ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2006) Volume 17, Issue 1
Attitudes, perception and practice of workers in laboratories in the two colleges of Medicine and their teaching hospitals in Lagos State, Nigeria as regards universal precaution measures
M.C Izegbu, O. O. Amole*, G.O. Ajayi
Departments of Morbid Anatomy, Pharmacology, +Medical Biochemistry, Lagos State University College of Medicine, Ikeja, PMB 21266, Lagos, Nigeria.
- *Corresponding Author:
- O.O Amole
Department of Pharmacology
Lagos State University College of Medicine Ikeja,
Lagos, Nigeria
Accepted date: December 12, 2005
Objective of the present study is to determine the knowledge, attitude, and practice of universal precautions amongst medical laboratory workers in the two Colleges of Medicine and their Teaching hospitals in Lagos State, Nigeria. Cross-sectional study of health care workers was Conducted using a standardized self-administered questionnaire, which enquired about knowledge, attitude and practices of universal precautions. The hepatitis B vaccination statuses were also determined. 300 questionnaires were administered and 154 of them were returned giving a response rate of 51.3%. Participants included; Medical laboratory scientist 55.8%(n=86), Laboratory at-tendants 23.3%(n=36), Medical laboratory technician 10.4%(n=16), Post-graduate students 7.8%(n=12) and Medical doctors 2.59%(n=4). All the participants wear gloves during laboratory work but 81.2% wear a single pair. Ny-lon gloves were commonly used (57%) followed by latex gloves (43%). 17.5 % of the partici-pants claimed to know what to do if exposed to infection. (i) 45.6% of the participants eat in the laboratory, (ii) 47.0% of them store foods and water in the refrigerators meant for stor-age of body fluids and chemicals, (iii) 31.5% of them put on cosmetics in the laboratory, (iv) 12.6% smoke and sniff in the laboratory, (v) 10.0% cut their finger nails with teeth and put their biros in their mouths in the laboratory. (vi) 36.5% do not know that tissues fixed in formalin can transmit infections. (vii) 91.5% are not immunized against hepatitis B virus (HBV). (viii) 99.0% of them do not take shower immediately after laboratory work. (ix) 82.0% of the participants do not feel that the use of masks is necessary in laboratory. It is concluded that the knowledge, attitude, perception, and compliance with universal pre-cautions amongst these highly exposed laboratory workers are poor.
Keywords
Universal precautions, Laboratory workers, Hepatitis B vaccinations, sharp injuries
Introduction
The workers in laboratories in Colleges of Medicine and Teaching hospitals generally are faced with many hazards at work and his/her health and safety may be severely jeopardized if adequate preventive protective measures are not taken. These hazards can be physical, chemical, blood-borne (cross) infections and even legal actions. The prevention of occupational hazards in laboratories requires a thorough knowledge of the risks and practical measures to be taken [1]. Laboratory and other health care workers should familiarize themselves with “universal precautions,” as defined by Center for Disease Control, are a set of precautions designed to prevent transmission of Human immunodeficiency virus (HIV), hepatitis B virus (HBV), and other bloodborne pathogens when providing first aid or health care. Under universal precautions, blood and certain body fluids of all patients are considered potentially infectious for HIV, HBV and other blood borne pathogens [2].
Universal precautions apply to blood, other body fluids containing visible blood, semen, and vaginal secretions. Universal precautions also apply to tissues and to the following fluids: cerebrospinal, synovial, pleural, peritoneal, pericardial, and amniotic fluids. Universal precautions do not apply to faeces, nasal secretions, sputum, sweat, tears, urine, and vomitus unless they contain visible blood. Uni-versal precautions do not apply to saliva except when visibly contaminated with blood or in the dental setting where blood contamination of saliva is predictable.
Universal precautions involve the use of protective barriers such as gloves, gowns, aprons, masks, or protective eyewear, which can reduce the risk of the health care worker’s skin or mucous membranes to potentially infective materials. In addition, it is recommended that all health care workers take precautions to prevent injuries caused by needles, scalpels, and other sharp instruments or devices.
Laboratory workers are exposed to a large pool of specimens from patients suffering from infections such as HBV and HIV [3,4]. However, they seem to have a poor perception of the risk of infections and are not compliant with the basic principles of universal precautions [5,6]. This system of infection control is, therefore, very important if the risk of transmission of infections in the laboratory is to be minimized, as they may not be aware of the outcome of blood and fluid specimens until they are investigated or contaminated instruments in the laboratory.
The purpose of this study was therefore to assess the knowledge about and compliance with universal precautions amongst laboratory workers in the College of Medicine of the University of Lagos and its Teaching hospital as well as Lagos State University College of Medicine and its Teaching Hospital all situated in Lagos State, Nigeria.
Materials and Methods
Background
This cross-sectional study of health care workers was conducted at the Colleges of Medicine and Teaching Hospitals in Lagos between March and April 2005.
Participants
Only health care workers who were directly involved with the work in the laboratories of these institutions participa-ted in the study. 300 questionnaires were randomly sent out, which were to be filled and returned. Only 154 questionnaires were returned.
Survey instrument
A structured self-administered questionnaire developed by adapting guidelines on universal precautions was used to collect data for the study [1]. It was pretested amongst laboratory staff at Olabisi Onabanjo University Teaching Hospital. Information sought included sociodemographic characteristics such as age, sex, marital status, cadre of the participants, duration of working experience and background on biohazards.
Participants were scored on some items using biosafety attitudinal scale. These items included (a) eating in the laboratory, (b) storage of food and water in the refrigera-tor meant for body fluids, drugs, chemicals or other specimens, (c) application of cosmetics, (d) smoking or sniffing, cutting of fingernails with teeth or putting the biro in the mouth, (e) wearing of hand gloves (f) putting on of laboratory coats, (g) transmission of infection by tissues fixed in formalin, (h) immunization against hepatitis B virus, (i) washing of hands after removal of hand gloves, (j) participation in periodic tuberculosis skin testing, (k) taking of shower immediately after participating in laboratory work, (l) wearing of gloves ,(m) impervious gown or (n) apron with full sleeve coverage during au-topsy procedures or embalmment.
A participant scores no mark when he or she is not sure, 1 mark when strongly disagree, 2 marks when disagree, 3 marks when agree and 4 marks strongly agree. Participants were deemed to have good attitudes if they scored 3 or 4 marks in ten of the fourteen selected items.
Participants were also scored on some items on biohazards and biosafety competence scale. These items included wearing and putting on of face masks, aprons or gowns, gloves, surgical scrub suit and its cap, developing safety management programme profile, participation in mandatory safety information training, understand routes of exposure to infection associated with laboratory work and knowledge of procedure when there are accidental splashes or spillage.
A participant is scored 1 mark when he or she does not practice the stated safety measures and 5 marks when he or she does.
Participants were deemed compliant if they scored 5 marks in at least five of the eight selected items. Furthermore, participant’s knowledge on the subject was sought by inquiring what they would do if they sustained injuries in the laboratory.
The Hepatitis B vaccination statuses were also determined.
Data analysis
All returned questionnaires were analyzed in a computer using Epi-Info version 6.04 b software (CDC, USA, and WHO, Geneva, Switzerland).
Both descriptive and inferential statistics were computed. The level of significance was set at p<0.05.
There were no written standing order procedures (SOP) regarding universal precaution procedures in the laborato-ries.
Results
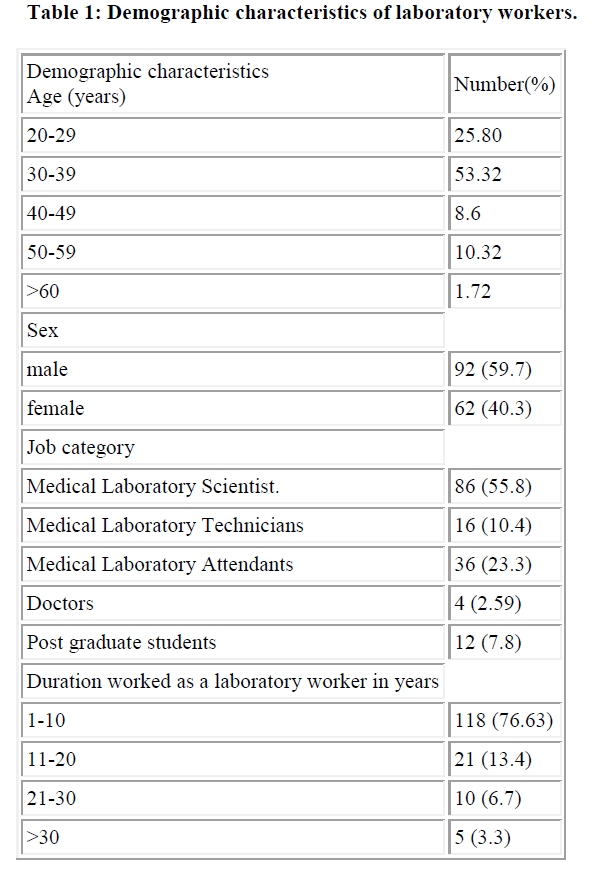
300 questionnaires were sent out and 154 of them were returned giving a response rate of 51.3%. 92 males and 62 females participated with an m: f=1.5. 73% of them claimed to be married while 27% are single. 82% of them proclaimed to be Christians while 18% were Muslims.
The mean age was 36.8±6.5 with a working experience of 8.3±2.1 years. 76.63%of the participants had worked for less than10 years.
Results shows that the category of the staff that partici-pated included, Medical laboratory scientist 55.8%(n=86), Laboratory attendants 23.3% (n=36), Medical laboratory technician 10.4%(n=16), Post-graduate students 7.8% (n=12) and Medical doctors 2.59% (n=4).
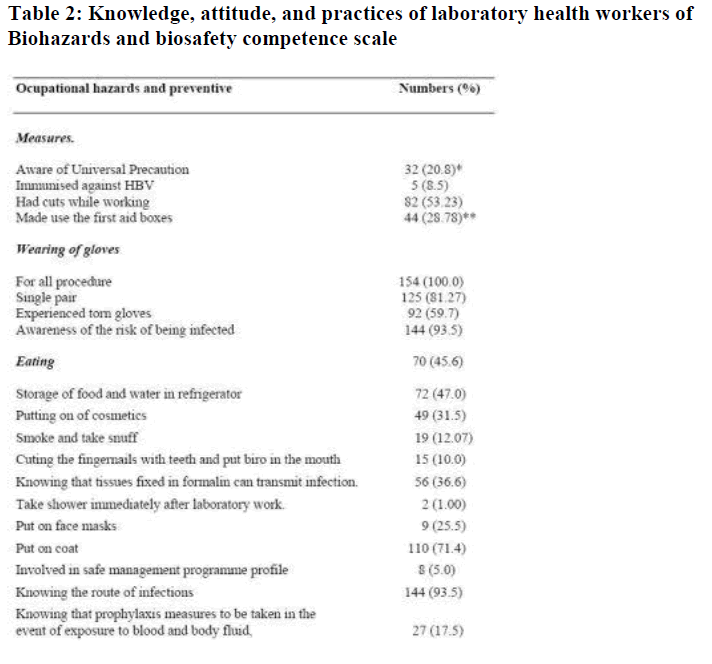
Regarding awareness about Universal Precautions, Table 2 shows that 20.8% (n=32) of the participants had heard of it and only 37.5% (n=12) of these could define and state it’s objectives
Background on biohazards
53.23% (n=82) of the participants had had cuts or punc-tures from needles, surgical blades, sharp instruments or devices and were treated in the laboratories. This study shows that 94% of the laboratories have first aid boxes and of these, only 28.78% of the victims make use of these boxes
All the participants wear gloves during laboratory works but 81.2% wear a single pair. Nylon gloves were most commonly used (57%) followed by latex gloves (43%).
Of these, 59.7% had experienced torn gloves and claimed that they are changed as soon as they are noticed.
93.5% of the participants were aware of the risk of being infected and they could only recognize HBV and HIV as potential workplace exposures. They do not know if the following diseases could be contacted at workplace: Shigellosis, Tuberculosis,Creutzfeld-Jacob disease, Small pox, Lassa fever, Brucellosis as indicated in their response.Creutzfeld-Jacob disease, Small pox, Lassa fever, Brucellosis as indicated in their response.
11.69% claimed to have been infected but the nature of the infection was not stated.
17.5 percentage of the participants claimed to know what to do if exposed to infection
Biosafety attitudinal scale
This scale shows that (i) 45.6% of the participants ate in the laboratory, (ii) 47.0% of them store foods and water in the refrigerators meant for storage of body fluids and chemicals, (iii) 31.5% of them put on cosmetics in the laboratory, (iv) 12.6% of smoke and sniff in the laboratory, (v) 10.0% cut their finger nails with teeth and put their biros in their mouths in the laboratory, (vi) 36.5% do not know that tissues fixed formalin can transmit infections, (vii) 91.5% of are not immunized against HBV, (viii)
99.0% of them do not take shower immediately after laboratory work, (ix) 82.0% of the participants do not feel that face masks are necessary in laboratory.
Results show that (i) 25.2% of the participants do not wear or put on face masks, (ii) 28.6% does not put on laboratory coats, (iii) 4.2% do not wash their hands after the removal of the gloves, (iv) 28.8% do not wear surgical scrub suites and it’s cap, (v) 95.0% had not been involved in developing safe management programme profile, (vi) 96.5% had never been involved in safety information training, (vii) 6.5% do not know the route of infection in the laboratory and (viii) 83.5% do not have the knowledge of procedure when there are accidental splashes and spillage of infectious materials.
Discussion
The level of awareness about universal precautions amongst laboratory workers is rather low as only 20.8% of them had heard about the term and only 37.5% of these could correctly state the objectives.
The attitude and practices of the laboratory health workers towards universal Precaution call for a lot of concern as 45.6% of them ate in the laboratory and this is compara-ble with 41.0% rate observed amongst laboratory scientist in Ibadan, Nigeria [7] and greater than 5.6% amongst workers in Lagos State Emergency Services (LASEMS) in Lagos [8]. 47.0% of them store foods, water and drinks in the refrigerators meant for storage of body fluids and chemicals, 31.5% of them put on cosmetics in the laboratory, 12.6% of them smoke and sniff in the labora-tory, 5.3% cut their finger nails with teeth and put their biros in their mouths in the laboratories, 28.6% do not put on laboratory coats, 4.2% do not wash their hands after the removal of the gloves, 36.5% do not know that tissues fixed formalin can transmit infections. Furthermore, 91.6% of them are not immunized against HBV, 99.0% of them do not take shower immediately after laboratory work. These have to change if these workers are to be protected from been infected and making the work places safe. Glove use amongst the study populations appears to be satisfactory. All the participants wear gloves during laboratory works and nylon gloves were most commonly used (67%) followed by latex gloves (33%). This observation is in agreement with the claims of other workers (8). It is very interesting to note that 81.2% wear a single pair and of these, 59.7% had experienced torn gloves, which are changed as soon as they are noticed. None of those who had sustained injuries reported it to the hospital authorities because they felt no positive actions would be taken and could be treated elsewhere (8). 53.23 % of them were treated in laboratory out of which 28.78% of them made use of the first aid boxes. The reasons proffered for the under utilization of the first aid boxes are that they are mere window dressings and as such they are ill equipped, poorly managed and kept in the laboratories in fulfillment of the requirements of the accrediting bodies.
The ultimate responsibility for laboratory safety within an institution lies with its Chief executive officer, who, along with all immediate associates should have a continuing, overt, commitment to the safety program. This commitment, as well as tangible support, should be obvious to all. A potentially effective safety program that is ignored by top management will fail because others will certainly ignore it. It has been shown that perception of senior management support for safety programmers was the most significant factor influencing compliance with infection control and reducing exposure incidents [8,9,10]. We observed that 17.5% of them were knowledgeable about post exposure prophylaxis, which is comparable with 8.0% as obtained amongst British surgeons [11] and 10.0% as recorded at LASEMS in Lagos [8]. It has been reported that health workers are generally not aware of what form of prophylaxis measures to be taken in the event of exposure to blood and body fluids [8]. Many needle and sharp injuries can be avoided but, in the event of a needle prick or sharp injury, the following steps should be taken (i) immediately wash the wound in tap water and non-mucosal surfaces with soap, (ii) record the accident, (iii) have hepatitis B immune globulin and active immunization if not already vaccinated HBV. Vaccination at 0,2, and 6 weeks (accelerated vaccination) may be effec-tive; the efficacy of immune globulin has not been estab-lished, (iv) have a booster of vaccine against HBV if already immunized but more than 3 years before, (v) if HIV is likely to be involved, expert counseling of the wounded person and the patient is required. The patient on whom the instrument has been used should be tested for HIV and the person wounded should also be tested at 3 and 6 months for HIV antibody [1].
The incidence of infection with HBV has declined in health care workers in recent years largely due to the widespread immunization with hepatitis B vaccine [12]. In many health facilities, even though the personnel are vaccinated, the seroconversion status after vaccination is not assessed [13]. The CDC recommendation is to test for antibody after completion of three injections of HBV vaccine, and if negative, give a second three-dose vaccine and test again anti-HBsAg antibodies. If there is no antibody response, no further vaccination is recommended. If an employee has a blood exposure to a patient known or suspected to be at high risk of HbsAg sero-positivity, he should be given HBIGx2 (one month apart) or HBIG and initiate revaccination [14]. In this study, 13 participants (8.4%) claimed to have been vaccinated against hepatitis B virus and the seroconversion statuses were not stated which is comparable to the reports of other workers [8,10]. This puts the greater percentage of the participants at risk if they were seronegative and this call for mass immunization for laboratory workers.
In conclusion, knowledge and compliance with universal precautions among these highly exposed laboratory workers is poor [8,9,15]. Suggestions to improve deficiencies identified include elaborate training on universal precaution commitment to safety safer work practices by hospital management. Vaccination of staff against hepatitis B should also be done while guidelines for post prophylaxis should be widely disseminated.
Acknowledgement
We are sincerely grateful to all the participants both in College of Medicine of University of Lagos/Lagos Uni-versity Teaching Hospital, Idi-Araba and Lagos State University College of Medicine/ Lagos State University Teaching Hospital, Ikeja for sparing their time to fill the questionnaires.
The authors sourced for funds for this project and therefore not indebted to any body
References
- Ogunbodede EO. Occupational hazard and safety in dental practice. Nig. J. Med. 1996; 5: 11-13
- Johnson and Johnson Medical Inc Blood-borne infection. A practical guide to OSHA compliance Arlington. Johnson and Johnson Medical Inc.1992.
- Nwabuisi C. Olatunji P.O. Prevalence of Hepatitis B surface antigen amongst tertiary health workers in Ilorin. Nig. Qrt.J.Hosp.Med.1999; 9: 95-97.
- Falope I A, Adedeji O.O, Eyesan S U; Incidence of HIV positivity in trauma victims over the age of 20years.The Niger postgraduate Med.J.1998; 5: 115-117.
- Adebamowo C. A, Ajuwon A. The immuization status and level of knowledge about Hepatitis B virus infection among Nigerian surgeons. West Afr.J.Med.1997; 16:93-1696.
- Brusaferro S. Martina P. Puzzolante L; Epidemiological study on knowledge, attitudes and behaviour of health care workers with respect to HIV infection. Med. Lav. 1997: 88: 495-506.
- Omokhodion F. O. Health and safety in clinical laboratory practice in Ibadan, Nigeria Afr.J.Med.Sci.1998: 27: 201-204.
- Odusanya O.O. Awareness and compliance with Universal Precautions amongst health workers at an emergency medical service in Lagos, Nigeria, Niger Med J, Vol. 44, No.1, January-February, 2003.
- Lunding S, Nielsen T.L., Nielsen J.O [Poor compliance with universal precautions among Danish physicians] Ugeskr Laeger 1998: 160:1789-1793.
- Nat’AcademiesPress, Biosafety in the Laboratory: Prudent Practices for Handling and Disposal of infectious Materials 1989, pg 1-8.
- Duff S E, Wong CKM, May RE. Surgeons and occupational health department’s awareness of guidelines on post-exposure prophylaxis for staff exposed to HIV: telephone survey, BMJ 1999:319: 162-163.
- Poole C.J.M, Miller S, Fillingham G. Immunity to hepatitis B among health care workers performing exposure-procedures. BMJ 1994; 309; 94-95.
- Barone P, Scicca A, Lupo F, Leonardi S, Murumeci S. Hepatitis vaccination in young nurses of a general hospital. Ann lg 1995; 7: 251-255.
- Centers for Disease Control and Prevention. Recommendation for post-exposure prophylaxis (PEP) for exposure to HBV, HCV and HIV. MMWR 2001; 50: 22.
- Willy M E, Dhillon G L, Loewer N L; Adverse exposures and universal precautions practice among a group of highly exposed health professionals. Infec. Control Hosp. Epidemiol 1990:11:351-356.