ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 1
Correlation between blood glucose levels on admission and short-term prognosis of in-patients with acute coronary syndromes after percutaneous coronary intervention
Department of cardiothoracic surgery, Changzheng HospitalSecond Military Medical University, Shanghai, PR China
#Contribute equally to this article and should be considered as co-first authors
- *Corresponding Author:
- Wang Zhinong
Department of cardiothoracic surgery
Changzheng Hospital
Second Military Medical University
PR China
Accepted date: June 06, 2016
Objective: This research aimed to investigate the influence of admission glucose level on the short-term outcomes after percutaneous coronary intervention.
Methods: 750 consecutive patients who underwent PCI after acute coronary syndrome during December 2011 and December 2013 were investigated and divided into three groups according to their admission glucose level: Group I (ABG<7.8 mmol/l), group II (7.8 mmol/l ≤ ABG<11.1 mmol/l), group III (ABG ≥ 11.0 mmol/l). In-hospital and 6-month complications were analysed and compared between the three groups.
Results: In-hospital mortality was 0.7% in group I, 3.1% in group II, and 6.8% in group III; six-month mortality was 2.4% in group I, 4.7% in group II, and 13.7% in group III. Multivariate logistic regression showed that admission glucose level ≥ 11.0 mmol/l was an independent risk factor related to in-hospital and six-month mortality in percutaneous coronary intervention after acute coronary syndrome.
Conclusion: In patients undergoing percutaneous coronary intervention after acute coronary syndrome, admission glucose level was predictive of short-term outcome. Early treatment of high glucose in perioperative time may benefit these patients.
Keywords
Acute coronary syndrome, Percutaneous coronary intervention, Blood glucose, prognosis
Introduction
Diabetes has been regarded as an equivalent risk of coronary heart disease for a long time. The short and long-term mortality rates of myocardial infarction patients with diabetes mellitus are higher than those without diabetes [1]. However, study of Goya et al. [2] found that predict mortality of blood glucose levels on admission in patients with acute myocardial infarction (AMI) is stronger than diabetes itself regardless of whether there is a history of diabetes, admission AMI patient with blood glucose ≥ 144 mg/dL has higher risk of death. In fact, most patients with acute coronary syndrome (ACS) has elevated blood glucose levels on admission, except in patients with previous history of diabetes, there is a part of patients with stress hyperglycaemia. The predictive value of blood glucose levels on admission to the prognosis of patients with ACS have been confirmed by a lot of studies [3,4]. Hyperglycaemia on admission in patients with AMI cause short and long term mortality increased, the incidence of adverse events also increased today, however, PCI has been the first-line treatment measure of ACS, Research of whether hyperglycaemia on admission in patients with ACS has influence of prognosis undergoing PCI treatment is less, what manner of blood glucose control in these patients has no clear criteria. Therefore, this study focuses on exploring the impact of short-term prognosis of hyperglycaemia on admission of patients with ACS performed PCI.
Subjects and Methods
Study objects
From September 2011 to September 2013, patients, due to ACS, which include unstable angina (UA), non-ST-Elevation Myocardial Infarction. (NSTEMI) and ST-Elevation Myocardial Infarction (STEMI) in our hospital (Changzheng) perform PCI, Study group 773 Patients with Acute Coronary Syndrome (ACS) who were treated with PCI in Changzheng Hospital from September 2011 to September 2013, including Unstable Angina (UA), Non-ST-Elevation Myocardial Infarction (NSTEMI) and ST-Elevation Myocardial Infarction (STEMI), referring to the United States and Europe’s acute coronary syndrome guidelines in 2013, total 773 cased were included. We excluded 13 cases due to admission blood glucose data missing, 10 cases re-hospitalized for treatment in 6 months, finally included 750 cases. All patients’ venous glucose levels were measured within 2 hours after admission, and were divided into three groups, normal blood glucose group (ABG<7.8 mmol/l), normal-high ABG group (7.8 mmol/l ≤ ABG<11.1 mmol/l), high ABG group (ABG ≥ 11.0 mmol/l).
Observed indication
Basic clinical data of all patients included age, gender, and history of hypertension, diabetes, hyperlipidaemia, chronic renal function insufficiency, chronic obstructive lung disease, smoke history, myocardial infarction, vascular reconstruction and stroke, acute heart failure, and severe arrhythmia. Upon admission, clinical measurements include blood glucose, haemoglobin, albumin, creatinine, uric acid, glutamic pyruvic transaminase, aspartate aminotransferase, and myocardial enzyme (CK-MB). PCI surgical treatment data included location of coronary artery lesions, stent implantation, etc. complications during hospitalization included death, bleeding, acute stent thrombosis, ischemia reperfusion arrhythmia and contrast induced nephropathy; 6 months postoperative complications included death, major cardiovascular events (i.e., myocardial re infarction, revascularization treatment).
Relevant definitions
Definitions followed the 2011 American Heart Interventional Treatment Guidelines. The definition of severe arrhythmias: atrial fibrillation, atrial flutter, paroxysmal supraventricular tachycardia, ventricular tachycardia, ventricular fibrillation, atrioventricular block and sick sinus syndrome. Ischemia reperfusion arrhythmia was defined as: ventricular fibrillation, sustained ventricular tachycardia, new onset of atrial fibrillation and atrial flutter, high degree atrioventricular block and severe bradycardia during PCI and 24 hours after PCI. Contrast nephropathy was defined as either a greater than 25% increase of serum creatinine or an absolute increase in serum creatinine of 0.5 mg/dL, 48 hours after use of iodine contrast agent without another clear cause for kidney injury.
Instruments and equipments
Blood glucose and other related biochemical indexes were tested by Roche Cobas C 701 automatic analysis system and its accessioned reagent (Roche, Germany). Routine blood tests were completed using SYSMEX XN-2000 automatic blood cell analyser and related reagents (SYSMEX, Japan), Troponin was measured by RAMP 200 fluorescence immunity analyser and related reagents (Response Biomedical Co., Canada ), PCI for all patient, was used SIEMNS Artis Zee Floor vascular imaging system (SIEMENS) for all patients.
Statistical method
Statistical analysis was performed using SPSS version 18.0. Discrete data measured from different groups are presented as mean ± standard deviation, and enumeration data is expressed by percentage (%). Measured data were analysed with paired t test while the enumeration data were analysed with χ2 test or the Fischer exact probability method (when sample data was insufficient). The suspected factors affecting PCI complications were analysed by univariate analysis. The factors that had P<0.20 from the univariate analysis were subsequently analysed by logistic multivariate analysis. Statistical significance was defined as a p<0.05.
Results
Clinical data of admission cases
The patients were grouped based on admission blood glucose level, where 549 (73.2%) cases constituted the normal ABG group (ABG<7.8 mmol/L), 128 (17.1%) were in the normalhigh ABG group (7.8 mmol/l ≤ ABG<11.1 mmol/l), and 73 cases were placed into the high ABG group (ABG ≥ 11.0 mmol/l). Table 1 lists basic clinical data of the 3 groups. The average admission ABG of the three groups was 5.44 ± 0.93 mmol/l, 8.90 ± 0.96 mmol/l, and 13.94 ± 2.71 mmol/l respectively. Compared with the other two groups, the proportion of patients with previous history of diabetes in high ABG group is significantly higher. (68.5% vs. 41.4% vs. 12.5%, P<0.01), in which the ratio of STEMI was the highest. Meantime, in high ABG group more patients with hypertension and chronic renal failure etc. complications. On admission, patients with acute heart failure were significantly more than the other two groups. However, the three groups of patient’s age and gender have no significant difference and proportion of patients who smoking is roughly the same. At the same time, the incidences of chronic obstructive pulmonary disease, peripheral vascular disease and hyperlipidaemia were also similar. Compared with the other two groups, high ABG group’s patients with old myocardial infarction, previous stroke history and history of vascular remodelling were not significantly increased.
| Variable | Normal ABG (n=549) | Normal High ABG (n=128) | High ABG (n=73) | P |
|---|---|---|---|---|
| AGE | 63.97 ± 11.10 | 63.83 ± 11.57 | 62.16 ± 11.62 | 0.44 |
| ABG (mmol/l) | 5.44 ± 0.93 | 8.90 ± 0.96 | 13.94 ± 2.71 | <0.01 |
| Female (%) | 122 (22.2) | 32 (25) | 18 (24.7) | 0.75 |
| Smokers (%) | 274 (49.9) | 67 (52.3) | 34 (46.6) | 0.82 |
| Diabetes (%) | 70 (12.8) | 53 (41.4) | 50 (68.5) | <0.01 |
| Preoperative diagnosis | <0.01 | |||
| UAP | 309 (56.3) | 45 (35.2) | 25 (34.2) | |
| Acute ST segment elevation myocardial infarction STEMI | 198 (36.1) | 67 (52.3) | 39(53.4) | |
| Acute non ST segment elevation myocardial infarction NSTEMI | 42 (7.7) | 16 (12.5) | 9 (12.3) | |
| Complications | ||||
| Hypertension (%) | 358 (65.2) | 93 (72.7) | 54 (74) | <0.05 |
| Chronic renal insufficiency (%) | 21 (3.8) | 3 (2.3) | 8 (11) | <0.05 |
| Chronic obstructive pulmonary disease (%) | 19 (3.5) | 3 (2.3) | 3 (4.1) | 0.97 |
| Peripheral vascular disease (%) | 38 (6.9) | 9 (7.0) | 7 (9.6) | 0.48 |
| Hyperlipidaemia (%) | 47 (8.6) | 16 (12.5) | 8 (11.0) | 0.25 |
| OMI (%) | 33 (6.0) | 13 (10.2) | 6 (8.2) | 0.19 |
| History of stroke (%) | 46 (8.4) | 14 (10.9) | 9 (12.3) | 0.19 |
| Previous PCI/CABG history (%) | 37 (6.7) | 13 (10.2) | 5 (6.8) | 0.53 |
| Acute heart failure (%) | 28 (5.1) | 12 (9.4) | 11 (15.1) | <0.01 |
| Severe arrhythmia (%) | 61 (11.1) | 19 (14.8) | 12 (16.4) | 0.11 |
Table 1: The basic clinical data of three groups based on the admission blood glucose level.
Data related to PCI surgery
Compared with the other two groups, the high ABG group had a greater proportion of emergency PCI treatments, and a high proportion of femoral artery approach PCI. Furthermore, the proportion of three coronary artery lesions of high ABG group was higher; the left circumflex artery lesions appeared even more. However, there was no significant difference among three groups for anterior descending artery and right coronary artery lesions as well as combined left main coronary artery lesions. In PCI treatment, there was no significant difference among 3 groups of drug-eluting stents (97.3% vs. 96.1% vs. 95.9%, P=0.4), the same as the number of stents implanted (Table 2).
| normal ABG (n=549) | NORMAL HIGH (n=128) | HIGH ABG (n=73) | ||
|---|---|---|---|---|
| Emergency PCI (%) | 110 (20) | 43 (33.6) | 26 (35.6) | <0.01 |
| Femoral artery approach (%) | 89 (16.3) | 31 (24.2) | 20 (27.4) | <0.01 |
| DES implantation (%) | 534 (97.3) | 123 (96.1) | 70 (95.9) | 0.40 |
| Number of SI | 1.45 ± 0.69 | 1.49 ± 0.76 | 1.41 ± 0.74 | 0.71 |
| Three coronary artery lesions (%) | 240 (43.7) | 65 (50.8) | 41 (56.2) | <0.05 |
| Lesion site | ||||
| LAD (%) | 507 (92.3) | 118 (92.2) | 70 (95.9) | 0.38 |
| LC (%) | 323 (58.8) | 81 (63.3) | 52 (71.2) | <0.05 |
| RCA (%) | 364 (66.3) | 95 (74.2) | 53 (72.6) | 0.09 |
| LMCA (%) | 33 (6.0) | 13 (10.2) | 4 (5.5) | 0.54 |
| Calcified (%) | 100 (18.2) | 22 (17.2) | 12 (16.4) | 0.68 |
Table 2: PCI treatment of three groups of patients based on admission blood glucose level.
The conclusion of three groups cases after PCI in hospital and 6 months after operation
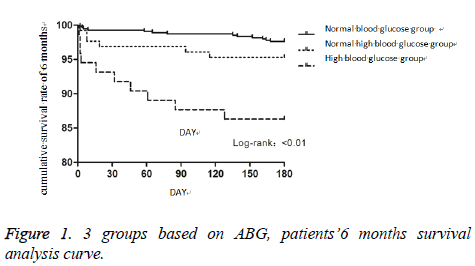
Results of three groups of patients with PCI in hospital and 6 months after operation were summarized in Table 3. (Regrouping refer to the history whether or not have diabetes) In patients complicated with diabetes mellitus, the three groups were not significantly different for total number of days in hospital and the number of postoperative hospital stay. The three groups in hospital mortality rate in accordance with admission blood glucose levels from low to high has the increasing trend, but there was no statistical difference, which was 1.4%, 3.8%, 6% respectively. Meanwhile there were no significant differences among 3 groups for the contrast agent nephropathy, arrhythmia complications and bleeding complications during the hospitalization. In the short term prognosis of 6 months, the morality of the three groups increased respectively (2.9% vs. 5.7% vs. 16%, P=0.022). There were no significant differences of the cumulative survival rate of 6 months between normal ABG group and normal-high ABG group (χ2=2.102, p=0.147), however the high ABG compared with the other two groups showed significant differences (χ2=24.993, p<0.01 vs. normal ABG group, χ2=5.238, p=0.022 vs. normal-high ABG group) (Figure 1). Compared with the other two groups, high ABG group showed no significant differences in the rates of palindromic myocardial infarction, revascularization and in the incidence of major cardiovascular events after operation for 6 months. In the high ABG group, the admission morality of patients without diabetes significantly increased (0.6% vs. 2.7% vs. 8.7%, P<0.01), and the incidence of bleeding complications and contrast induced nephropathy were also higher, but arrhythmic complications showed no significant difference in the three groups. 6 months after surgery, all the complications, including death, showed no differences in the three groups. There was no significant relationship between the levels of ABG and rates of re-infarction and treatment rates of revascularization in 6 months after operation.
| Diabetes (173) | No diabetes (577) | |||||||
|---|---|---|---|---|---|---|---|---|
| NORMAL ABG GROUP (n=70) | NORMAL HIGH ABG (n=53) | HIGH ABG (n=50) | P | NORMAL ABG (n=479) | NORMAL HIGH ABG (n=75) | HIGH ABG (n=23) | P | |
| In hospital conclusion | ||||||||
| Total in hospital (DAY) | 7.40 ± 4.94 | 8.39 ± 4.48 | 8.36 ± 5.14 | 0.432 | 6.90 ± 3.41 | 7.33 ± 2.87 | 6.78 ± 2.86 | 0.565 |
| Days after operation (DAY) | 4.74 ± 4.72 | 5.00 ± 3.46 | 6.28 ± 5.48 | 0.18 | 4.49 ± 3.34 | 5.76 ± 3.33 | 4.78 ± 3.13 | 0.010 |
| Death | 1 (1.4%) | 2 (3.8%) | 3 (6.0%) | 0.398 | 3 (0.6%) | 2 (2.7%) | 2 (8.7%) | <0.01 |
| Contrast-induced nephropathy | 3 (4.3%) | 1 (1.9%) | 3 (6.0%) | 0.566 | 1 (0.2%) | 1 (1.3%) | 1 (4.3%) | 0.015 |
| Bleeding complications | 3 (4.5%) | 5 (9.4%) | 3 (6.0%) | 0.553 | 21 (4.4%) | 3 (4.0%) | 5 (21.7%) | 0.001 |
| Complications of arrhythmia | 0 (0.0%)) | 3 (5.7%) | 2 (4.0%) | 0.153 | 8 (1.7%) | 1 (1.3%) | 2 (8.7%) | 0.052 |
| Six months after the operation. | ||||||||
| Death | 2 (2.9%) | 3 (5.7%) | 8 (16.0%) | 0.022 | 11 (2.3%) | 3 (4.0%) | 2 (8.7%) | 0.148 |
| Reinfarction | 1 (1.4%) | 2 (3.8%) | 1 (2.0%) | 0.682 | 7 (1.5%) | 0 (0.0%) | 0 (0.0%) | 0.484 |
| Repeated Revascularization therapy | 11 (15.7%) | 9 (17.0%) | 11 (22.0) | 0.661 | 63 (13.2%) | 10 (13.3%) | 5 (21.7%) | 0.503 |
| Major cardiovascular events | 12 (17.1%) | 12 (22.6%) | 17 (34.0%) | 0.099 | 78 (16.3%) | 14 (18.7%) | 8 (34.8%) | 0.069 |
Table 3: Conclusions of three groups based on admission blood glucose level in hospital and 6 months after operation.
Univariate and multivariate logistic regression analysis showed the independent risk factors associated with patients with acute coronary syndrome PCI treatment were admission acute heart failure, chronic renal insufficiency, blood glucose>11.1 mmol/l and emergency PCI. And in addition to the above 4 factors, the independent risk factor in 6 months after operation was age (Table 4).
| Variable | Wald χ2 | OR | 95% CI | P |
|---|---|---|---|---|
| In hospital morality | ||||
| Abg | 5.365 | 0.068 | ||
| Blood glucose>7.8 mmol/l | 0.272 | 1.356 | 0.432-4.256 | 0.602 |
| Blood glucose>11.1 mmol/l | 5.332 | 3.348 | 1.200-9.338 | 0.021 |
| Chronic renal insufficiency | 16.398 | 11.646 | 3.549-38.211 | <0.01 |
| Emergency PCI | 17.467 | 7.793 | 2.975-20.413 | <0.01 |
| Acute heart failure at admission | 14.814 | 6.578 | 2.521-17.167 | <0.01 |
| Postoperative 6-month mortality | ||||
| Abg | 6.830 | 0.033 | ||
| Blood glucose>7.8 mmol/l | 0.337 | 1.411 | 0.442-4.504 | |
| Blood glucose>11.1 mmol/l | 6.789 | 3.993 | 1.409-11.316 | 0.009 |
| Age (Every ten years old increase) | 6.310 | 1.678 | 1.120-2.512 | 0.012 |
| Chronic renal insufficiency | 13.662 | 9.424 | 2.868-30.962 | <0.01 |
| Emergency PCI | 18.292 | 8.050 | 3.095-20.936 | <0.01 |
| Acute heart failure at admission | 14.931 | 6.364 | 2.489-16.269 | <0.01 |
Table 4: Independent predictors of mortality in patients with acute coronary syndrome in hospital and after surgery.
Discussion
Abnormal glucose metabolism is found in patients with acute coronary syndrome, which was found in patients with diabetes and in patients without previously diagnosed diabetes. It is reported that AMI patients with admission hyperglycaemia significantly associated with mortality [5], even for patients with emergency PCI, its short-term, long-term mortality was also significantly correlated with admission hyperglycaemia. In the era of PCI treatment, there are some studies [6] have found, hyperglycaemia on admission of patients undergoing PCI were independent predictors of prognosis in acute coronary syndrome, patients’ postoperative short-term and long-term mortality is higher in hyperglycaemia patients than normal blood sugar patients. In this study, by analysing 750 ACS patients treated with PCI, we found a highly correlation between the blood glucose level at admission and the short term prognosis of ACS patients treated with PCI. Mortality rate of patients in high ABG group and the incidence of adverse events were both higher than that patients in normal and normal high ABG group no matter in hospital or half year after the surgery, which was consistent with many previous studies [7-9]. In this study, we also found that the morality of patients without diabetes and high blood glucose patients was significantly increased. And incidence of other perioperative complications was high; suggesting that stress hyperglycaemia was associated with adverse prognosis of ACS patients during the perioperative of PCI. And in patients with diabetes, mortality rate of three groups of patients in hospital had no significant difference, but the morality rate of high blood glucose group was increased significantly 6 months after operation, suggesting that both stress hyperglycaemia and diabetes itself may affect short-term prognosis of patients with ACS after PCI.
There are many reasons for hyperglycaemia in ACS patients, and we have shown that diabetes was one of the most important factors. The proportion of high blood glucose patients with diabetes history was the highest. However, in our study we did not find that diabetes was the leading cause in terms of independent factors of poor prognosis. Therefore, other factors may also play a role. The probable reasons included: 1. patients with occult diabetes, the result of oral glucose tolerance test decreased in patients with myocardial infarction, but they were not diagnose as diabetes without clinical diabetic symptoms. In fact, diabetes is risk factors for coronary heart disease, and its effect on the coronary possible start at earlier stages to reduce the oral glucose tolerance test [10]. In fact, Norhammar et al. found that after an oral glucose tolerance test, 31% of AMI patients whose blood glucose was lower than 11.1 mmol/l were diagnosed with impaired glucose tolerance and diabetes 2 [11]. Stress hyperglycaemia-due to sympathetic excitement in ACS patients, hyperglycaemia may result due to the increased glucagon and blood glucose release hormones [12]. The stress hyperglycaemia can aggravate heart inflammation, apoptosis and accelerate the coagulation process, which can cause an increase in the area of myocardial infarction, decreased and left ventricular ejection fraction and other poor prognoses.
High blood glucose at admission in ACS patients after PCI had poor prognosis, thus emphasising the need for PCI perioperative glycaemic control [13,14]. Although studies have shown that insulin has a protective effect on acute myocardial infarction, more clinical data is needed to determine whether conventional insulin therapy that will be implemented on patients with high blood glucose on admission.
References
- Donahoe SM, Stewart GC, McCabe CH. Diabetes and mortality following acute coronary syndromes. Jama 2007; 298: 765-775.
- Goyal A, Mehta SR, Gerstein HC. Glucose levels compared with diabetes history in the risk assessment of patients with acute myocardial infarction. American heart journal 2009; 157(4): 763-70.
- Kosiborod M, Inzucchi SE, Krumholz HM. Glucometrics in patients hospitalized with acute myocardial infarction: defining the optimal outcomes-based measure of risk. Circulation 2008; 117: 1018-27.
- Goyal A, Mahaffey KW, Garg J. Prognostic significance of the change in glucose level in the first 24 h after acute myocardial infarction: results from the CARDINAL study. Europ heart J 2006; 27: 1289-1297.
- Foo K, Cooper J, Deaner A. A single serum glucose measurement predicts adverse outcomes across the whole range of acute coronary syndromes. Heart 2003; 89: 512-516.
- Planer D, Witzenbichler B, Guagliumi G. Impact of hyperglycaemia in patients with ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention: the Horizons-Ami trial. Inter J cardiol 2013; 167(6): 2572-2579.
- Pres D, Gasior M, Strojek K. Blood glucose level on admission determines in-hospital and long-term mortality in patients with ST-segment elevation myocardial infarction complicated by cardiogenic shock treated with percutaneous coronary intervention. Kardiologia polska 2010; 68: 743-751.
- Straumann E, Kurz DJ, Muntwyler J. Admission glucose concentrations independently predict early and late mortality in patients with acute myocardial infarction treated by primary or rescue percutaneous coronary intervention. Am heart J 2005; 150: 1000-1006.
- Vis MM, Sjauw KD, van der Schaaf RJ. In patients with ST-segment elevation myocardial infarction with cardiogenic shock treated with percutaneous coronary intervention, admission glucose level is a strong independent predictor for 1-year mortality in patients without a prior diagnosis of diabetes. Am heart J 2007; 154: 1184-1190.
- Cameron A. The metabolic syndrome: validity and utility of clinical definitions for cardiovascular disease and diabetes risk prediction. Maturitas 2010; 65: 117-121.
- Norhammar A, Tenerz A, Nilsson G. Glucose metabolism in patients with acute myocardial infarction and no previous diagnosis of diabetes mellitus: a prospective study. Lancet 2002; 359: 2140-2144.
- Marfella R, Di Filippo C, Portoghese M. Tight glycaemic control reduces heart inflammation and remodelling during acute myocardial infarction in hyperglycaemic patients. J Am Col Cardiol 2009; 53: 1425-1436.
- Cruz-Gonzalez I, Chia S, Raffel OC. Hyperglycaemia on admission predicts larger infarct size in patients undergoing percutaneous coronary intervention for acute ST-segment elevation myocardial infarction. Diab res clin pract 2010; 88: 97-102.
- Iliadis F, Kadoglou N, Didangelos T. Insulin and the heart. Diab res clin pract 2011; 93: 86-91.