ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 9
Amlodipine/atorvastatin has an effect on vascular function and normal lipid levels
1School of Basic Medical Sciences, Lanzhou University, Lanzhou, Gansu, PR China
2Affiliated Hospital of Gansu University of Chinese Medicine, Lanzhou, Gansu, PR China
3MJR PharmJet GmbH, Uberherrn, Germany
4Lanzhou University Second hospital, Lanzhou, Gansu, PR China
5Key Lab of Prevention and Treatment for Chronic Disease by Traditional Chinese Medicine of Gansu Province, Lanzhou, Gansu, PR China
Accepted on January 24, 2017
Objective: To investigate whether the use of amlodipine/atorvastatin can affect vascular endothelial function as well as blood vessel elasticity and lipid level compared with hypotensor alone.
Method: There were 162 participants selected into domestic compound hypotensive tablets (Group 1), amlodipine tablets (Group 2) and amlodipine/atorvastatin group (Group 3) randomly. After 3 months, 144 participants remained. Each participant’s medical history was collected, and each participant underwent a blood biochemical examination including high-sensitivity C-Reactive Protein (hs-CRP), Flow-Mediated-Dilation (FMD) and Endothelium-Independent Dilatation (EID), and carotid-Femoral Pulse Wave Velocity (c-f PWV) before and after the 3-month follow-up period.
Results: Compared with baseline, the FMD values of all groups improved significantly. Group 3 showed the greatest difference, followed by Groups 2 and 1. In contrast, no difference in EID was noted (P>0.05 in three groups). After treatment, the c-f PWV of Groups 2 and 3 turned to be significantly better (P<0.05), while that of Group 1 did not change. There was no statistical significant difference among three groups. The lipid levels of the participants in Group 3 decreased, while those in Groups 1 and 2 did not change. The hs-CRP levels of Groups 2 and 3 decreased significantly, whereas that of Group 1 did not change.
Conclusions: In conclusion, we found that Amlodipine/atorvastatin combination pills can improve vascular endothelial function as well as vascular elasticity, and down-regulate the level of hs-CRP.
Keywords
Vascular endothelial function, Pulse wave velocity, Amlodipine/atorvastatin.
Introduction
Cardiovascular disease, a major cause of death worldwide, has the following risk factors: hypertension, age, smoking, glucose tolerance, family history of premature cardiovascular events, obesity, high homocysteine level, and dyslipidaemia. Hypertension is the most important factor among which. Framingham risk score showed that, of hypertensive patients, 78% of men and 82% of women have at least one risk factor [1].
Hypertension and dyslipidaemia are the main reasons for endothelial dysfunction and decreasing arterial elasticity. Studies have indicated that the occurrence and development of cardiovascular disease are related to decreased arterial elasticity [2]. The co-existence of hypertension and high cholesterol can accelerate endothelia dysfunction, causing atherosclerotic plaque formation, the main cause of cardiovascular disease [3]. Most experiments have shown that the rate of death can be decreased by the combination of the treatment of hypertension and hyperlipidaemia [4,5]. Therefore, drug and non-drug methods of controlling blood pressure and lipid levels can reduce cardiovascular mortality rates and improve patient quality of life.
Pulse Wave Velocity (PWV) is a sensitive indicator that can evaluate the arterial elasticity in early clinical trials, and carotid-femoral PWV (c-f PWV) in particular is a reliable predictor of cardiovascular events and mortality [6]. Flow- Mediated Dilatation (FMD) is the most common non-invasive method for evaluating endothelial function. Most patients with hypertension also have dyslipidaemia. Evidence-based medicine studies mainly focus on patients with dyslipidaemia and fail to focus on patients with normal lipid levels and one or two cardiovascular risk factors (such as hypertension, age, smoking, glucose tolerance, family history of premature cardiovascular events, obesity, high homocysteine level, and dyslipidaemia mentioned above). Additionally, based on the use of hypotensors and statins, especially amlodipine/ atorvastatin, helps reduce the incidence and mortality rates of cardiovascular disease in patients with hypertension. However, few studies have examined the early atherosclerotic changes caused by amlodipine/atorvastatin in patients with hypertension, in whom endothelial function and arterial elasticity are the two main indexes. Because of the obvious relationship between morning blood pressure and the incidence of cardiovascular disease, controlling morning blood pressure can reduce the incidence of cardiovascular disease. As such, this study investigated whether the combined use of amlodipine/atorvastatin and a hypotensor can affect patients’ vascular endothelial function and blood vessel elasticity compared to use of the hypotensor alone. Here we studied patients with hypertension without hyperlipidaemia but with one or two cardiovascular risk factors.
Materials and Methods
Materials
The 162 participants in this survey were chosen from among inpatients between March and December 2012 who were administered domestic compound hypertensive tablets, amlodipine tablets, or amlodipine/atorvastatin. The patients were 30-75 years of age, did not have hyperlipidaemia, and had one or two cardiovascular risk factors or being treated at baseline. Both genders were included. After 3 months, 144 participants remained: 44 were included in Group 1 (domestic compound hypotensive tablets which are from China and contain 5 potent medicines: reserpine, chlordiazepoxide, hydrochlorothiazide, dihydralazine sulfate, triamterene. 1 tablet once and per day); 48 were in Group 2 (amlodipine tablets 5 mg per day), and 52 were in Group 3 (amlodipine/atorvastatin, 5 mg per day). Patients were diagnosed according to 1999 World Health Organization/International Society of Hypertension criteria, i.e., systolic blood pressure ≥ 140 mmHg and/or diastolic blood pressure ≥ 90 mmHg, which is in accordance with the 2010 Chinese Hypertension Guideline criteria. The lipid levels of the selected participants corresponded to the 2013 European Society of Cardiology/ European Society of Hypertension (ESC/ESH) management guidelines [7]: total cholesterol ≤ 200 mg/dL, Low-Density Lipoprotein Cholesterol (LDL-C) ≤ 120 mg/dL, and Triglycerides (TG) ≤ 150 mg/dL. All participants provided written informed consent. The experiment excludes the patients whose basal blood pressure>180/100 mmHg, or secondary hypertension, or LDL-C>125 mg/dL, or TG>400 mg/dL, or ejection fraction<40%, or the co-existence of other serious diseases.
Methods
Each participant’s medical history was collected, and all patients underwent a blood biochemical examination (including LDL, C (mg/dl), HDL-C (mg/dl), TC (mg/dl), TG (mg/dl), hs-CRP (mg/l)), high-sensitivity C-Reactive Protein (hs-CRP), FMD, and Endothelium-Independent Dilatation (EID) (Sonos 5500 Ultrasonic Color Doppler system; American HP), and c-f PWV using a 1000 arteriosclerosis testing system (Beijing FuTian Electric). All data were processed and analysed by SPSS 20.0 and EXCEL 2007. One-way analysis of variance was used to compare the three groups and the results are expressed as ͞x ± S. Values of P<0.05 were considered statistically significant.
Results
General clinical data
After the 3-month follow-up study, 144 participants remained: 44 in Group 1 (domestic compound hypotensive tablets); 48 in Group 2 (amlodipine tablets), and 52 in Group 3 (amlodipine/ atorvastatin). The basic participant characteristics-including age, gender, body mass index, smoking history, TG, LPL-C, total cholesterol, high-density lipoprotein, and hs-CRP did not differ statistically among the three groups (Table 1).
| G1 | G2 | G3 | P | |
|---|---|---|---|---|
| No. (M/F) | 44 (25/19) | 48 (22/26) | 52 (25/27) | 0.12 |
| Age | 48.84 ± 13.73 | 49.12 ± 12.55 | 48.41 ± 11.16 | 0.32 |
| BMI (kg/m2) | 27.08 ± 2.60 | 25.01 ± 2.72 | 26.28 ± 3.29 | 0.22 |
| Smoking | 4 | 5 | 6 | 0.11 |
| SBP (mmHg) | 155.9 ± 10.6 | 155.2 ± 11.7 | 154.1 ± 10.3 | 0.25 |
| DBP (mmHg) | 97.3 ± 9.6 | 95.9 ± 10.2 | 96.3 ± 8.2 | 0.48 |
| LDL-C (mg/dl) | 113.92 ± 20.73 | 114.77 ± 26.39 | 120.33 ± 25.31 | 0.13 |
| HDL-C (mg/dl) | 45.45 ± 8.44 | 44.98 ± 8.94 | 47.56 ± 9.56 | 0.26 |
| TC (mg/dl) | 184.19 ± 33.17 | 186.08 ± 38.58 | 194.13 ± 36.91 | 0.99 |
| TG (mg/dl) | 138.6 ± 111.32 | 160.3 ± 117.02 | 163.02 ± 90.79 | 0.16 |
| ALT (IU/L) | 18.4 ± 0.5 | 20.3 ± 0.8 | 19.8 ± 0.3 | NS |
| CRE (μmmol/L) | 48.4 ± 6.5 | 46.3 ± 7.8 | 47.3 ± 6.3 | NS |
Table 1. Participants’ general clinical data (͞x ± S).
Vascular endothelial function
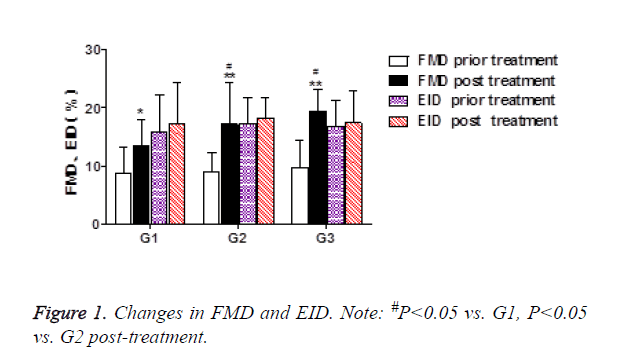
The mean FMD of all groups improved significantly. Group 3 showed the highest degree of improvement, followed by Groups 2 and 1. However, no difference in EID was seen (Table 2 and Figure 1).
| G1 | G2 | G3 | ||||
|---|---|---|---|---|---|---|
| Basline | 3 month | Basline | 3 month | Basline | 3 month | |
| FMD (%) | 8.7 ± 4.6 | 13.4 ± 4.6* | 8.9 ± 3.4 | 16.8 ± 6.2**# | 9.7 ± 4.6 | 19.4 ± 3.7*△ |
| EID (%) | 15.7 ± 6.5 | 17.1 ± 7.3 | 17.2 ± 4.5 | 18.2 ± 3.6 | 16.7 ± 4.5 | 17.4 ± 5.4 |
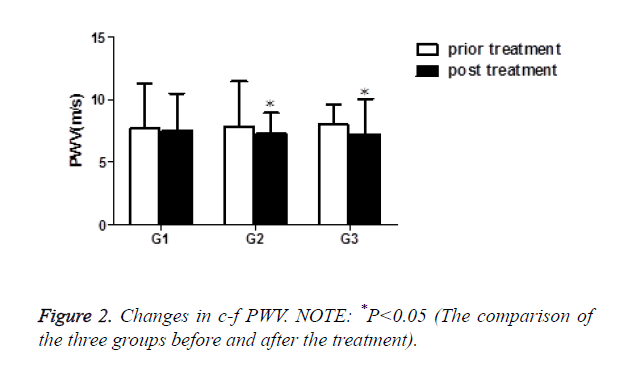
| PWV (m/s) | 7.69 ± 3.59 | 7.53 ± 2.95 | 7.81 ± 3.63 | 7.29 ± 1.63* | 8.58 ± 4.29 | 7.82 ± 2.84* |
| NOTE: *P<0.05, **P<0.01 (The comparison of the three groups before and after the treatment); #P<0.05 vs. G1, △P<0.05 vs. G2 post-treatment | ||||||
Table 2. Changes in vascular function (͞x ± S).
Vascular elasticity
After treatment, the c-f PWV of Groups 2 and 3 were significantly improved, whereas that of Group 1 did not change. There were no statistically significant changes among the three groups (Table 2 and Figure 2).
Lipid and hs-CRP levels
After treatment, the lipid levels of the participants in Group 3 decreased, while those in Groups 1 and 2 did not change. The hs-CRP levels of Groups 2 and 3 also significantly declined, whereas that of Group 1 did not change. The differences in hs- CRP levels in Groups 2 and 3 were statistically different from those in Group 1 but not statistically different from each other (Table 3).
| Groups | LDL-C (mg/dl) | HDL-C (mg/dl) | TC (mg/dl) | TG (mg/dl) | hs-CRP (mg/l) | |
|---|---|---|---|---|---|---|
| G1 | Basline | 113.92 ± 20.73 | 45.45 ± 8.44 | 184.19 ± 33.17 | 138.6 ± 111.32 | 1.44 ± 1.01 |
| 3 month | 113.15 ± 20.55 | 45.1 ± 8.54 | 182.50 ± 32.50 | 135.25 ± 90.24 | 1.42 ± 0.03 | |
| G2 | Basline | 114.77 ± 26.39 | 44.98 ± 8.94 | 186.08 ± 38.58 | 160.3 ± 117.02 | 1.40 ± 0.91 |
| 3 month | 113.27 ± 24.39 | 43.98 ± 9.01 | 184.79 ± 38.41 | 151.52 ± 98.25 | 1.30 ± 0.13*# | |
| G3 | Basline | 120.33 ± 25.31 | 47.56 ± 9.56 | 194.13 ± 36.91 | 163.02 ± 90.79 | 1.43 ± 0.54 |
| 3 month | 105.5 ± 21.14*# | 47.52 ± 9.35 | 177.33 ± 35.2*# | 148.06 ± 75.93*# | 1.32 ± 0.17*# | |
| Note: *P<0.05 (The comparison of the three groups before and after the treatment); #P<0.05 vs. G1 post-treatment. | ||||||
Table 3. Changes in lipid and hs-CRP levels (͞x ± S).
Discussion
The “China Cardiovascular Disease Report 2011” shows that China currently has 230 million patients with cardiovascular disease and that 350 million succumb to it yearly, accounting for 41% of all deaths [6]. As is known to all, the cardiovascular diseases such as hypertension and coronary heart disease share the same physiological and pathological basis-atherosclerosis. In the presence of hypertension, vascular endothelial cells are stimulated by growth factor and vasoactive substances, leading to an increase in the migration of vascular smooth muscle cells and promoting the development of molded fibrous [8,9]. Long-term uncontrolled hypertension is the main cause of cardiovascular disease, particularly when accompanied by genetic factors, environmental factors, and structural abnormalities of blood vessels. Therefore, the treatment for hypertension also focuses on changes in vascular function.
In the clinical setting, there are many measurement methods for vascular function, including PWV, FMD, urinary micro albumin/creatinine, and Nitric Oxide (NO).
The main forms of atherosclerosis are vasoconstriction and endothelium dysfunction, which finally causes the partial or complete close-up of vascular. So for the patients with hypertension, it is crucial to prevent and treat Atherosclerosis. The 2010 ESC/ESH hypertension management guidelines changed the c-f PWV standard from 12 m/s to 10 m/s. Generally speaking, the larger the value, the greater the degree of stiffness. Benetos et al. found the accelerated artery stiffness can be affected by blood pressure, heart rate, and c-f PWV after they had been following up the treated patients with hypertension and the participants with normal blood pressure for 6 years [10].
In addition, Laurent et al. examined 1,715 patients with hypertension for as long as 7.9 years and found that as the c-f PWV increased by 4 m/s, the patients’ relative risk of stroke increased to>1.72 and that after adjustment for cardiovascular risk factors, c-f PWV remained a significant indicator (relative risk=0.39, P<0.02) [11].
Endothelial dysfunction is the contributing factor for atherosclerosis and a common cause of atherosclerosis and hypertension. Atherosclerotic vascular abnormalities, primarily vasoconstriction and endothelial dysfunction, can ultimately lead to partial or complete occlusion of the blood vessels in patients with hypertension, so the prevention and treatment of atherosclerosis are critical. FMD is the most common non-invasive inspection method for evaluating endothelial function, which can predict cardiovascular disease events [12].
The ACTION study [13] found that amlodipine demonstrated some anti-atherosclerotic properties, stimulated NO production, act as an anti-oxidant, and regulate matrix deposition. This study found that after treatment of amlodipine or amlodipine/atorvastatin, vascular function is obviously improved; in contrast, vascular function is not improved by Guo compound antihypertensive drugs, as found in early research. Therefore, vascular function is best improved by amlodipine/atorvastatin treatment. Atorvastatin interferes with the development of atherosclerosis through non-lipid-related and pleiotropic effects, including improved endothelial function, reduced vascular smooth muscle cell proliferation, stabilized athermanous plaques, reduced inflammation, and reduced platelet aggregation [14]. In an open-label study of 21 hypertensive, hypercholesterolemic patients, 3 months of amlodipine treatment improved large and small vessel arterial compliance by 26% and 38%, respectively, and reduced systemic vascular resistance by 10% (all P<0.0001 vs. baseline) [15]. The addition of atorvastatin for an additional 3 months improved small-vessel arterial compliance by an additional 42% (P<0.001 vs. month 3) and reduced systemic vascular resistance by an additional 5% (P<0.05 vs. month 3). In contrast, large-vessel compliance was not further improved by combination therapy. What’s more, Azushima et al. also found the effects of single pill-based combination therapy of amlodipine and atorvastatin on within-visit blood pressure variability and parameters of renal and vascular function in hypertensive patients with chronic kidney disease.
In conclusion, we found that Amlodipine/atorvastatin combination pills can improve vascular endothelial function as well as vascular elasticity, and down-regulate the level of hs- CRP.
References
- Khot UN, Khot MB, Bajzer CT, Sapp SK, Ohman EM. Prevalence of conventional risk factors in patients with coronary heart disease. JAMA 2003; 290: 898-904.
- Vlachopoulos C, Aznaouridis K, Stefanadis C. Prediction of cardiovascular events and all-cause mortality with arterial stiffness-A systematic review and meta-analysis. J Am Coll Cardiol 2010; 55: 1318-1327.
- Mason RP. A rationale for combination therapy in risk factor management: a mechanistic perspective. Am J Med 2005; 118: 54-61.
- Widlansky ME, Gokce N, Keaney JF, Vita JA. The clinical implications of endothelial dysfunction. J Am Coll Cardiol 2003; 42: 1149-1160.
- Corretti MC, Anderson TJ, Benjamin EJ. Guidelines for the ultrasound assessment of endothelial-dependent flow-mediated vasodilation of the brachial artery-A report of the International Brachial Artery Reactivity Task Force. J Am Coll Cardiol 2002; 39: 257-265.
- Laurent S, Cockcroft J, Van Bortel L. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur H J 2006; 27: 2588-2605.
- Mancia G, Fagard R, Narkiewicz K. 2013 ESH/ESC guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). Blood Pres 2013; 22: 193-278.
- OLeary DH, Polak JF, Kronmal RA, Manolio TA, Burke GL. Carotid-artery intima and media thickness as a risk factor for myocardial infarction and stroke in older adults. Cardiovascular Health Study Collaborative Research Group. N Engl J Med 1999; 340: 14-22.
- Blanco-Colio LM, Osende JI, Martín-Ventura JL. Statins in hypertensive patients: potential explanations for the ASCOT-LLA study results. Drugs 2004; 64: 61-67.
- Van BLM, Laurent S, Boutouyrie P. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid-femoral pulse wave velocity. J Hypertens 2012; 30: 445-448.
- Benetos A, Adamopoulos C, Bureau JM. Determinants of accelerated progression of arterial stiffness in normotensive subjects and in treated hypertensive subjects over a 6-year period. Circul 2002; 105: 1202-1207.
- Moens AL, Goovaerts I, Claeys MJ, Vrints CJ. Flow-mediated vasodilation: a diagnostic instrument, or an experimental tool? Chest 2005; 127: 2254-2263.
- Lubsen J, Wagener G, Kirwan BA. Effect of long-acting nifedipine on mortality and cardiovascular morbidity in patients with symptomatic stable angina and hypertension: the ACTION trial. J Hypertens 2005; 23: 641-648.
- Zhou MS, Schulman IH, Jaimes EA. Thiazide diuretics, endothelial function, and vascular oxidative stress. J Hypertens 2008; 26: 494-500.
- Leibovitz E, Beniashvili M, Zimlichman R. Treatment with amlodipine andatorvastatin has additive effect in improvement of arterial compliance in hypertensive hyperlipidemic patients. Am J hypertens 2003; 16: 715-718.
- Azushima K, Uneda K, Tamura K, Wakui H, Ohsawa M. Effects of single pill-based combination therapy of amlodipine and atorvastatin on within-visit blood pressure variability and parameters of renal and vascular function in hypertensive patients with chronic kidney disease. Biomed Res Int 2014; 2014: 437087.