ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Paper - Biomedical Research (2019) Volume 30, Issue 6
Effect of proton pump inhibitors on glucose tolerance among Type 1 diabetes mellitus: A clinical narrative review
Department of Pharmacy Practice, College of Pharmacy Gulf Medical University, Ajman, UAE
- *Corresponding Author:
- Dr. Syed Wasif Gillani, PhD, GCP [cert]
Associate Professor Department of Pharmacy Practice College of Pharmacy, Gulf Medical University, Ajman, UAE Web: wasifgillani@gmail.com, dr.syedwasif@gmu.ac.ae
Accepted Date: December 20, 2019
Objective: This systemic review was aimed to evaluate the effectiveness of PPI in the treatment of DM
type 1 patients and other related risk factors.
Method: The review specifically focused on studies fulfilled the eligibility criteria; published in between
2016-2019 and should be written in the English language only. Primarily literature search focused on
original research article reported the objective data on PPIs use among T1DM patients. Articles were
searched in PubMed, Cochrane, Springer, and Science Direct. The search was limited to the English
language only.
Results: The results showed that the PPIs in combination with insulin achieved better clinical outcomes
than insulin users alone manifested by most of the gastrin and HbA1c results were achieved within the
targeted therapeutic range. The findings also showed that to have lower levels of HbA1c, anti-diabetic
medications should be used together with PPIs. Disregarding the way that exactly as expected, without
getting true significance beside the sulfonylureas gathering (in mix with or without metformin just as
thiazolidinedione) that got an abatement in HbA1c of 1.4% respect those patients who didn't consume a
PPI.
Conclusion: It is found that long-term use of PPI developed somehow protection against diabetes than
patients who were not treated with PPI. It is suggested to have RCTs focused on the use of PPI to predict
HbA1c and FBS levels in patient with type 1 diabetes.
Keywords
PPI, Glucose tolerance, Insulin resistance, T1DM, Diabetes, Endocrine.
Introduction
The number of pre diabetic and diabetic are increasing day by day. Studies conducted have shown the beneficial effects of proton pump inhibitors in patients with diabetes. The global prevalence of diabetes* among adults over 18 years of age has risen from 4.7% in 1980 to 8.5% in 2014 [1]. Diabetes Mellitus (DM) is a metabolic ailment which incorporates various physiological organs and on a very basic level portrayed by raised degrees of glucose [1]. The affliction presented in two structures, type1 DM and type 2 DM.
Type 1 diabetes is insulin-dependent diabetes commonly diagnosed among children and young adults. The exact cause for type 1 diabetes is still unknown however it is believed that genetic and environmental factors play vital role in disease development and progression. In contrast autoimmune response on β-cells of pancreas are responsible for development Type 2 DM. Type 2 diabetes is usually developed among middle aged and older adult population [2]. The objective of this clinical review is to explore the patterns of PPIs on glucose tolerance and affect the type 1 diabetes mellitus treatment. The review focused on the clinical impacts of PPIs in the management of diabetes mellitus.
Methodology
Eligibility criteria
Proton pump inhibitors: omeprazole is one the drug of choices of the PPIs therapy for patient’s ulcer. Drug specialist vs. Doctor: thinks about spotlight on either drug specialist oversaw centre as well as doctor oversaw facility to perceive how the two gatherings are accomplishing individual clinical results. Blood glucose measurements: Persistent glucose checking gives data about the course, size, term, recurrence, and reasons for variances in blood glucose levels. Contrasted and regular strengthened glucose observing, characterized as three to four blood glucose estimations for each day, persistent checking gives a lot more prominent understanding into glucose levels for the duration of the day. Nonstop glucose readings that supply pattern data can help distinguish and counteract undesirable times of hypo-and hyperglycaemia [3].
HbA1c: Haemoglobin A1c, often abbreviated HbA1c, is a type of haemoglobin (a blood shade that conveys oxygen) that is bound to glucose. The blood test for HbA1c level is routinely performed in individuals with type 1 and type 2 diabetes mellitus. Blood HbA1c levels are intelligent of how well diabetes is controlled. The ordinary range for level for haemoglobin A1c is under 6%. HbA1c is ordinarily estimated to decide how well a sort 1 or type 2 diabetes treatment plans (meds, exercise, or dietary changes) is working [4].
Search subjects
This study searched the literature based on required criteria as; the usage of PPI among diabetic patients, the effect of them PPIs on blood glucose level with Type 1 diabetic patients and various risk factors associated with it. Complications related to diet and drug interactions in diabetic patients and its effects on hyper or hypo glycaemia. Treatment options and related consequences are specific to patients with type 1 diabetes mellitus.
Search eligibility criteria
This systemic review specifically focused on studies fulfilled the eligibility criteria; published in between 2016-2019 and should be written in the English language only. A systematic review and meta-analyses on effect of PPI among diabetic patients but we limited our article search to specific type of diabetes which is type 1 diabetes mellitus. Primarily literature search focused on original research article reported the objective data on PPIs use among T1DM patients.
Literature search
Articles were searched in PubMed, Cochrane, Springer, and Science Direct. The search was limited to the English language from 2016 onwards. Due to the inclusion criteria of the article ’ s keywords such as Esomeprazole, management, pharmacist, Type 1, therapy, clinic, and anti-diabetics were used. For example, the PubMed research method was written as follows: (PPI management), (anti-diabetic management).
Study selection and data extraction
Qualified examinations were additionally audited for its quality (study plan, length of study, mediation done, how they evaluated the outcomes and follow-up methodology). Quiet portrayal was likewise assessed regarding difficulties and sign of protons pump inhibitors.
Results
Literature search
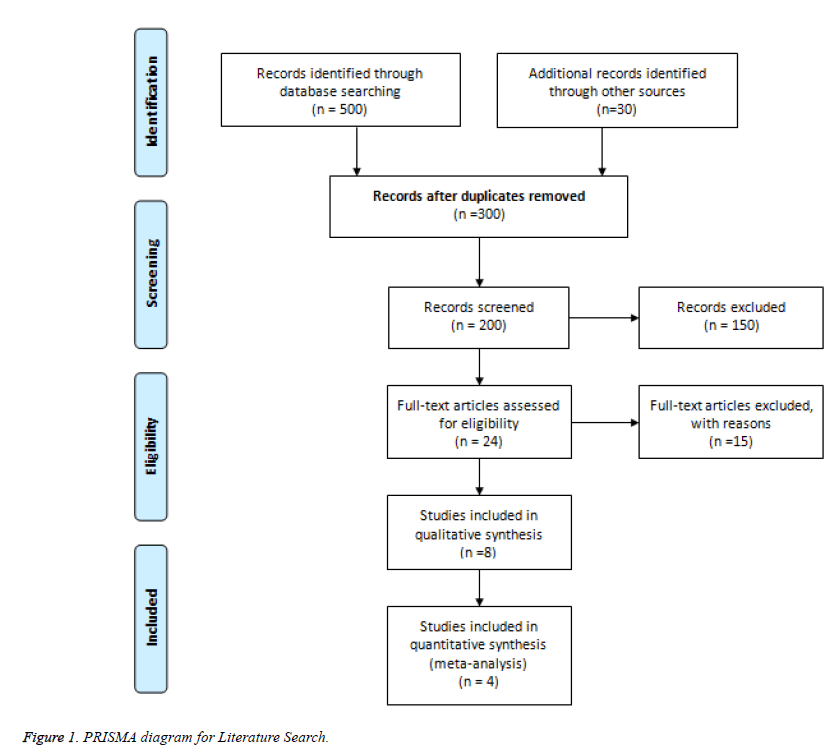
A total of 500 articles were found to be relative to the subject, after excluding the duplicates >50% have been excluded. Following the title and reviewing the abstract another 300 were ruled out, and 6 studies were included in the systematic review (Figure 1).
Drug interaction between anti-diabetic medication and PPI: This literature (A Study on Drug-Drug Interaction of Esomeprazole and Anti-Diabetic Drugs) is proving that in DM type 1 has no drug interaction between anti-diabetic medications and PPIs. Starting with first literature, Esomeprazole at 30 mg/kg portion didn't without anyone else's input decrease the blood glucose level, demonstrating that any communication with anti-diabetic sedates in this examination isn't of the pharmacodynamic type. In the present examination, restorative dosages of esomeprazole didn't impact any of the parameters of the hypoglycemia incited by sulfonylureas. In that case, esomeprazole upgraded the term of hypoglycemia just as the top degree of hypoglycemia incited by sulfonylureas. The writing reports uncover that sulfonylureas are utilized predominantly by CYP2C9 and CYP3A [5]. At the portion of 30 mg/kg esomeprazole most likely restrains these isoenzymes. Since it requires multiple times the helpful portions of esomeprazole to restrain the CYP isoenzymes that are liable for digestion of sulfonylureas, these compounds obviously have low affectability/partiality for esomeprazole.
Also, according to the following literature (Combination therapy with sitagliptin and lansoprazole in patients with recent-onset type 1 diabetes), results show that combination therapy with sitagliptin and lansoprazole was well-tolerated. No adverse or serious adverse events were probably or related to the study treatment. 87 events were identified as possibly related to treatment but were distributed equally between treatment and placebo groups. The frequencies of various adverse events and the frequencies of hypo-glycemic events did not differ significantly between the two groups [6]. In this issue of The Lancet Diabetes and Endocrinology, Kurt Griffin and associates reported the eventual outcomes of the Fix T1D starter, a phase 2, randomized, twofold outwardly impeded fundamental that tried to switch or adjust as of late dissected sort 1 diabetes in kids and adults through treatment with the blend of a DPP-4 inhibitor (sitagliptin) and a PPI (lansoprazole). Along these lines, it remains possible that a couple of drugs that change hormone obsessions may extend the adaptability and expansion of β cells and might have work in alteration or decrease of type 1 diabetes. Despite the way that DPP-4 inhibitors and GLP1-receptor agonists could be viewed as β-cell guarded, they furthermore increase the pace of insulin release. Of interest, this defense might be contrary to the possibility that those with as of late examined sort 1 diabetes have hurt β cells and would benefit by assumed β-cell rest by methods for concentrated glycemic control; regardless, there is advancing talk and conflicting data as for thought [6].
Long term use of PPI with type 1 diabetes: In the following literature (Effect of Proton-Pump Inhibitor Therapy on Serum Chromogranin A Level) it is explaining the effects of longterm use for PPI with DM typ1 patients. According to Sanduleanu et al, we additionally assessed the impact of discontinuance of PPI treatment, the time pattern of progress of serum CgA and gastrin levels. No distinctions were seen between the various PPI particles from this viewpoint. The most unmistakable increment was seen in patients treated with a high-portion PPI routine. Long term proton pump inhibitor utilize that have generated the most noteworthy concern: B12 insufficiency; iron lack; hypomagnesemia; expanded helplessness to pneumonia, enteric diseases, and breaks; hypergastrinemia and cancer; interactions between drugs; and birth defects. Diarrhea The most relevant reported adverse effect due to PPI use whether on long term or discontinuation. Most studies didn ’ t specifically determine the cause of diarrhea but given that it is acute diarrhea most probably the cause is infectious. Thus, proving this issue has not been reported fully and further investigations and studies are needed physicians have been overly prescribing PPIs [7].
Lifestyle modification in type 1 to avoid GI problems: This literature (The use of proton pump inhibitors decreases the risk of diabetes mellitus in patients with upper gastrointestinal disease) is the first retrospective cohort study evaluating the effect of PPIs on DM risk in patients with UGID. We found that patients with UGID had an increased risk of DM compared to non-UGID patients, but we also found that UGID patients who received PPI therapy had a significantly lower risk of developing DM within 5 years than patients who did not receive PPIs. Furthermore, we observed a dose-related effect of PPIs on DM risk [8].
Diabetes and gastrin secretion: As discussed in the review (Proton pump inhibitors: impact on glucose metabolism) Gastrin has shown to be an islet development factor (like glucagon-like peptide-1, epidermal development factor, changing development factor-a,) and have the option to reestablish a practical b-cell mass in diabetic creatures. This hormone is probably going to animate insulin emission during a conventional protein-rich feast; this is, to have an incretinlike impact. Proton siphon inhibitors (PPIs) can raise serum gastrin focus significantly and in this way, influence on glucose digestion through advancing b-cell recovery/extension and furthermore upgrading insulin emission. Quickened lipolysis, incretin deficiency/obstruction, hyperglucagonemia, renal expanded glucose reabsorption, and cerebrum insulin opposition. Toward the end, hyperglycaemia in both sort 1 diabetes (T1D) and T2D results from a flat out or relative deficit in the pancreatic b cell mass; in this manner, b-cell recovery is a zone under dynamic examination. Selections of treatments generally made by efficacy, security, decency, and cost of prescriptions, straightforwardness, and foreseen level of patient adherence [9].
According to Suarez-Pinzon et al the study showed that blend treatment with GLP-1 and gastrin grows the b-cell mass in human islets embedded in immune deficient diabetic mice, to a great extent from pancreatic conduit cells related with the islets, and this was sufficient to enhance hyperglycaemia in the mice. Our study shows that sitagliptin and lansoprazole treatment in new-onset type 1 diabetes produces a heterogeneous response in concentrations of GLP-1 and gastrin. Although the primary endpoint was not met, our findings suggest increased concentrations of GLP-1 and gastrin in participants could have a protective effect on C-peptide preservation. Additional studies of these drugs in combination with other drugs are necessary to assess their potential use for new-onset type 1 diabetes and to understand the heterogeneity of the responses. Also, Suarez-Pinzon et al showed that blend treatment with a DPP-4 inhibitor to raise endogenous degrees of GLP-1, together with a PPI could turn around diabetes in the NOD mouse model of T1D. Treatment with DPP-4 inhibitor re-established normoglycemia in 38% of mice, PPI in 33%, and blend of DPP-4 inhibitor and PPI in 75% of creatures. Medicines with a solitary operator didn't significantly build plasma C-peptide or pancreatic insulin content, while joined treatment significantly did [10].
The outcome was a pattern to have lower methods for HbA1c for the diverse anti diabetic treatments joined with a PPI, in spite of the fact that true to form, without getting factual significance aside from the sulfonylureas gathering (in blend with or without metformin as well as thiazolidinedione) that got a decrease in HbA1c of 1.4% regard those patients who didn't expend a PPI. After this, Boj-Carceller et al. individual correspondence in a littler report with diabetic in-patients with poor glycemic control (normal HbA1c of 9.2%), where 33.8% had T1D, found that the individuals who were utilizing a PPI indicated lower HbA1c levels, uniquely on the off chance that they were T2D not accepting insulin treatment yet [11].
PPI and gastric emptying rate: An issue on Effects of Proton Pump Inhibitors on Gastric Emptying has concluded that a delay in gastric emptying rate was caused by PPI in DM type 1 patient. The delay in not significant and seems small but physicians should take precautions in patients whose baseline gastric emptying rate is slow. If a diabetic patient is on insulin therapy and it being co administered with PPI, they might experience attacks of hypoglycaemia because of delay in emptying rate could produce a time gap between the release of nutrients in the small intestine and the action of insulin [12].
Discussion
This systemic review aimed to evaluate the effectiveness of PPI in the treatment of DM type 1 patients and other related risk factors. The results showed that the PPIs in combination with insulin achieved better clinical outcomes than insulin users alone manifested by most of the gastrin and HbA1c results were achieved within the targeted therapeutic range thus prevails the primary objective of the study. Similar findings were reported in several publications, Suarez-Pinzon et al. reported that blending treatment with a DPP-4 inhibitor to raise endogenous degrees of GLP-1, together with a PPI could turn around diabetes in the NOD mouse model of T1D. Treatment with DPP-4 inhibitor re-established normoglycemia in 38% of mice, PPI in 33%, and blend of DPP-4 inhibitor and PPI in 75% of creatures. Medicines with a solitary operator didn't significantly build plasma C-peptide or pancreatic insulin content, while combined treatment significantly did. However, when combing GLP-1 and gastrin grows the b-cell mass in human islets embedded in immune deficient diabetic mice, to a great extent from pancreatic conduit cells related with the islets, and this was sufficient to enhance hyperglycaemia in the mice [10].
The result was an example to have lower techniques for HbA1c for the assorted anti-diabetic medications got together with a PPI, disregarding the way that exactly as expected, without getting true significance beside the sulfonylureas gathering (in mix with or without metformin just as thiazolidinedione) that got an abatement in HbA1c of 1.4% respect those patients who didn't consume a PPI. After this, Boj-Carceller et al. singular correspondence in a tinier report with diabetic in-patients with poor glycemic control (ordinary HbA1c of 9.2%), where 33.8% had T1D, found that the people who were using a PPI demonstrated lower HbA1c levels, interestingly in case they were T2D not tolerating insulin treatment yet [11].
According to PubMed, the following article (first review companion study assessing the impact of PPIs on DM chance in patients with UGID. We found that patients with UGID had an expanded danger of DM contrasted with non-UGID patients, yet we additionally found that UGID patients who got PPI treatment had a fundamentally lower danger of creating DM inside 5 years than patients who didn't get PPIs. Moreover, we watched a portion related impact of PPIs on DM hazard [8]. An issue on Effects of Proton Pump Inhibitors on Gastric Emptying has presumed that a postponement in gastric discharging rate was brought about by PPI in DM type 1 patient. The deferral in not critical and appears to be little but rather doctors should play it safe in patients whose standard gastric purging rate is moderate. On the off chance that a diabetic patient is on insulin treatment and it being codirected with PPI, they may encounter assaults of hypoglycaemia due to defer in discharging rate could deliver a period hole between the arrival of supplements in the small digestive tract and the activity of insulin [13-19].
Limitations of the Review
Most of the articles included animals subject so not enough information we found on human subjects. Not only this, but also most of the information found was on type 2 DM patients and their correlation with PPI. Not all studies had achieved the accuracy of collecting the data. The small group size might lead to a false statistical significance and the short term of follow-up. Several studies had no data to compare their blood sugar level or the HbA1c. Also, some of the data were old so were not really taken into consideration.
Conclusion
This study was conducted to evaluate the ability of the Proton Pump inhibitors effect with type 1 patient diabetes mellitus yet was found didn’t only meet the standard but also suggested that it can also be used as an anti-diabetic medication enhancer with insulin. It is also found that long-term use of PPI developed somehow protection against diabetes than patients who were not treated with PPI. It is suggested to have RCTs focused on the use of PPI to predict HbA1c and FBS levels in patient with type 1 diabetes. Further investigations are need on human subjects since most of the results were obtained from the mice population.
References
- Draper J, Mur LA, Jenkins G, Ghosh-Biswas GC, Bablak P, Hasterok R, Routledge AP. Brachypodium distachyon. A new model system for functional genomics in grasses. Plant Physiol 2001; 127: 1539-1555.
- Christiansen P, Andersen CH, Didion T, Folling M, Nielsen KK. A rapid and efficient transformation protocol for the grass Brachypodium distachyon. Plant Cell Rep 2005; 23: 751-758.
- Vogel JP, Garvin DF, Leong OM, Hayden DM. Agrobacterium-mediated transformation and inbred line development in the model grass Brachypodium distachyon. Plant Cell Tissue Organ Cult 2006; 84: 199-211.
- Vogel J, Hill T. High-efficiency Agrobacterium-mediated transformation of Brachypodium distachyon inbred line Bd21-3. Plant Cell Rep 2008; 27: 471-478.
- Alves SC, Worland B, Thole V, Snape JW, Bevan MW, Vain P. A protocol for Agrobacterium-mediated transformation of Brachypodium distachyon community standard line Bd21. Nature Protoc 2009; 4: 638.
- Ajmal MM, Almatrooshi S, Hussain M. Sort by relevance Sort by date Role of public policies in promoting CSR: empirical evidence from business and civil society of UAE, 2019.
- Hoekema A, Hirsch PR, Hooykaas PJ, Schilperoort RA. A binary plant vector strategy based on separation of vir-and T-region of the Agrobacterium tumefaciens Ti-plasmid. Nature 1983; 303: 179-180.
- Lazo GR, Stein PA, Ludwig RA. A DNA transformation–competent Arabidopsis genomic library in Agrobacterium. Biotechnol 1991; 9: 963.
- Chen S, Songkumarn P, Liu J, Wang GL. A versatile zero background T-vector system for gene cloning and functional genomics. Plant physiol 2009; 150: 1111-1121.
- Cutler SR, Ehrhardt DW, Griffitts JS, Somerville CR. Random GFP∷ cDNA fusions enable visualization of subcellular structures in cells of Arabidopsis at a high frequency. Proceedings of the Nat Acad Sci 2000; 97: 3718-3723.
- Linsmaier EM, Skoog F. Organic growth factor requirements of tobacco tissue cultures. Physiologia Plantarum 1965; 18: 100-27.
- Ohira K, Ojima K, Fujiwara A. Studies on the nutrition of rice cell culture I. A simple, defined medium for rapid growth in suspension culture. Plant Cell Physiol 1973; 14: 1113-1121.
- Murashige T, Skoog F. A revised medium for rapid growth and bioassay with tobacco tissue cultures. Physiol Plant 1962; 15: 473-497.
- Doyle JJ, Doyle JL. A rapid DNA isolation procedure for small quantities of fresh leaf tissue. Phytochem Bulletin 1987; 19: 11–15.
- Gombos M, Zombori Z, Szécsényi M, Sándor G, Kovács H, Györgyey J. Characterization of the LBD gene family in Brachypodium: a phylogenetic and transcriptional study. Plant Cell Rep 2017; 36: 61-79.
- Zhu H, Wen F, Li P, Liu X, Cao J, Jiang M, Ming F, Chu Z. Validation of a reference gene (BdFIM) for quantifying transgene copy numbers in Brachypodium distachyon by real-time PCR. Appl Biochem Biotechnol 2014; 172: 3163-3175.
- Svec D, Tichopad A, Novosadova V, Pfaffl MW, Kubista M. How good is a PCR efficiency estimate: Recommendations for precise and robust qPCR efficiency assessments. Biomol Detect Quantif 2015; 3: 9-16.
- Lee MB, Jeon WB, Kim DY, Bold O, Hong MJ, Lee YJ, Park JH, Seo YW. Agrobacterium-mediated transformation of Brachypodium distachyon inbred line Bd21 with two binary vectors containing hygromycin resistance and GUS reporter genes. J Crop Sci Biotechnol 2011; 14: 233-238.
- Chetty VJ, Ceballos N, Garcia D, Narváez-Vásquez J, Lopez W, Orozco-Cárdenas ML. Evaluation of four Agrobacterium tumefaciens strains for the genetic transformation of tomato (Solanum lycopersicum L.) cultivar Micro-Tom. Plant Cell Rep 2013; 32: 239-247.
- Nagy B, Majer P, Mihaly R, Pauk J, Horváth GV. Stress tolerance of transgenic barley accumulating the alfalfa aldose reductase in the cytoplasm and the chloroplast. Phytochem 2016; 129: 14-23.
- Păcurar DI, Thordal-Christensen H, Nielsen KK, Lenk I. A high-throughput Agrobacterium-mediated transformation system for the grass model species Brachypodium distachyon L. Transgenic Res 2008; 17: 965-975.
- Winicur ZM, Zhang GF, Staehelin LA. Auxin deprivation induces synchronous Golgi differentiation in suspension-cultured tobacco BY-2 cells. Plant Physiol 1998; 117: 501-513.
- Gaspar TH, Kevers C, Faivre-Rampant O, Crèvecoeur M, Penel CL, Greppin H, Dommes J. Changing concepts in plant hormone action. In Vitro Cell Dev Biol Plant 2003; 39: 85.
- Perrot-Rechenmann C, Napier RM. Auxins. In: Vitamins and Hormones. 2005; pp203-233.
- Zhou D, Yin K, Xu Z, Xue H. Effect of polar auxin transport on rice root development. Acta Botanica Sinica 2003; 45: 1421-1427.
- Wang J, Seliskar DM, Gallagher JL. Tissue culture and plant regeneration of the salt marsh monocots Juncus roemerianus and Juncus gerardi. In Vitro Cell Dev Biol Plant 2005; 41: 274-80.
- Khan TN, Jeelani G, Tariq S, Mahmood T, Hussain SI. Effect of different concentrations of rooting hormones on growth of tomato cuttings (Solanum esculentus L). J Agric Res 2011; 49: 241-247.
- MacIsaac SA, Sawhney VK, Pohorecky Y. Regulation of lateral root formation in lettuce (Lactuca sativa) seedling roots: Interacting effects of α‐naphthaleneacetic acid and kinetin. Physiologia Plantarum 1989; 77: 287-293.
- Jeon JS, Lee S, Jung KH, Jun SH, Jeong DH, Lee J, Kim C, Jang S, Lee S, Yang K, Nam J. T‐DNA insertional mutagenesis for functional genomics in rice. Plant J 2000; 22: 561-570.
- Bevan MW, Garvin DF, Vogel JP. Brachypodium distachyon genomics for sustainable food and fuel production. Curr Opin Biotechnol 2010; 21: 211-217.
- Meyerowitz EM, Pruitt RE. Arabidopsis thaliana and plant molecular genetics. Science 1985; 229: 1214-1218.
- Vain P, Worland B, Thole V, McKenzie N, Alves SC, Opanowicz M, Fish LJ, Bevan MW, Snape JW. Agrobacterium‐mediated transformation of the temperate grass Brachypodium distachyon (genotype Bd21) for T‐DNA insertional mutagenesis. Plant Biotechnol J 2008; 6: 236-245.