ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 4
Anthropometrically determined abdominal obesity among nurses in Vhembe and Capricorn Districts, Limpopo, South Africa.
1Department of Nursing Sciences, University of Fort Hare, East London, South Africa
2Department of Advanced Nursing, University of Venda, Thohoyandou, South Africa
3Department of Public Health, University of Venda, Thohoyandou, South Africa
4Department of Nursing Science University of Limpopo, Turfloop Campus, South Africa
- *Corresponding Author:
- Goon DT
Department of Nursing Sciences
University of Fort Hare, East London, South Africa
Accepted date: August 28 2014
Anecdotal evidence concerning the prevalence of abdominal obesity (AO) among nurses in South Africa is alarming; however, no scientific study has confirmed this notion. The purpose of this study was to determine AO, using proxy measures of waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) among nurses in Vhembe and Capricorn districts, Limpopo, South Africa. The study involved a purposive sample of 153 practising nurses aged 19 to 50+ years. Height, weight, waist and hip circumferences were measured and participation in physical activity was assessed by report. Cut-off points for abdominal obesity were: WC= ≥102 cm (men) and ≥88 cm (women); WHR = ≥0.9 (men) and ≥0.8 (women) and WHtR= ≥0.5. The prevalence of AO was 68.2%, 80.5%, 56.5% according to WC, WHR and WHtR, respectively. Among the males nurses, AO were: WC (18.8%), WHR (37.0%), and WHtR (%) while corresponding figures for females nurses were WC (49.4%), WHR (43.5%), WHtR (0.0%). Female nurses had significantly ( X 2 =2.2 03, p = 0.003) higher prevalence of AO compared to the male nurses. The prevalence of AO (WHR, WHtR) increased with age, peaking at ages 40-49 for both sexes, while WC measured obesity showed a similar pattern but peaks at age 50+ among the male nurses. Majority of the nurses decline participating in physical activity. There is high prevalence of AO among nurses in this region, a rate comparable to the general population in South Africa. Future studies identifying risk factors for prevalence of AO in nurses are warranted.
Keywords
Abdominal obesity, anthropometric indices, nurses, South Africa
Introduction
One of the metabolic health outcomes included in the metabolic syndrome [1] is abdominal obesity (AO); fat stored around the abdomen and waist. AO is associated with mortality [2,3], morbidity [4], increased disability [5], poor quality of life [6,7] and increased health care costs [8-10]. Therefore, it is important to identify and treat early, individuals with AO in order to plan appropriate remedial strategies for their health. Thus studying fat distribution is of concern from both an epidemiological and clinical viewpoint [11]. Clinically, fat patterning is supported by numerous epidemiological studies confirming its deleterious effect on cardiovascular risk and morbidity and mortality [3,12-15], and thought to be a better precursor of weight-related and many other types of chronic diseases than total body fat [16].
Direct measurement of AO can be performed by computed tomography, magnetic resonance imaging. However, the use of such “gold standard” methods, has limited applicability when screening larger sample sizes, especially in developing countries like South Africa, largely because they are expensive, unavailable and timeconsuming [11]. In its place, indirect anthropometric measures of waist circumference (WC), waist-to-hip ratio (WHR) and waist-to-height ratio (WHtR) are often used to screen for central fat pattern. These anthropometric measures are known to be associated with cardiovascular and metabolic risk factors [17,18].
The prevalence of AO varies significantly across the world [19] and perhaps among sub-groups of populations. As such, designing appropriate health plans and preventive measures requires gathering the necessary information on AO from different areas [20]. However, to our knowledge, there is no study assessing AO involving nurses in South Africa. Given the health cost implications of chronic diseases such as hypertension, diabetes mellitus and cancer associated with obesity, the findings of the present study will facilitate the development of a preventative strategy for these health care problems. The aim of this study was to examine the prevalence of AO in nurses aged 19-50+ years using different anthropometric indices of WC, WHR and WHtR.
Methods
Participants
This cross-sectional study was carried out on 153 nurses from Vhembe and Capricorn districts in Limpopo province, South Africa. Participants were purposively selected to participate in the study. All nurses practising in Vhembe (rural) and Capricorn (semi-rural) districts were eligible to participate in the study. Exclusion criteria for participation were age below 19 years, Participants who were pregnant (for females), ill, and inability to walk unassisted. Information concerning age, sex and physical activity participation were collected by self-report.
Informed consent was obtained from each participating nurse. The managers of individual hospitals gave permission for the study. Data collection took place in October-November 2011. The study was conducted in accordance with the Declaration of Helsinki for human studies of the World Medical Association [21].
Anthropometry measurements
Stature and body mass were determined according to the standard anthropometric methods of the International Society for the Advancement of Kinanthropometry (ISAK) [22]. Stature was measured to the nearest 0.1 centimeters (cm) in bare feet with participants standing upright against a wall-mounted stadiometer. Body mass was measured to the nearest 0.5 kilogramme (kg) with participants lightly dressed (underwear and T-shirt) using a portal digital scale (Tanita HD 309, Creative Health Products, MI, USA). WC was measured at the level of the narrowest point between the lower costal (10th rib) border and the iliac crest. If there was no obvious narrowing then the measurement was taken at the mid-point between those two landmarks.
The measurement was taken at the end of a normal exhalation with the arms relaxed at the sides (with a required accuracy of one millimetre). The hip circumference was measured at the maximal circumference of the buttock with a steel tape to the nearest 0.1 cm. Circumferences were measured with the cross-hand technique, with the tape at right angles to the body and the readings were done on the right hand side. Only one field worker took the measurements to ensure uniformity and to avoid intervariation in circumference measurements.
Defining abdominal obesity
Abdominal obesity was determined using WHO criteria [23]. WC cut-off was based on WHO action levels. Action level II (substantially increased risk for metabolic syndrome) WC ≥102 cm for men and ≥88 cm for women was used. The diagnostic criteria for WHR were WHR ≥1.0 in men and≥0.85 in women [23,24]. Concerning WHtR, the cut off value of ≥ 0.5 indicates AO [25].
Statistical analysis
Descriptive statistics (percentages, means and standard deviations) were applied to the data. Comparison of proportions was performed with Chi-square tests. All analyses were conducted using the Statistical Package for the Social Sciences (SPSS) version 20.0.
Results
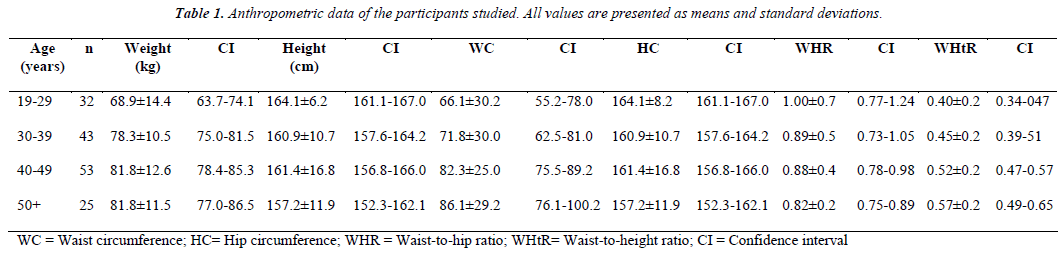
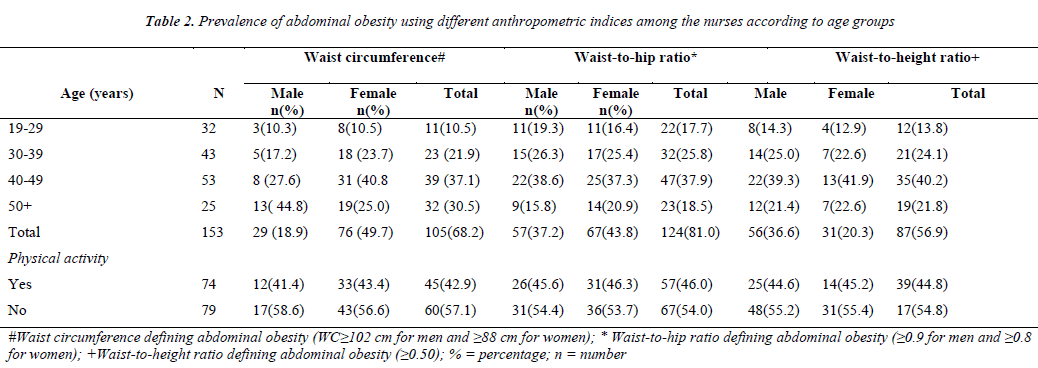
The physical characteristics of the participants are shown in Table 1. The mean (± SD) age of the participants was 39.3 ± 10.7 kg years. Their mean (± SD) weight, height, WC, HC, WHR and WHtR were 78.1 ± 23.1 kg, 156.4 ± 6.0 cm, 0.77 ± 0.3 cm, 0.95 ± 0.3 cm, 0.89 ± 0.2 and 0.49 ± 0.1, respectively. Shown in Table 2, is the prevalence of AO among the nurses stratified by age groups. The prevalence of AO was 68.2%, 80.5%, 56.5% according to WC, WHR and WHtR, respectively. Among the males’ nurses, AO were: WC (18.8%), WHR (37.0%), and WHtR (%) while corresponding figures for female’s nurses were WC (49.4%), WHR (43.5%), WHtR (0.0%).
Female nurses had significantly (X2 = 2.203, p = 0.003) higher prevalence of AO (WC and WHR) compared to the male nurses, while the male nurses had significantly (X2 = 1.924, p = 0.002) higher WHtR ≥ 0.5 compared to female nurses. The prevalence of AO (WHR, WHtR) increased with age, peaking at ages 40- 49 for both sexes, while WC measured obesity showed a similar pattern but peaks at age 50+ among the male nurses. Concerning physical activity participation, majority 79(51.3%) declined participating in physical activity.
Discussion
The present study is to our knowledge the first to evaluate the prevalence of AO among nurses in South Africa. Central fat distribution is a significant factor which can indicate predisposition to cardiovascular and metabolic diseases [26,27]. In order to evaluate potential health risks at an early stage, information on fat distribution is necessary even in individuals with normal weight [28]. The WC, WHR and WHtR as proxy anthropometric indices of abdominal fat distribution can be useful for evaluating the risk incidence of cardiovascular and metabolic diseases [18].
The findings of this study, in the analysed regions, indicate a high prevalence of AO (68.2%, 81.8%, 56.9% for WC, WHR and WHtR, respectively) (Table 2) among the nurses. Comparison of AO among nurses in South Africa is fraught with difficulty as scant data exist. Therefore, the prevalence of AO in this group of population can only be compared to the general South African population. Our finding is similar in scale to the Demographic and Health Survey [29] conducted twelve years ago involving a sample of 13,089 South Africans, which found AO in 51.4% of the participants. Using the WC 80 cm in women, 94 cm in men (30) AO was 63.4% among South African adults. In Turkey, Oguz et al. [31] reported AO to be 13.8% among healthcare workers including nurses. Differences in defining AO, genetic factors, age, type of diet and extent of physical activity might contribute to variations comparable to those found in this study. Nevertheless, the high prevalence rate observed in our sample, being nurses is surprising and might predisposes them to risks of hypertension, diabetes mellitus, cardiovascular disease and stroke. It is expected that nurses with the requisite education are equipped to promote health, in this case, teach about the health implications of excessive weight gain and fat deposit. However, the scenario been witnessed in this present study tend to indicate that this supposedly group of health care providers might end up been health care receivers. Again, if these healthcare providers do not respond to obesity interventions, it may be unrealistic to expect the general public to do so [32]. As strange as this might appears, it is possible some of these nurses may be ignorant of the possible consequences of central fat accumulation. However, this supposition is only speculative. Therefore, a study examining the perception and knowledge of the nurses concerning central fat deposition is warranted.
The present study demonstrated that AO increased with age, peaked between 40-49 years. Other studies [33,34] have reported similar findings that AO is more common among individuals older than 40 years. In a crosssectional study among the Luo, Maasai and Kamba, in rural and urban Kenya, among 1430 individuals (58.3% females), aged 17-68 years, AO increased with age [35].
Generally, AO was higher in female nurses compared to the male nurses. Of course, this is an expected finding, as differences in AO have been reported across genders [36-38]. The gendered nature of AO has been previously reported among USA [39] and Turkish [40], adults. Puoane et al. [29] study among South African adults reported higher prevalence of AO in women (42.0%) compared to men (9.2%). Similarly, a recent study in South Africa [41] indicated higher AO in women than men, as measured by WC and WHR.
Several underlying factors may contribute to AO found in the nursing population in the present study. AO is positively associated with daily energy intake, percentage of energy from fats and sugar intakes [40]. It should be observed that the major staple foods in this region such as ‘pap’ and rice are rich in carbohydrate. It may be possible that energy input among the nurses in our study may be actually higher than the energy expenditure and this positive energy balance would likely result to high fat accumulation. This is attested to by the data collected concerning physical activity, which indicated that majority (51.3%) of the nurses, did not participate in any physical activity (Table 2). In a study, regarding the association between measures and determinants of obesity in African women, Kruger et al. [42] found that physical inactivity demonstrated the strongest association with measures of obesity.
Several limitations of the study should be noted. The direct methods of assessing AO such as computed tomography or magnetic resonance imaging would have provided an objective and better information on the intraabdominal adipose tissue (IAAT) of the nurses. However, this was not feasible due to cost, time and the relatively larger samples involved. Also, the inclusion of only two districts limits the generalisation of the results to all practising nurses in Limpopo Province or South Africa. As such, one should be cautious in interpreting the findings of the study. Notwithstanding the fact that our study did not clearly demonstrate predisposing factors (diet and other lifestyles characteristics, levels of physical activity, cortisol measurements) for AO, it did however; provide baseline data on central body fatness among nurses in a rarely research population group in a semi-urban South African setting.
Conclusion
The study documented higher prevalence of AO among nurses. Given that AO is associated with adverse health outcomes (43); further study need to evaluate the relationship of various body fat distribution indices to adverse biochemical variables as well as the possible correlates of AO among nurses. Judging from a public health perspective, such information could be useful in formulating urgent intervention strategies in order to stem the health risks of AO among the South African nurses in these regions.
Acknowledgements
The authors are grateful to all the nurses who participated in the study and the hospital mangers who allowed for the study to be carried out in their hospitals.
References
- Esteghamati A, Morteza A, Khalilzadeh O, Noshad S, Novin L, Nakhjavani M. Association of serum cortisol levels with parameters of metabolic syndrome in men and women. Clin Invest Med 2004; 34(3): E131-E137.
- Cameron AJ, Magliano DJ, Shaw JE, Zimmet PZ, Carstensen B, et al (2012). The influence of hip circumference on the relationship between abdominal obesity and mortality. Int J Epidemiol, 41: 484-494.
- Whitlock G, Lewington S, Sherliker P, Clarke R, Emberson J, et al (2009). Body mass index and causespecific mortality in 900 000 adults: collaborative analyses of 57 prospective studies. Lancet, 373: 1083-1096.
- Grimble RF (2010). The true cost of in-patient obesity impact of obesity on inflammatory stress and morbidity. Proc Nutr Soc, 69: 511-517.
- Averett SL (2011). Labour market consequences: employment, wages, disability and absenteeism. In J Crawley (Ed). The Oxford handbook of the social science of obesity. New York: Oxford University Press.
- Bentley TG, Palta M, Paulsen AJ, Cherepanov D, Dunham NC, et al (2011). Race and gender associations between obesity and nine health-related quality-of-life measures. Qual life Res, 20: 665-674.
- Perez M, Warren CS (2012). The relationship between quality of life, binge-eating disorder, and obesity status in an ethnically diverse sample. Obesity, 20: 879-885.
- Finkelstein E, Yang H (2011). Obesity and medical costs. In J Crawley (Ed). The Oxford handbook of the social science of obesity. New York: Oxford University Press.
- Moriarty JP, Branda ME, Olsen KD, Shah ND, Borah BJ, et al (2012). The effects of incremental costs of smoking and obesity on health care costs among adults: a 7-year longitudinal study. J Occup Environ Med, 54: 286-291.
- Cawley J, Meyerhoefer C (2012). The medical care costs of obesity: an instrumental variables approach. J Health Econ, 31: 219-230.
- Goon DT, Toriola AL, Shaw BS, Amusa LO (2011). Centripetal fat patterning in South African children. Pak J Med Sci, 7(4): 832-6.
- Manolopoulos KN, Karpe F, Frayn KN (2010) Gluteofemoral body fat as a determinant of metabolic health. Int J Obes, 34: 949-959.
- Conoy D, Boekholdt SM, Wareham N, Luben R, Welch A, Bingham S, et al (2007). Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation into Cancer and Nutrition in Norfolk cohort: A population-based prospective study. Circulation, 116:2933-2943.
- PischonT, Boeing H, Hoffmann K (2010). General and abdominal adiposity and risk of death in Europe. N Engl J Med, 359: 2105-2125. Erratum. N Engl J Med, 362: 2433.
- Despres JP (2007). Cardiovascular disease under the influence of excess visceral fat. Crit Pathw Cardiol, 6: 51-59.
- Klein S, Allison DB, Heymsfield SB, Kelley DE, Leibel RL, Nonas C, et al (2007). Waist circumference and cardiometabolic risk: A consensus statement from Shaping America’s Health: Association for Weight Management and Obesity Prevention; NAASO. The Obesity Society: the American Society for Nutrition, and the American Diabetes Association. Am J Clin Nutr, 85: 1197-1202.
- Liu Y, Tong G, Tong W, Lu L, Qin X (2011). Can body mass index, waist circumference, waist-hip ratio and waist-height ratio predict the presence of multiple metabolic risk factors in Chinese subjects? BMC Publ Health, 11:35.
- Skrzypczak M, Szwed A, Pawlinska-Chmara R, Skrzpulec V (2008). Body mass index, waist to hip ratio and waist/height in adult Polish women in relation to their education, place of residence, smoking and alcohol consumption. J Comp Hum Biol, 59: 329-342.
- Balkau B, Deanfield JE, Despres JP, Bassand JP, Fox KA, Smith Jr SC, et al. (2007). International Day for the Evaluation of Abdominal Obesity (IDEA): a study of waist circumference, cardiovascular disease, and diabetes mellitus in 168,000 primary care patients in 63 countries. Circulation, 116: 1942-1951.
- Qui X, Zhang Y, Cai Y, He M, Sun L, Fu J, et al (2013). Prevalence of obesity, abdominal obesity and associated factors in hypertensive adults aged 45-75 years. Clin Nutr, 32: 361-367.
- World Medical Association (2008). Declaration of Helsinki-Ethical Principles for Medical Research Involving Human Subjects. WMJ, 54: 122-125.
- Marfell-Jones M, Olds T, Stew A, Carter L (2006) International standards for anthropometric assessment. Australia: The International Society for the Advancement of Kinanthropometry.
- World Health Organization (WHO). (1998). Obesity:preventing and managing the global epidemic. Report of WHO consultation on obesity, June 5-7 1997. Geneva, Switzerland: WHO.
- Han TS, Van Leer EM, Seldell JC, Leah ME (1995). Waist circumference action levels in the identification of cardiovascular risk factors: Prevalence study in a random sample. Br Med J, 311: 1401-1405
- Ashwell, M (2009). Obesity risk: importance of the waist-to-height ratio. Nurs Standard, 23(41): 49-54.
- Snijder MB, Dekker JM, Visser M, Bouter LM, Stehouwer C, Kostense PJ, et al (2003). Associations of hip and thigh circumferences indepdent of waist circumference with the incidence of type 2 diabetes: the Hoom Study. Am J Clin Nutr, 77: 1192-1197.
- Skrzypczak M, Szwed A, Pawlinska-Chmara R, Skraypulec V (2007). Assessment of the BMI, WHR and W/Ht in pre-and postmenopausal women. Przeglad Anthropol Rev, 70: 3-13.
- Pavlica T, Bozic-krstic V, Rakic R (2010). Body mass index, wasit-to-hip ratio and waist/height in adult population from Backa and Banat-the Reublic of Serbia. Ann Hum Biol, 37(4): 562-573.
- Puoane T, Steyn K, Bradshaw D, Laubsher R, Fourie J, Lambert V, et al (2002). Obesity in South Africa: The South African Demographic and Health Survey. Obes Res, 10(10): 1038-1048.
- Malhota R, Hoyo C, Ostbye T, Huges G, Schwartz D, Tsolekile L, et al (2008). Determiants of obesity in an urban township of South Africa. S Afr J Clin Nutr, 21(4): 316-320.
- Oguz A, Sagun G, Uzunlulu M, Alpasian B, Yoruimaz E, Teliner E, et al (2008). Frequency of abdominal obesity and metabolic syndrome in healthcare workers and their awareness levels about these entities. Arch Turk Soc Cardiol, 36(5): 302-309.
- Miller SK, Alpert PT, Cross CL. Overweight and obesity in nurses, advanced practice nurses, and nurse educators. J Am Acad Nurse Pract, 20:259-265.
- Amole IO, OlaOliorun AD, Odeigah LO, Adesina SA (2011). The prevalence of abdominal obesity and hypertension amongst adults in Ogbomoso, Nigeria. Afr J Prim Health Care Fam Med, 3(1): Art.#188. doi:10.4102/phcfm.v3i1.188
- Sardinha LB, Santos DA, Silva AM, Coelho-e-Silva MJ, Raimundo AM, Moreira H, et al (2012). Prevalence of overweight, obesity, and abdominal obesity in a representative sample of Portuguese adults. Plos One, 7(10): e47883. doi:10.1371/journal.pone.0047883
- Christensen AL, Hansen AW, Larsson MW, Mwangi DL, Kilonzo T, Boit MK, et al (2008). Obesity and regional fat distribution in Kenyan populations: Impact of ethnicity and urbanization. Ann Hum Biol, 35(2): 232-249.
- Flegal KM, Carroll MD, Ogden LC, Curtin LR (2010). Prevalence and trends in obesity among US adults, 1990-2008. JAMA, 13.
- Must A, Whitney-Evans E (2011). The epidemiology of obesity. In J Crawley (Ed). The Oxford handbook of the social science of obesity. New York: Oxford University Press.
- World Health Organization (2009). World Health Statistics. Geneva: World Health Organization.
- Himes C (2011). The demography of obesity. In J Crawley (Ed). The Oxford handbook of the social science of obesity. New York: Oxford University Press.
- Yabanci N, Gocgeldi E, Simsek I, Kilic S (2010). Prevalence of obesity, abdominal obesity and the associated factors among a group of Turkish adults. Pak J Med Sci, 26(1): 21-25.
- Mkhonto SS, Labadarios D, Mabaso MLH (2012). Association of body weight and physical activity with blood pressure in a rural population in the Dikgale village of Limpopo province in South Africa. BMC Res Notes, 5: 118.
- Kruger HS, Venter CS, Vorster HH (2003). Physical inactivity as a risk factor for cardiovascular diseases in communities undergoing the rural to urban transition: the THUSA study. Cardiovasc J South Afr, 14(1): 16-23.
- Yamborisut U, Sakamoto N, Visetchart P, Tontisirin K (2012). Central body fat distribution indices in Thai preschool children. Open J Pediatr, 2: 47-52.