ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2015) Volume 26, Issue 2
Association of fatty pancreas and diabetes. A Case Control Study from Kathmandu Valley.
Department of Biochemistry, Nepalese Army Institute of Health Sciences, Kathmandu, Nepal.
- *Corresponding Author:
- Satrudhan Prasad Gupta
Department of Biochemistry,
Nepalese Army Institute of Health Sciences
Kathmandu, Nepal.
Accepted date: February 04 2015
Objective of the present study is to determine the association of fatty pancreas and diabetes in Nepal. It is a hospital-based study carried out using data retrieved from the register maintained in the Kathmandu Valley Hospital between 1st December, 2012 and 31st May, 2013. The variables collected were age, gender, HbA1c, serum creatinine, fasting blood glucose. The fatty pancreas still remained positively associated with diabetes (OR, 1.344; 95% CI, 1.074–1.682) and prediabetes (OR, 1.132 95% CI, 0.960 – 1.337) in all the subjects. Similarly, triglycerides levels remained positively associated with diabetes (OR, 1.586; 95% CI, 1.269 – 1.981) and prediabetes (OR, 1.379;95% CI, 1.179 – 1.612) in all the subjects. The fatty pancreas is an important associated factor for newly diagnosed diabetes independent of age, gender, adiposity, and other cardiometabolic risk factors in Nepali population.
Keywords
Fatty pancreas, diabetes, HbA1c, creatinine, fasting blood glucose
Introduction
The functional state of the pancreas has a substantial share in the progress of hyperinsulinemia, insulin resistance, impaired glucose tolerance and, equally, the prevailing metabolic changes (obesity, atherogenic dyslipidemia), which contribute to the violation of the endocrine and exocrine pancreatic function [1]. Obesity leads to fat infiltration of multiple organs including the heart, kidneys, and liver. Under conditions of oxidative stress, fatderived cytokines are released locally and resulted in an inflammatory process and organ dysfunction. In the liver, fat infiltration has been termed nonalcoholic fatty liver disease, which may lead to nonalcoholic steatohepatitis [2]. No data are, however, available on the influence of obesity on pancreatic fat, cytokines, and nonalcoholic fatty pancreas disease (NAFPD). Fatty infiltration of the pancreas has been shown to interfere with insulin secretion. Both insulin sensitivity and secretion are important in the pathogenesis of diabetes and pre-diabetic states. Fatty pancreas may promote the development of chronic pancreatitis pancreatic cancer and exacerbate the severity of acute pancreatitis. Moreover, fatty pancreas facilitates the dissemination and lethality of pancreatic cancer, and the formation of pancreatic fistula after pancreatic surgery. There is also independent role of fatty pancreas in impaired glucose metabolism. The excess accumulation of lipids in islets is thought to contribute to the development of diabetes in obesity by impairing beta-cell function [3]. Therefore, we designed a study to determine the association of fatty pancreas and diabetes in Nepal.
Materials and Methods
It was a hospital-based study carried out using data retrieved from the register in the Kathmandu Valley Hospital between 1st December, 2012 and 31st May, 2013. The variables collected were age, gender, HbA1c, serum creatinine, fasting blood glucose. The glycated haemoglobin was determined by ion exchange chromatography [4]. Estimation of serum creatinine was done by Jaffe’s alkaline picrate method [5]. The assessment of fasting blood glucose was done by glucose oxidase and peroxidase method [6]. The transaminases (AST and ALT) were estimated by liquid UV test [7]. Estimation of total cholesterol was done by CHOD-PAP method [8]. All these laboratory parameters were analyzed using human reagent kits and with the help of semi-autoanalyser (Humalyser 3500, Germany). Approval for the study was obtained from the institutional research ethical committee. Analysis was done using descriptive statistics and testing of hypothesis. The data were analyzed using Excel 2003, R 2.8.0, Statistical Package for the Social Sciences (SPSS) for Windows Version 16.0 (SPSS Inc; Chicago, IL, USA) and the EPI Info 3.5.1 Windows Version. The One-way ANOVA was used to examine the statistical significant difference between groups. Post Hoc test LSD was used for the comparison of means of case groups. A p-value of <0.05 (two-tailed) was used to establish statistical significance.
Results
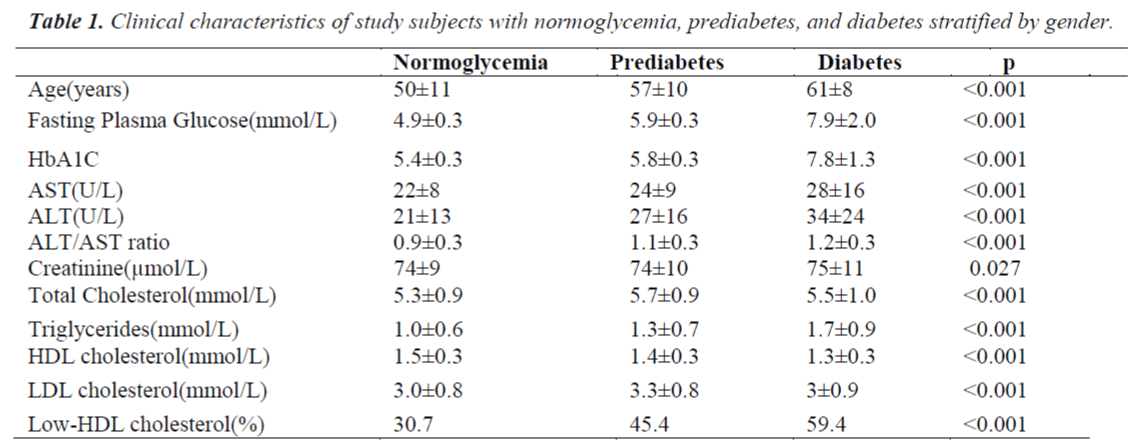
Table 1 shows that fasting plasma glucose levels were raised in cases of pre-diabetic and diabetic patients. Similarly, TG levels were raised in pre-diabetic and diabetic patients.
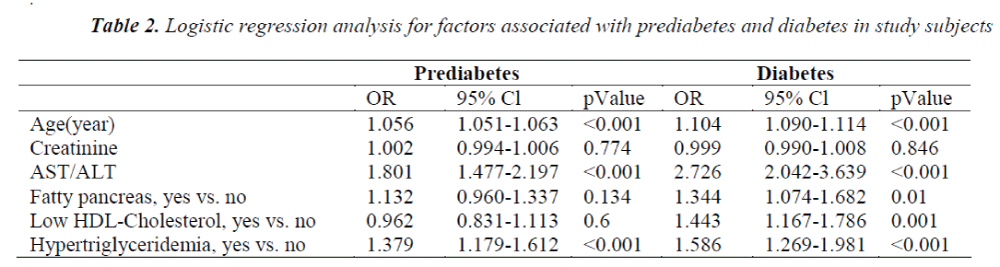
Table 2 depicts the odds ratio of age, which was significantly raised in pre-diabetic and diabetes patients. The fatty pancreas remained positively associated with diabetes (OR, 1.344; 95% CI, 1.074–1.682) and pre-diabetes (OR, 1.132 95% CI, 0.960 – 1.337) in all the subjects. Similarly, triglycerides levels remained positively associated with diabetic (OR, 1.586; 95% CI, 1.269 – 1.981) and pre-diabetic (OR, 1.379;95% CI, 1.179 – 1.612) states.
Discussion
Fatty pancreas is strongly associated with diabetes and pre-diabetic states in both the gender. An association between ectopic fat accumulation in the liver and pancreas has been previously observed in many, but not all, studies [9]. This result implies that in addition to insulin resistance associated with obesity and ectopic fat deposition, such as NAFLD, the impaired β-cell function in fatty pancreas may contribute to the further development of diabetes, as β-cell dysfunction is essential for the development of type-2 diabetes [10]. In our present study, the fatty pancreas still remained positively associated with diabetes (OR, 1.344; 95% CI, 1.074–1.682) and prediabetic states (OR, 1.132 95% CI, 0.960 – 1.337) in all the subjects. Similarly, triglycerides levels remained positive in all the subjects associated with diabetes (OR, 1.586; 95% CI, 1.269 – 1.981) and pre-diabetes (OR, 1.379;95% CI, 1.179 – 1.612).
In addition, once diabetes develops, fatty replacement of damaged tissue may contribute to the extra-islet pancreatic fat deposition. Moreover, the increased levels of malonyl-CoA caused by hyperglycemia in diabetes also inhibit carnitine palmitoyltransferease-1, leading to a de- crease in mitochondrial β-oxidation and further stimulation of intracellular triglyceride accumulation [11]. In conclusion, fatty pancreas is an important associated factor for newly diagnosed diabetes independent of age, gender, adiposity, and other cardiometabolic risk factors in Nepali population.
References
- Wong VW, Wong GL, Yeung DK, et al Fatty pancreas, insulin resistance, and β-cell function: a population study using fat-water magnetic resonance imaging. Am J Gastroenterol 2014; 109: 589-597.
- Lee JS, Kim SH, Jun DW, et al. Clinical implications of fatty pancreas: correlations between fatty pancreas and metabolic syndrome. World J Gastroenterol 2009: 15: 1869-1875.
- Hori M, Takahashi M, Hiraoka N, et al. Association of pancreatic Fatty infiltration with pancreatic ductal adenocarcinoma. Clin Transl Gastroenterol 2014; 5: 53.
- Eckerbom S, Bergqvist Y, Jeppsson JO. Improved method for analysis of glycated haemoglobin by ion exchange chromatography. Ann Clin Biochem 1994; 31: 355-360.
- Peake M, Whiting M. Measurement of serum creatinine--current status and future goals. Clin Biochem Rev 2006; 27: 173-184.
- Trinder P. Determination of blood glucose using 4- amino phenazone as oxygen acceptor. J Clin Pathol 1969; 22: 246.
- Henley KS, Pollard HM. A new method for the determination of glutamic oxalacetic and glutamic pyruvic transaminase in plasma. J Lab Clin Med 1955; 46: 785.
- Trinder P. Determination of serum cholesterol by enzymatic colorimetric method. Ann Clin Biochem 1969; 6: 24-27.
- Lim EL, Hollingsworth KG, Aribisala BS, et al. Reversal of type 2 diabetes: normalisation of beta cell function in association with decreased pancreas and liver triacylglycerol. Diabetologia 2011; 54: 2506-2514.
- Gastaldelli A. Role of beta-cell dysfunction, ectopic fat accumulation and insulin resistance in the pathogenesis of type 2 diabetes mellitus. Diabetes Res Clin Pract 2011; 93: S60-65.
- Zhang D, Liu ZX, Choi CS, et al. Mitochondrial dysfunction due to long-chain Acyl-CoA dehydrogenase deficiency causes hepatic steatosis and hepatic insulin resistance. Proc Natl Acad Sci USA 2007; 104: 17075- 17080.