ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 3
Clinical efficacy of expansive pedicle screw in degenerative scoliosis
Department of Orthopaedics, Chinese PLA General Hospital, Beijing, China
- *Corresponding Author:
- Yan Wang
Department of Orthopaedics
Chinese PLA General Hospital
Beijing 100853, China
Accepted on 29 August 2016
Background: The surgical treatment of adult scoliosis still presents many points of discussion.
Methods: This study involved a total number of 21 DS patients (4 males and 17 females). All patients required long-segment pedicle screw fixation due to the coronal plane or sagittal plane balance. Postoperative follow-up and evaluation were performed. The balance of coronal and sagittal planes was improved compared with the situation before surgery in 21 patients. A total number of 252 EPS screws were inserted, and 5 screws were removed 3 times during the surgery. There were three screws located on the concave side of the apical vertebrae and two screws located in the lower thoracic spine. All screws were held in place 1 year after surgery without loosening, pull-out, and fracture of rods.
Results: No screw loss occurred during 1-year follow-up, with no statistically significant differences over time (P<0.05). Satisfactory efficacy was also achieved after decompression for those combined with lumbar spinal stenosis.
Conclusion: EPS is effective for correcting DS with good orthopedic outcome and clinical efficacy, although evaluation of the pull-out strength during surgery is required.
Keywords
Pedicle screw, Degenerative scoliosis, Fixation, Surgery.
Introduction
Since China has become an aging society, the incidence of degenerative scoliosis (DS) is on the rise. DS needs to be distinguished from adult scoliosis as it is a result of progressive degeneration of structural spinal elements leading to spinal column malalignment, whereas adult scoliosis is a collective term (inclusive of degenerative scoliosis) comprising of all spinal deformities in a skeletally mature individual [1-3]. The incidence of scoliosis in adulthood varies in the literature between 1.4 and 29.4% [4-7]. For many years in the literature available, the possibility that one could develop spinal deformities in adulthood or old age took backstage. In 1969, Vanderpool et al. [8] predicted that osteoporosis and osteomalacia could produce vertebral instability to a degree that may induce the onset of a spinal deformity, which in most cases is manifested primarily at the lumbar level. This possibility was confirmed in subsequent studies [3,9-12], which concluded that scoliosis could appear de novo in adults with degenerative etiology and in most cases was responsible for worsening low back pain [13]. Many DS patients have co-existing osteoporosis (OP) of varying degrees, which is one of the reasons for the occurrence and progression of DS in the elderly population [14-16]. For DS patients who require surgical treatment, the binding capacity and stability of the pedicle screw are major concerns. Indeed, Professor Cook and Lei Wei [17,18] had designed an expansive pedicle screw (EPS) to improve the binding capacity and stability. However, their studies were limited because of not emphasizing the use and efficacy of EPS in DS patients undergoing long segment fixation. This study presents 21 DS cases treated by EPS retrospectively.
Materials and Methods
General information
A total number of 21 DS patients (4 males and 17 females) with an average age of 58 years from September 2012 to September 2013 were involved in this study. All cases presented with imbalance in the torso and mechanical lower back pain due to DS, with or without lumbar spinal stenosis (radicular pain, neurogenic intermittent claudication, and neurogenic lower back pain).
Surgical protocol
All patients required long-segment pedicle screw fixation due to the coronal plane or sagittal plane balance. Decompression of responsible segments and lumbar fusion were needed for patients complicated by lumbar spinal stenosis. Proximal fusion was performed above the superior vertebra in scoliosis patients in the coronal plane or at the level of neutral vertebra. The segments to be operated on spanned over the thoracolumbar kyphosis in the sagittal plane. In order to the post-operative degeneration, the anterior vertebrae were placed at T10 under the condition that X-ray imaging showed that the vertical trabeculae were sparse or indistinct. Distal fusion was performed at L5 or S1 depending on inter-body space by magnetic resonance imaging (MRI). To ensure and improve the quality of life, pedicle screw was fixed at L5 as L5/S1 disc was functioning well without any instability or spondyloschisis. If the L5/S1 disc was damaged and X-ray imaging revealed sparse and indistinct vertical trabeculae, iliac screw fixation was necessary.
EPS screws (Shandong Weigao Group, Shandong, China) were used and inserted conventionally. Lumbar fusion was performed if good imaging findings were obtained. For patients with imbalance, posterior release was done first. The real purpose was to ensure a satisfactory orthopedic surgery outcome instead of restore lumbar lordosis or correct the Cobb angle completely.
Post-operative follow-up and evaluation
Frontal and lateral radiographs of the entire spine were obtained in the standing position before and after lumbar fusion. The following parameters were measured: Cobb angle; central sacral vertical line distance (deviation of C7 from the vertical line of the midline of the sacrum [C7-CSVL]); lumbar lordosis (angle between the superior endplate of L1 and endplate of S1 [LL]); pelvic tilt (PT); sacral slope (angle between the plane of the sacral endplate and the horizontal line [SS]), pelvic incidence (the angle between line passing from the midpoint of sacral endplate and line connecting the midpoint of the sacral endplate and the midpoint of the bilateral femoral heads [PI]); sagittal vertical axis (from C7 to superior posterior edge of sacrum [SVA]). T-tests were used to compare parameters in each means before fusion, immediately after fusion as well as 1 year after fusion. Besides this, VAS scores for lower back and leg pain, and Oswestry disability index (ODI) scores were also collected. SPSS17.0 software was used to perform all statistical analysis in this study.
Results
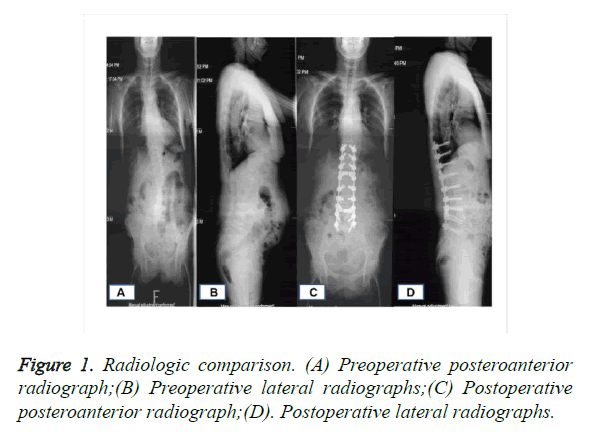
The balance of coronal and sagittal planes was improved compared with the situation before surgery in 21 patients (Figure 1). A total number of 252 EPS screws were inserted, and 5 screws were removed 3 times during the surgery. There were three screws located on the concave side of the apical vertebrae and two screws located in the lower thoracic spine. All screws were held in place 1 year after surgery without loosening, pull-out, and fracture of rods.
It turns out that all cases had satisfactory orthopedic outcomes and compared with situation before surgery, the imbalance in the sagittal and coronal planes was improved. No screw loss occurred during 1-year follow-up, with no statistically significant differences over time (P<0.05). There was no significant difference between the situation immediately after surgery and 1 year after surgery (P>0.05; Table 1). Satisfactory efficacy was also achieved after decompression for those combined with lumbar spinal stenosis. Table 2 showed that there were significant differences in VAS and ODI scores before surgery and 1 year after surgery (P<0.05).
| Before surgery | After surgery | 1 year after surgery | |
|---|---|---|---|
| Cobb | 28.3 ± 11.4 | 16.2 ± 9.9 | 16.6 ± 8.4 |
| C7-CSVL | 3.3 ± 2.3 | 1.9 ± 1.8 | 1.1 ± 2.2 |
| LL | 24.6 ± 15.3 | 38.1 ± 11.3 | 35.1 ± 10.5 |
| PT | 27.7 ± 12.8 | 17.6 ± 14.4 | 18.6 ± 13.8 |
| SS | 23.5 ± 14.2 | 34.1 ± 12.9 | 32.3 ± 11.5 |
| PI | 51.4 ± 14.6 | 52.3 ± 11.6 | 51.8 ± 13.3 |
| SVA | 15.1 ± 7.5 | 8.5 ± 5.5 | 9.8 ± 7.5 |
Table 1. Imaging parameters before and after lumbar fusion.
| Pre-operation 1-year-followed-up | P | ||
|---|---|---|---|
| ODI | 35.3 ± 6.4 | 17.6 ± 7.3 | <0.05 |
| Lumbago of VAS |
6.2 ± 2.2 | 3.8 ± 1.5 | <0.05 |
| Skelalgia of VAS |
5.3 ± 2.7 | 3.3 ± 2.3 | <0.05 |
Table 2. Quality of life scores before and after lumbar fusion.
Discussion
DS occurs after skeletal maturation, typically in the lumbar spine and involving short segments [19,20]. DS is associated with vertebral rotation, slippage, and sagittal plane imbalance, and may present the following symptoms: lumbar spinal stenosis (radicular pain, neurogenic intermittent claudication, and neurogenic lower back pain); and imbalance in the torso and mechanical lower back pain [21-23]. Surgical intervention was in needed for patients with conservative therapy which proves to be ineffective [6,24-26].
Treatment strategies were varied according to the different symptoms. Silva and Lenke proposed six levels of treatment for DS based on clinical presentations and imaging findings, which were usually referred to as the Lenke-Silva classification [27]. It provided reliable basis for selecting the segments for fixation and fusion, as follows: level I, simple posterior lumbar decompression without fusion; level II, posterior lumbar decompression+posterior short segment fixation and fusion; level III, posterior lumbar decompression+posterior long segment fixation and fusion; level IV, posterior lumbar decompression+anterior and posterior fixation and fusion; level V, posterior lumber fixation and fusion with extension to the thoracic segment; and level VI, posterior lumbar decompression+osteotomy+posterior fixation and fusion. Decompression of the affected intervertebral space with fixation and lumbar fusion was preferred for simple spinal stenosis without imbalance in the torso or mechanical lower back pain due to DS. If imbalance in the torso or mechanical lower back pain was present, orthopedic procedures with fixation and lumbar fusion would be necessary for the deformed position. What’s more, the decompression of intervertebral space was performed for patients with lumbar spinal stenosis. Because all of our patients underwent long segment fusion and required orthopedic procedures, the treatment protocol belongs to the second category.
During the 1-year follow-up period after orthopedic treatment, the QoL scores (ODI and VAS) were greatly increased and the balance in the sagittal and coronal planes was partially restored. DS patients do not require complete restoration of balance as in adolescent idiopathic scoliosis for two reasons: lordosis must be reconstructed firstly in order to restore the lumbar curve completely , which may lead to coronal plane imbalance and junction kyphosis in the sagittal plane; and second, most DS patients are combined with osteoporosis (OP) with high stiffness. Inappropriate orthopedic efforts could lead to the pull-out of screws during surgery and failure of internal fixation. In this study, all screws were located in positions bearing large stress. The screws were used for correcting scoliosis in the apical vertebra region in coronal plane and kyphosis of the thoracolumbar segment in sagittal plane. It should be emphasized that orthopedic treatment of DS in the sagittal plane is more important. According to the literature, the imbalance of sagittal plane is the major reason for the pain mechanical of lower back [10,11]. Among our cases, LL was restored to 38° from the previous 24.6° with a PT of 51° after treatment. Considering the risk of proximal junction kyphosis, even though sagittal plane balance was greatly improved, LL was not completely restored. Since DS patients had low compensatory ability, complete restoration might lead to coronal plane imbalance, and therefore the Cobb angle was restored to 16.2° from the previous 28.3°. C7-CSVL, as a measure of coronal plane balance, was restored to 1.9 cm from the previous 3.3 cm, and finally to 1.1 cm during the 1-year follow-up period.
DS is usually concurrent with OP. It has been reported by Pappou et al. [28] that the incidence of DS was 91.7% in the patients with OP. Thus, DS may be regarded as a clinical indicator of OP. Among the 48 patients with DS reported by Bridwell et al. [29], the incidence of OP was 38%. It has been reported that 36% of OP patients had co-existing DS, and DS was mostly caused by the compression fracture of OP patients [30]. In order to reduce the failure of intra-operatively internal fixation, all patients were treated with an EPS in this study. Unfortunately, pull-out occurred 3 times, probably due to the design of the EPS itself. The front of the EPS will not expand as it is pressed into a rod until the nut is tightened. Therefore, the binding capacity of the screw will not improve during surgery, but after surgery when the nut is tightened.
Conclusion
EPS is effective for correcting DS with good orthopedic outcome and clinical efficacy, although evaluation of the pull-out strength during surgery is required.
References
- Kanter AS, Asthagiri AR, Shaffrey CI. Aging spine: challenges and emerging techniques. Clin Neurosurg 2007; 54: 10-18.
- Anasetti F, Galbusera F, Aziz HN, Bellini CM, Addis A. Spine stability after implantation of an interspinous device: an in vitro and finite element biomechanical study. J Neurosurg Spine 2010; 13: 568-575.
- Benner B, Ehni G. Degenerative lumbar scoliosis. Spine 1979; 4: 548-552.
- Aebi M. The adult scoliosis. Eur Spine J 2005; 14: 925-948.
- Kostuik JP, Bentivoglio J. The incidence of low-back pain in adult scoliosis. Spine 1981; 6: 268-273.
- Xu L, Sun X, Huang S, Zhu Z, Qiao J. Degenerative lumbar scoliosis in Chinese Han population: prevalence and relationship to age, gender, bone mineral density, and body mass index. Eur Spine J 2013; 22: 1326-1331.
- Jiang CJ, Yang YJ, Zhou JP, Yao SQ, Yang K. Applications of the scoliosis width-to-length ratio for guiding selection of the surgical approaches of degenerative lumbar scoliosis. BMC Musculoskelet Disord 2016; 17: 48.
- Vanderpool DW, James JI, Wynne-Davies R. Scoliosis in the elderly. J Bone Joint Surg Am 1969; 51: 446-455.
- Yamada K, Nakamae T, Shimbo T, Kanazawa T, Okuda T. Targeted Therapy for Low Back Pain in Elderly Degenerative Lumbar Scoliosis: A Cohort Study 2016; 41: 872-879.
- Du J, Tang X, Li N, Zhang L, Zhang X. Limited long-segment fusion for degenerative lower lumbar scoliosis: a special kind of scoliosis. Int Orthop 2016; 40: 1227-1231.
- Wang H, Ma L, Yang DL, Ding WY, Shen Y. Radiological analysis of degenerative lumbar scoliosis in relation to pelvic incidence. Int J Clin Exp Med 2015; 8: 22345-22351.
- Zheng J, Yang Y, Lou S, Zhang D, Liao S. Construction and validation of a three-dimensional finite element model of degenerative scoliosis. J Orthop Surg Res 2015; 10: 189.
- Briard JL, Jegou D, Cauchoix J. Adult lumbar scoliosis. Spine 1979; 4: 526-532.
- Pappou IP, Girardi FP, Sandhu HS, Parvataneni HK, Cammisa FP. Discordantly high spinal bone mineral density values in patients with adult lumbar scoliosis. Spine 2006; 31: 1614-1620.
- Yagi M, King AB, Boachie-Adjei O. Characterization of osteopenia/osteoporosis in adult scoliosis: does bone density affect surgical outcome? Spine 2011; 36: 1652-1657.
- Seo JY, Ha KY, Hwang TH, Kim KW, Kim YH. Risk of progression of degenerative lumbar scoliosis. J Neurosurg Spine 2011; 15: 558-566.
- Cook SD, Salkeld SL, Whitecloud TS, Barbera J. Biomechanical evaluation and preliminary clinical experience with an expansive pedicle screw design. J Spinal Disord 2000; 13: 230-236.
- Lei W, Wu Z. Biomechanical evaluation of an expansive pedicle screw in calf vertebrae. Eur Spine J 2006; 15: 321-326.
- Kaspiris A, Grivas TB, Weiss HR, Turnbull D. Surgical and conservative treatment of patients with congenital scoliosis: alpha search for long-term results. Scoliosis 2011; 6: 12.
- Palmisani M, Dema E, Cervellati S. Surgical treatment of adult degenerative scoliosis. Eur Spine J 2013; 22: S829-833.
- Trobisch P, Suess O, Schwab F. Idiopathic scoliosis. Dtsch Arztebl Int 2010; 107: 875-884.
- Ouellet J, Odent T. Animal models for scoliosis research: state of the art, current concepts and future perspective applications. Eur Spine J 2013; 22: S81-95.
- Hong JY, Suh SW, Modi HN, Hur CY, Song HR. Reliability analysis for radiographic measures of lumbar lordosis in adult scoliosis: a case-control study comparing 6 methods. Eur Spine J 2010; 19: 1551-1557.
- Ploumis A, Transfledt EE, Denis F. Degenerative lumbar scoliosis associated with spinal stenosis. Spine J 2007; 7: 428-436.
- Cho KJ, Kim YT, Shin SH, Suk SI. Surgical treatment of adult degenerative scoliosis. Asian Spine J 2014; 8: 371-381.
- Fujimori T, Iwasaki M, Nagamoto Y, Sakaura H, Oshima K. The utility of superficial abdominal reflex in the initial diagnosis of scoliosis: a retrospective review of clinical characteristics of scoliosis with syringomyelia. Scoliosis 2010; 5: 17.
- Silva FE, Lenke LG. Adult degenerative scoliosis: evaluation and management. Neurosurg Focus 2010; 28: E1.
- Pappou IP, Papadopoulos EC, Swanson AN, Cammisa FP. Jr., Girardi FP. Osteoporotic vertebral fractures and collapse with intravertebral vacuum sign (Kummel's disease). Orthopedics 2008; 31: 61-66.
- Bridwell KH. Degenerative scoliosis. In: The textbook of spinal surgery. Philadelphia, JB Lippincott, 1997, 728-741.
- Vanderpool DW JJ, Wynne-Davies R. Scoliosis in the elderly. J Bone Joint Surg Am 1969; 51: 446-455.