ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 15
Diffuse large B cell lymphoma-related prognostic factors, Ki-67 and Bcl-6 expression levels
Department of Oncology, Hubei Cancer Hospital, Wuhan, Hubei, PR China
Accepted date: July 03, 2017
Objective: This study aims to investigate the diffuse large B cell lymphoma-related prognostic factors, Bcl-6 and Ki-67 expression levels.
Methods: 67 cases of patients with diffuse large B cell lymphoma in our hospital were collected from Feb 2014 to Mar 2015. The Bcl-6 and Ki-67 expression levels in patients with diffuse large B cell lymphoma were detected using the immunohistochemical method. The related characteristics and prognosis were analyzed.
Results: Statistical analysis shows that the Bcl-6 protein expression levels are not related to sex or age; Ki-67 is not related to sex but related to age. Bcl-6 is not related to lactate dehydrogenase or primary site but is related to Ann Arbor stage. Ki-67 is related to lactate dehydrogenase and Ann Arbor stage.
Conclusion: The microvessel density dose, Bcl-6-positive rate and Ki-67 labelling index of diffuse large B cell lymphoma are important indexes to evaluate the prognosis of patients with diffuse large B cell lymphoma.
Keywords
Diffuse large B cell lymphoma (DLBCL), Prognosis, Bcl-6, Ki-67.
Introduction
Diffuse Large B Cell Lymphoma (DLBCL), a heterogeneous non-Hodgkin’s lymphoma, is a malignant tumor characterized by B cell diffuse proliferation and has the characteristics of rapid growth and invasiveness [1]. A large number of studies have indicated that angiogenesis is the key factor of the tumor growth and metastasis and is a new index to judge the prognosis of tumor [2]. In recent years, the relationship between Bcl-6 and Ki-67 expression levels, as well as the prognosis of BLBCL, has been a concern by many scholars [3]. In this study, 67 cases of patients with DLBCL in our hospital were collected from Feb 2014 to Mar 2015. For these cases, follow up was conducted. The related prognostic factors, Ki-67 and Bcl-6 expression levels, were investigated. The report is as follows.
Data and Methods
General data
67 cases of patients with DLBCL in our hospital were obtained from Feb 2014 to Mar 2015. These cases included 38 male and 29 female patient’s aged 17-68 y old (average age of 44.62 ± 6.25). Among the 67 cases of patients, 54 cases had tumors inside the primary lymph nodes and 13 cases had the tumors outside the lymph nodes. The clinical manifestations of the primary tumor in the lymph nodes mainly included weight loss and fever, whereas manifestations of those outside the lymph nodes were abdominal pain and gastrointestinal bleeding. Ten lymph nodes with reactive hyperplasia were selected as the control.
Immunohistochemistry staining
The specimen was fixed using 10% neutral formalin liquid and the sections were embedded using paraffin. The monoclonal antibody working fluid Ki-67 and Bcl-6 in the experiment were produced by Fuzhou Maixin biological technical developing company. The SP method was adopted for the immunohistochemical staining method. The sections were digested using the trypsin before the primary antibody was added for 20 min. PBS was taken as the negative control instead of primary antibody.
Detection of Bcl-6 and Ki-67 positive rates
The Ki-67 labelling index, Bcl-6-positive rate, and Microvessel Density (MVD) count were obtained using the color magic image analysis system. To ensure the accuracy and objectivity of MVD count in the tumor, the representative sections were selected. Then, the marginal reaction zone and tumor bleeding area were excluded. The sections were observed under lowpower field to determine the top three areas with the highest vascular density in each section. The MVD numerical value in each region was counted under low-power field. The average value was the tumor MVD value [4].
Statistical processing
The data were processed using the SPSS16.0 software. The enumeration data were compared using χ2 test. P<0.05 indicated that the data was statistically significant.
Results
Clinical and pathological results
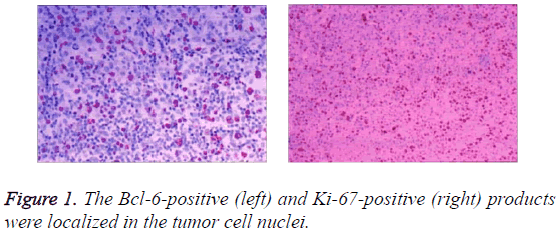
The Bcl-6 and Ki-67 positive products were localized in the nuclei, which are brownish red and fine granular (Figure 1).
The relationship between Bcl-6 and Ki-67 protein expression levels and general data
In Table 1, statistical analysis shows that Bcl-6 and protein expression levels are not related to sex or age. Ki-67 expression is not related to sex, but it is related to age.
| Group | n | Bcl-6-positive rate | Ki-67 high expression rate | |
|---|---|---|---|---|
| Sex | Male | 38 | 24 (63.16%) | 25 (65.79%) |
| Female | 29 | 20 (68.97%) | 20 (68.97%) | |
| Age | <60 | 48 | 26 (54.17%) | 25 (52.08%) |
| ≥ 60 | 19 | 14 (73.68%) | 18 (94.74%) | |
| χ2 value | - | - | - | 7.265 |
| P value | - | - | - | <0.05 |
Table 1: The relationship between Bcl-6 and Ki-67 protein expression levels and general data.
The relationship between Bcl-6 and Ki-67 protein expression levels and clinical characteristics
In Table 2, statistical analysis shows that Bcl-6 is not related to lactate dehydrogenase or primary site but related to Ann Arbor stage. Ki-67 is related to lactate dehydrogenase and Ann Arbor stage.
| Group | n | Bcl-6-positive rate | Ki-67 high expression rate | |
|---|---|---|---|---|
| Ann Arbor stage | I, II stage | 40 | 33 (82.50%) | 22 (55.00%) |
| III, IV stage | 27 | 13 (48.15%) | 23 (85.19%) | |
| Lactic dehydrogenase | Normal | 37 | 27 (72.97%) | 19 (51.35%) |
| Normal | 30 | 17 (56.67%) | 26 (86.67%) | |
| Primary site | Inside the lymph node | 43 | 31 (72.09%) | 29 (67.44%) |
| Outside the lymph node | 24 | 13 (54.17%) | 17 (70.83%) | |
| χ2 value | - | - | - | 19.723 |
| P value | - | - | - | <0.05 |
Table 2: The relationship between Bcl-6 and Ki-67 protein expression levels and clinical characteristics.
Discussion
DLBCL is one of the most common Non-Hodgkin lymphomas, accounting for 30%-40% of Hodgkin lymphomas [5]. Clinical manifestations of DLBCL are heterogeneous. The symptoms can be alleviated in 40%-50% of patients after combined chemotherapy. However, other patients are still not relieved or have relapse. Genetic difference of tumor cells is the main reason for this difference [6].
Bcl-6 gene is the recognized DLBCL-associated oncogene and independent prognostic factor. Different opinions exist about the relationship between Bcl-6 expression and lymphoma prognosis. Many studies have indicated that Bcl-6 has a close relationship with the prognosis of the lymphoma [7].
Moreover, studies considered that Bcl-6 had little relationship with its prognosis. Ki-67 was expressed in the cell cycle stages of G, S, G2 and M. The ratio of Ki-67-positive cells reflected the proliferated cell ratio entering the cell cycle. Its high expression was usually associated with the adverse reactions of tumor prognosis [8]. The clinical analysis of DLBCL shows that Bcl-6 protein expression is not related to sex or age and Ki-67 is not related to sex but is related to age. This result is the same with previously obtained results [9]. Protein expression levels of tumor cells differed, thereby resulting in differences in biological behaviour of tumor cells. The abnormal expression levels of Ki-67 and ki-67 proteins would affect the cell apoptosis and growth of Bcl-6 [10]. Statistical analysis shows that Bcl-6 is not related to lactate dehydrogenase or primary site but is related to Ann Arbor stage. Ki-67 is related to lactate dehydrogenase and Ann Arbor stage.
Conclusion
The MVD dose, Bcl-6-positive rate, and Ki-67 labelling index of DLBCL are important indicators to evaluate the prognosis of patients with diffuse large B cell lymphoma.
References
- Ozturk N, Kara A, Vural I. Evaluation of antitumor activity of a non-steroidal anti-inflammatory drug, ibuprofen, by a targeted nanoparticulate system. Lat Am J Pharm 2017; 36: 44-52.
- Li J, Sun D, Wang R. The in vitro immunomodulatory and anti-tumor activity of thymosin α1-thymopentin fusion peptide. Lat Am J Pharm 2016; 35: 1559-1566.
- Nisar N, Rabbani M, Masood AI. A prospective study of pharmaceutical care for lymphoma patients in the department of oncology, Nishtar Hospital, Multan, Pakistan. Lat Am J Pharm 2013; 32: 322-328.
- Raj JR, Rahman SMK, Anand S. Preliminary evaluation of differentiation of benign and malignant breast tumors using non-invasive diagnostic modalities. Biomed Res India 2016; 27: 596-603
- Sailesh KS, Archana R, Sajeevan A, Mukkadan JK. Effect of controlled vestibular stimulation on depression, spatial and verbal memory scores in underweight female students-A pilot study. Biomed Res India 2016; 27: 611-615
- Kang C, Sun Y, Zhu J, Li W, Zhang A, Kuang T, Xie J, Yang Z. Delivery of nanoparticles for treatment of brain tumor. Curr Drug Metab 2016; 17: 745-754.
- Kim SH, Kaplan JA, Sun Y, Shieh A, Sun HL, Croce CM, Grinstaff MW, Parquette JR. The self‐assembly of anticancer camptothecin-dipeptide nanotubes: a minimalistic and high drug loading approach to increased efficacy. Chem Eur J 2015; 21: 101-105.
- Kim SH, Sun Y, Kaplan JA, Grinstaff MW, Parquette JR. Photo-crosslinking of a self-assembled coumarin-dipeptide hydrogel. New J Chem 2015; 39: 3225-3228.
- Song L, Kang C, Sun Y, Huang W, Liu W, Qian Z. Crocetin inhibits lipopolysaccharide-induced inflammatory response in human umbilical vein endothelial cells. Cell Physiol Biochem 2016; 40: 443-452.
- Sun Y, Kang C, Liu F, Song L. Delivery of antipsychotics with nanoparticles. Drug Develop Res 2016; 77: 393-399.