive care units. Korean J Intern Med 2010; 25: 181-187.
- Ostermann M, Chang RW. Acute kidney injury in the intensive care unit according to RIFLE. Crit Care Med 2007; 35: 1837-1843.
- Wen Y, Jiang L, Xu Y, Qian CY, Li SS. Prevalence, risk factors, clinical course, and outcome of acute kidney injury in Chinese intensive care units: a prospective cohort study. Chin Med J (Engl) 2013; 126: 4409-4416.
- Fang Y, Ding X, Zhong Y, Zou J, Teng J. Acute kidney injury in a Chinese hospitalized population. Blood Purif 2010; 30: 120-126.
- Du B, An Y, Kang Y, Yu X, Zhao M, Ma X. China Critical Care Clinical Trial Group. Characteristics of Critically Ill Patients in ICUs in Mainland China. Critical Care Med 2013; 41: 84-92.
- Luo X, Jiang L, Du B, Wen Y, Wang M. A comparison of different diagnostic criteria of acute kidney injury in critically ill patients. Crit Care 2014; 18: R144.
- Mallhi TH, Khan AH, Adnan AS, Sarriff A, Khan YH, Jummaat F. Clinico-laboratory spectrum of dengue viral infection and risk factors associated with dengue hemorrhagic fever: a retrospective study. BMC Infect Dis 2015; 15: 1.
- Case J, Khan S, Khalid R, Khan A. Epidemiology of acute kidney injury in the intensive care unit. Crit Care Res Pract 2013; 2013: 479730.
- Mandelbaum T, Scott DJ, Lee J, Mark RG, Malhotra A. Outcome of critically ill patients with acute kidney injury using the Acute Kidney Injury Network criteria. Crit Care Med 2011; 39: 2659-2664.
- Wen Y, Jiang L, Xu Y, Qian CY, Li SS. Prevalence, risk factors, clinical course, and outcome of acute kidney injury in Chinese intensive care units: a prospective cohort study. Chin Med J (Engl) 2013; 126: 4409-4416.
- Lassnigg A, Schmidlin D, Mouhieddine M, Bachmann LM, Druml W, Bauer P, Hiesmayr M. Minimal changes of serum creatinine predict prognosis in patients after cardiothoracic surgery: a prospective cohort study. J Am Soc Nephrol 2004; 15: 1597-1605.
- Mallhi TH, Khan AH, Sarriff A, Adnan AS, Khan YH. Association of Ward Acquired, On-admission, Progressive and Non-progressive AKI with Death among Dengue Patients: A Hidden Relationship. Acta Med Port 2016; 29: 157-158.
- Hoste EA, Clermont G, Kersten A, Venkataraman R, Angus DC, De Bacquer D, Kellum JA. RIFLE criteria for acute kidney injury are associated with hospital mortality in critically ill patients: a cohort analysis. Critical Care 2006; 10: R73.
- Uchino S, Bellomo R, Goldsmith D, Bates S, Ronco C. An assessment of the RIFLE criteria for acute renal failure in hospitalized patients*. Critical Care Med 2006; 34: 1913-1917.