ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 4
Cost analysis of different venues for treating suicide cases presented to the Emergency Department.
1Cumhuriyet University, Department of Emergency Medicine, Sivas, Turkey
2Bezmialem Vakif University, Department of Emergency Medicine, Istanbul, Turkey
3Isparta State Hospital, Department of Emergency Medicine, Isparta, Turkey
4Suleyman Demirel University, Department of Anesthesia and Reanimation, Isparta, Turkey
- *Corresponding Author:
- Kenan Ahmet TURKDOGAN
Bezmialem Vakif University
Department of Emergency Medicine
Istanbul, Turkey
Accepted May 11 2014
Patients presented with poisoning-related suicide attempts is one of the most problematic cases of the emergency services. The most important reason for this being the failure to decide the department of the hospital in which these patients should be admitted to, following consultation. The objective of this study is to emphasize the cost- lowering effect of treatment and follow-up of such suicide cases in Emergency Departments (ED) instead of intensive care units. A total of 791 adult patients with suicidal attempts were retrospectively examined and their clinical and demographic data were included. In addition, the costs of their treatment in the ED, Intensive Care Unit (ICU) and Psychiatric Clinic between 01/01/2007 and 31/12/2011were compared. When patients were classified by their month of birth it was found that patients who born in January had the maximum tendency to commit suicide (n:227, 28.7%), while those born in December were the least to do so (n:30, 3.8%). Of all the patients, 122 (15.4%) were followed-up in Anesthesia Intensive Care (AIC), 639 (80.8%) in the Emergency Department Observation Unit and 30 (3.8%) in the Psychiatric Clinic.When costs of the patients who could receive the same medical treatment in case of necessity were compared; mean cost of the patients were found to be $ 665.44 for the patients treated in AIC, $ 204.09 for patients treated in EDs and $186.85 for those received treatments in the psychiatric clinic. We defined that it would be profitable if the intoxication cases were followed-up in the ED observation units and that ED’s could be used more effectively than ICUs.
Keywords
cost,intoxication, emergency observation, patient follow-up, suicide
Introductıon
Suicidal behavior is increasing over the years in many countries and is recognized as a universal problem today. According to data from World Health Office (WHO) more than 800,000 persons die by suicide annually [1].
Today, poisoning-related suicide attempts are one of the most common cases of suicides, and this is a sociocultural problem which continues to affect human life in various ways. Intake of medicines for suicide is wide in the developed countries, while accidental poisoning is more common in the other countries. Today, this issue remains important because of both health costs and sociocultural impacts [2-3].
According to 2011 data derived from 57 poison control centers in the USA, approximately 2.3 million poisoning cases (0.74%) have been reported. Of more than 2 million suicide cases which occurred in the USA, 78% were reported to be treated at home without presenting to the Emergency Departments [1].
Despite suicidal attempts being one of the most important problems encountered in the EDs in our country, it is difficult to reach to a reliable morbidity and mortality statistics due to the lack of proper records.
The number of poisoning cases admitted to the EDs account for 0.46-1.57% of all cases [4,5]. Poisoning cases may result in severe outcomes depending on the factors and duration of hospital stay. Some of these patients may require to stay in the ICU for further care following an accurate and effective treatment in EDs [4,6]. Unfortunately since the number of beds are limited in ICUs, it is thought that increasing the number of intermediate intensive care units or emergency observations would result in better and inexpensive service for the follow-up of these patients.
Objective of this study was to reveal our societal lacks resulting from a retrospective examination of suicidal attempts that lead to both heavy medical expenses and sociocultural damage and shed light on the mortality and morbidity data of drug intoxication.
Methods
Patient population and study design
A total of 791 adult patients presented for drug intoxication, hanging, alcohol intoxication and organophosphate drug intake to our ED, between January 2007 and December 2012 were included in the study. All patients had undergone acute treatment and also had consultation with the psychiatry clinic before discharge. They were retrospectively examined and their clinical and demographic data were analyzed. A comparative study was done on the cost of treatment of these patients in the ED, intensive care units and psychiatric clinics.
Results
Statistical analysis
Anova, t-test, correlation analysis and Roc analysis were used for the continuous data, while Chi-square test was used for the classifications. Descriptive statistics were expressed as the case numbers and percentage (%). The data showing a normal distribution were expressed with mean + standard deviation. Values of p<0.05 were considered statistically significant.
Experimental study
Mean age of the total patient group was 28.78±11.98 years. As a breakdown: mean age of the patients with unknown cause of taking drugs was found as 23.50±2.34 years, while mean age of the patients with suicidal drug taking was 28.69±0.44 years and accidental drug taking was 29.18±1.62 years.
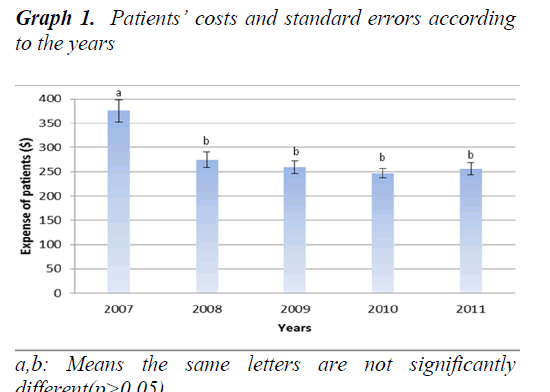
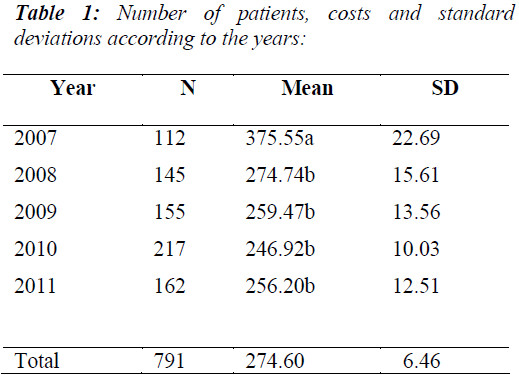
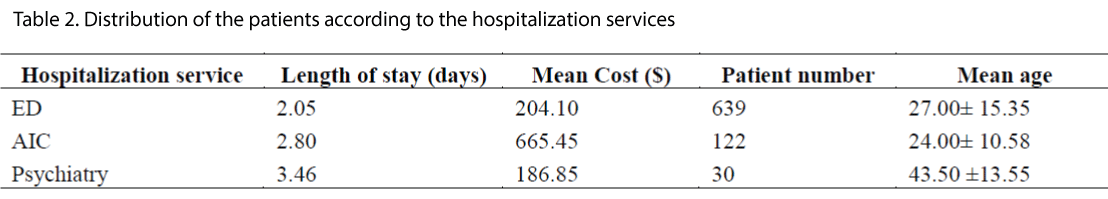
Number of the patients presented to our ED due to suicide is given in Table 1. Among the patients who could receive the same treatment in case of necessity, mean cost of the patients hospitalized in AIC was found as $665.45, in ED as $204.10 and in the psychiatric clinic as $186.85 (Graphic 1).
When suicide attempts were classified according to the months of birth; patients born in January were the most common to attempt suicide (n:227, 28.7%) while patients born in December were the least to do so (n:30, 3.8%). No significant correlation was found in terms of the months and seasons (p>0,05).
When the suicidal patients were classified according to the month of suicidal attempts; most attempts were observed in December (n:83,10.5%) while the least attempts were in May (n:44, 5.6%). This classification was carried out in order to understand whether there was a difference between education season and summer holiday, but no significant difference was found between the months (p>0,05).
When the patients were analyzed according to the departments of hospitalization; 122 (15.4%) patients were followed-up in AIC, 639 (80.8%) in ED and 30 (3.8%) in the psychiatric clinic. Twenty-nine (3.7%) of the patients hospitalized in ED and were referred to the psychiatric clinic (Table 2).
When length of stay in ED was analyzed no significant difference was found. Mean length of stay was found to be 2.81 hours and standard deviation as 0.9814 in the patients who were hospitalized in ED.
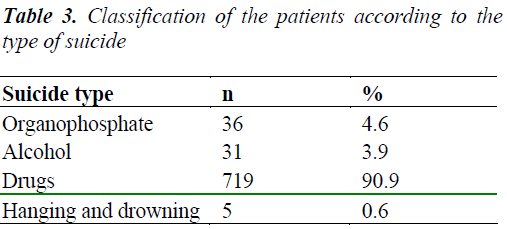
When the patients were grouped according to the types of suicide; 36 (4.6%) of the patients presented with organophosphate intake, 31 (3.9%) alcohol intake, 719 (90.9%) drug intake and 5 (0.6%) due to hanging or drowning (Table 3). Of the patients, 9 (1.1%) were lost, while 23 (2.9%) rejected the treatment with the approval of his/her companion. Of the patients, 759 (96%) were treated and discharged from ED.
When the causes of taking suicidal drugs were examined; history was unknown for 8 patients (1%) since they did not answer the anamnesis question, while 738 (93.3%) reported suicidal drug intake and 45 (5.7%) accidental intake. Accidental intakes occurred due to unintentionally intake of hydrochloric acid, bleach and pesticides found in the kitchen or cellar.
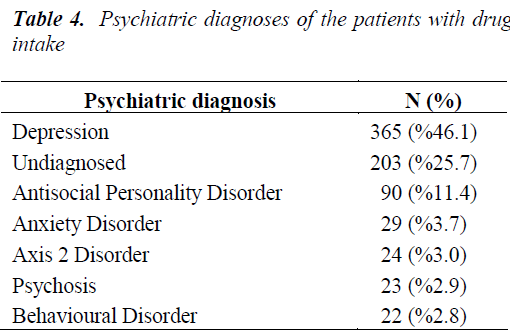
When the patients were analyzed according to their backgrounds; 743 (93.9%) patients were unremarkable.When the psychiatric diagnoses were analyzed; diagnosis of depression was established in 365 (46.1%) patients; while no diagnosis was set in 203 (25.7%) patients in the acute period (Table 4). Diagnosis of depression was set in the subsequent examinations in 152 (74.9%) of the patients who could not be diagnosed in the acute period.
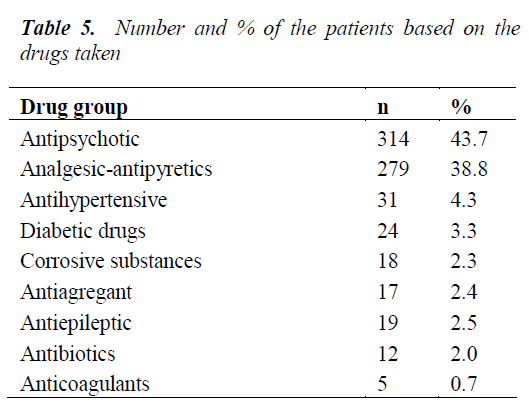
When the patients were analyzed in terms of the drugs taken; 503 (63.6%) had been suicidally exposed to chemicals with multiple drug intake and 288 (36.4%) with single drug intake. Of the drugs taken, 204 (25.8%) were antipsychotic, 135 (17.1%) analgesic and antipyretics (Table 5).
When supply of the drugs was analyzed; history could not be obtained in 91 (11.5%) patients, 427 (54%) patients were found to be poisoned using drugs of their families, 187 (23.6%) using their own drugs, 4 (0.5%) by drugs bought from a pharmacy and 82 (10.4%) using the chemicals found in the home. The type of drug taken was not correlated with the length of stay in the hospital, while it was found to be correlated with waiting time in ED (p< 0.001).
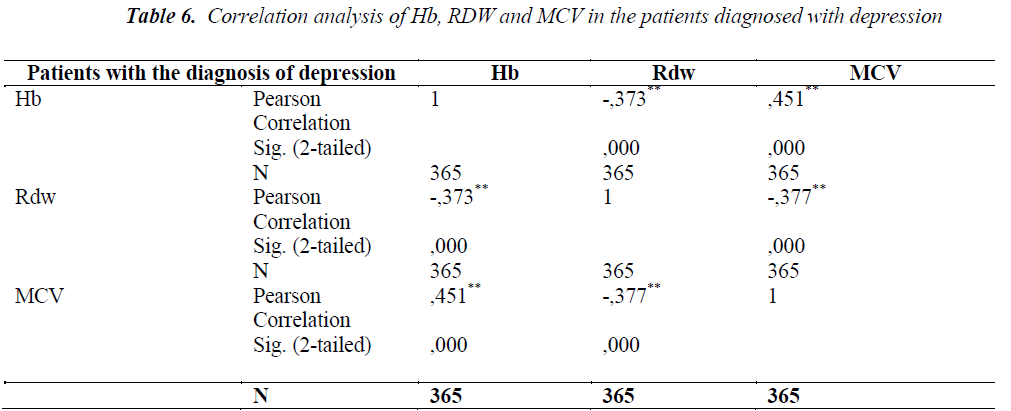
Correlation analysis carried out yielded a significant correlation between Hb, RDW and MCV in the patients having the diagnosis of depression, while these values were not correlated in the other diagnoses (Table 6).
Discussion
Poisoning is a clinical condition developing from taking a drug or a toxic substance via various ways and at a level to damage the body, which occasionally results in death.
Poisoning has been one of the major problems that concerns the society since ancient times [7]. Even if small amounts of any substance; chemical, physical or organic; which is ingested, inhaled, absorbed or injected, results in damage to the structures and impair the functions, this substance is called as poison, and this event is known as poisoning. [8].
Poisoning cases are frequently encountered in EDs and some of these patients require to be treated in ICUs. Although the condition of a patient presented wit poisoning may seem to be stable at first; consideringh poisoning may seem to be stable at first; considering effects of the drug is time-dependent and patient’s condition may rapidly change, these patients should be monitored in ED or in a service having monitoring facilities where intervention can be done quickly when needed [9].
There are several studies in the literature investigating suicidal attempts with drugs in terms of age groups. When such attempts were analyzed in terms of mean age; Pekdemir et al. found the mean age as 28.28±13.4 [10] and Serinken et al. as 24.5±5.7 [11], while in our study the mean age of suicide cases was found as 28.78±11.98. In a study conducted by Kaygusuz et al. with 245 adults treated in the intensive care unit; 35.5 % of the patients were found to be in the age range of 14-20 years and 36.7% in the range of 21- 30 years [12]. No significant difference was found in the three studies in terms of the mean age. According to 2013 report of American Centers for Disease Control and Prevention (CDC) [13], suicide cases were most common in the age range of 15-34 years. Whereas in our study, mean age was found to be 27.00± 15.35 in patients treated in ED (80.78%), 24.00± 10.58 in patients treated in AIC (15.42%) and 43.50 ±13.55 in those treated in the psychiatry clinic (3.79%).
In our study female:male patient ratio was found to be 70.3.% : 29.7%, while in other studies the following female:male patient ratios have been reported: Pinar et al., 57.5% : 42.5% [14], Göksu et al., 64.8% : 35.3% [15], Kurt et al. 60.2% : 39.8% [16], Kekeç et al., 60% : 40% [17], Akbaba et al. 67.6% : 32.4% [18], and Serinken et al. 86.3% :13.7% [11].
There are numerous studies in the literature about the poisoning agents used for suicides. Pekdemir et al. found antidepressant drugs as the the most common agent (16.9%) [10]. In a study by Kaygusuz et al; the most common drug exposure was antidepressants by 46.1% and multiple drug intake by 53.5% [12].In a study by Pınar et al conducted with all age groups between 1989 and 1990; 16.8% were defined as analgesic, 9.7% pesticides, 8.7% ethanol, 7.7% anticonvulsants; 7.0% caustic, 6.0% tricyclic antidepressant, 5.4% hydrocarbon, 5.1% antihist-aminic and 4.7% carbon monoxide poisoning according to the drug substance, while the mortality rate was found as 0.8% [14]. In a 1-year, data review by Özköse et al. with 228 adult poisoning cases; 75.8% of the cases were found to be poisoned, while 29.7% of these cases were found to be through analgesics with 78.9% of these cases were suicidal [19]. In a study by Kurt et al. in Aydın region; 34.7% of the patients who were poisoned intentionally exposed to the chemicals [16]. In a study by Kekeç et al. in Kayseri region; 54.5% of the substances taken in the poisoning cases were drugs and 80% of the patients intentionally exposed to the chemicals [17]. When in our study suicide cases were analyzed in terms of the drug groups; 503 patients (63.6%) have taken multiple drugs, while 288 (36.4%) patients have taken single drug or chemical. Of the drugs taken; 204 (25.8%) were antipsychotic and 135 (17.1%) analgesics and antipyretics. We attributed this to the fact that mental and depressive disorders are becoming more common now-a-days, and that these drugs can be readily obtained from pharmacies without a prescription.
When drug intoxication cases were grouped according to the years; an increase was seen from 2007 to 2010 with a peak value of 217 in 2010 which decreased in 2011. Number of the patients were observed to decrease in parallel to the awareness raising work and increase in the number of psychotherapy work in the hospitals.
Today, number of the beds in ICUs is insufficient. Cost of the poisoning cases treated in the ICUs is higher due to insufficient number of staff and high operational expenditures of the technological equipments used. In our study, mean cost of the suicide patients treated in ED was found to be $204.10, while it was $665.45 if treated in the AICs. In a study conducted by Serinken et al. with 219 suicide patients (2006); mean cost of the patients treated in the ED was found to be $125.95, while it was found to be $358.23 for the patients treated in the other hospital services.
Conclusion
In conclusion:
1. Use of antidepressants and antipsychotics as suicidal drugs have increased as these are easily found at home.
2. Given the fact that the persons accidentally exposed to dangerous chemicals are mostly the elderly and women; we defined, as a protective factor, that women should be carefully protected from the chemicals they use at home and that dispensing drugs to the elderly, specially neuropsychiatric drugs should be done by their relatives.
3. In numerous studies; differences in female to male ratio and accidental or suicidal intaking of the chemical substances was attributed to regional sociocultural changes and adaptation of the young population to that culture.
4. In our study, we found that a profit of 461.35$ could be made by following-up the patients in EDs and in this way, ICUs could be used more effectively for other patients.
Acknowledgements
The authors thank the Refik Saydam Hygiene Center of Ankara, Turkey for testing the serum samples, and our colleagues from the Turkish Ministry of Health for their contributions.
Conflict of interest
No conflict of interest and no funding source to declare.
Ethical approval
The study was performed in accordance with the Declaration of Helsinki for Human Research, and was approved by the institutional ethics committee.
References
- 2011 Annual Report of the American Association of Poison Control Centers ’ National Poison Data System (NPDS): 29th Annual Report
- Comtois KA, Linehan MM. Psychosocial treatments of suicidal behaviors: A practice-friendly review. Journal of Clinical Psychology: In Session, 2006; 62 (2), 161- 70.
- Wax PM. History. In: Goldfrank LR, Flomenbaum NE. Toxicologic Emergencies (Ed 6th) New York, McGraw- Hill 1998:1-14.
- Akkose S, Fedakar R, Bulut M, Cebicci H. Epidemiology of Poisoning in Adults: A 5 Year Study. Turkish Journal of Emergency Medicine 2003; 3: 8-10.
- Yavuz S, Aydin S. The profile of the poisoned cases.The Turkish Journal of Toxicology 2003; 1: 47-52.
- Senol V, Yildirim C, Sozuer E, Ozturk Y. An Epidemiology of Homicide and Suicide Cases in Emergency Department.Tr J Emerg Med 2002; 2 : 18- 23.
- Chirasirisap K, Ussanawarong S,Tassaneeyakul W et al. A study of major causes and types of poisoning in Khonkaen,Thailand, Vet Hum Toxicol 1992; 34: 489-92.
- http://www.acilveilkyardim.com Erisim tarihi 05. 07.2007
- Tintinalli EJ, Kelen GD, Stapczynski JS. Emergency Medicine A Comprehensive Study Guide. 5th ed. USA: McGraw-Hill, 1999:1057-63, 1103-25, 1182-5.
- Pekdemir M, Yildiz M, Durukan P, Kavalci C. Evaluation of Poisining Cases Presented to Our Emergency Department. Tr J Emerg Med. 2002; 2: 36-40
- Serinken M, Karcioglu O, Sengul C, Turkcuer I, Keysan MK. Hospital Costs of Managing Deliberate Self-Poisoning in Turkey. Med Sci Monit, 2008; 14: CR152-58
- Kaygusuz K, Gursoy S, Kiliccioğlu F, Ozdemirkol Đ, Mimaroglu C. The Retrospective Analysis of the Cases that were Observed with the Diagnosis of Acute Drug Intoxication in the Intensive Care Unit of Cumhuriyet University Medical Faculty Hospital Between 1998- 2004 Years. Cumhuriyet Medical Journal 2004;26:161-5
- CDC Health Disparities and Inequalities Report — United States, 2013
- Pinar A, Fowler J, Bond GR, Acute Poisoning in Izmir, Turkey- A Pilot Epidemiologic Study. J Toxicol Clin Toxicol. 1993; 31: 593-601
- Ozkose Z, Ayoglu F, Etiological And Demographical Characteristics Of Acute Adult Poisoning Đn Ankara, Turkey. Human & Experimental Toxicology. 1999; 18: 614-618
- Kurt Đ,Erpek AG, Kurt MN, Gurel A. Epidemiology of Adult Poisoning at Adnan Menderes University. Journal of Adnan Menderes University Medical Faculty 2004; 5: 37-40
- Kekec Z, Gunay N, Zozuer EM, Guven M, Sungur M. An analysis of 682 adult poisonings in central Anatolia of Turkey. Vet HumToxicol. 2004; 46: 335-336