ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 17
Algorithmic approach to upper respiratory tract infections in primary care
1Department of Family Medicine, Eskişehir Osmangazi University, Eskişehir, Turkey
2Yeni Family Health Care Center, Eskişehir, Turkey
3Kemal Nurhan Mani Family Health Care Center, Eskişehir, Turkey
4Yıldıztepe Family Health Care Center, Eskişehir, Turkey
- *Corresponding Author:
- Hüseyin Balcioğlu
Department of Family Medicine
Eskişehir Osmangazi University, Eskişehir, Turkey
Accepted date: August 11, 2017
Introduction: Despite the majority of these infections being viral, a high percentage are regarded as bacterial infection by physicians and treated unnecessarily with antibiotics. We aimed to compare changes in patient-physician behaviors and therapeutic approaches and costs with use of Upper Respiratory Tract Infections (URTI) algorithms in primary care.
Material and Methods: This study is a randomized, controlled clinical field study, which was performed with the participation of 34 volunteer family physicians that were, later, divided into 2 groups as algorithm group and control group, with respect to their family center. Both groups were asked to fill surveys that were designed specifically for each group. Differences in therapeutic approaches and treatment costs were compared for both algorithm using and not using physician’s groups. At the end of the study, participant physicians were asked to answer a 12-question survey to assess their therapeutic approach to URTI.
Results: A total of 460 patients were included to study. When antibiotic prescribing rates were compared between the groups, significantly fewer antibiotics were prescribed in the algorithm group. Modelling experiments for all cases revealed that group itself and presence of a sore throat, cough and fever were effective variables for antibiotic prescribing. Modelling was performed separately to determine how algorithm affects decision making. Prescription fees are significantly higher in the antibiotics using group.
Conclusion: Although there are guidelines in the primary care practice, this behavioural change after a single training suggests that more training are necessary and application of record-based algorithm systems is required.
Keywords
Algorithm, Upper respiratory tract infections (URTI), Antibiotic prescription, Sore throat.
Introduction
Upper Respiratory Tract Infections (URTI), which are defined as diseases characterized by acute nasal and pharyngeal mucosal inflammation in the absence of another respiratory disorder, represent the most common disease evaluated in primary care. Despite great advances in medicine, uncomplicated URTIs continues to be a great burden on society in terms of human suffering, economic losses and millions of days of absence from work or school each year [1]. The incidence is estimated to be 2-3 episodes per year in adults, 6-8 episodes per year in children URTI represents 50% of all adult illnesses and 75% of illnesses in children [2]. URTI are most commonly observed in the spring. The majority of these infections (69-83%) were showed to be viral in origin. The most common viral infectious agents are from rhinovirus family in about 80% of cases. Other viruses include the coronavirus, influenza A or B, parainfluenza virus, adenovirus, enterovirus, and respiratory syncytial virus. In remaining cases, no proven pathogen was identified. Primary bacterial infections are extremely rare. Despite the majority of these infections being viral, a high percentage are regarded as bacterial infection by physicians and treated unnecessarily with antibiotics [3,4].
A study from a large, outpatient ambulatory network of more than 52000 cases of URTI showed that 65% of cases received an antibiotic prescription [5]. Overuse of antibiotics may lead to resistance, increased cost, and increased incidence of adverse effects, including anaphylaxis [6]. To provide an effective, accurate and reliable treatment facility and to guide therapy, some criteria were determined and various algorithms have been developed for specific diseases. For an approach to the management of URTI to be of practical use during routine office visits in primary health care, these algorithms must be simple, be applicable to both children and adults, reduce unnecessary antibiotic prescribing and improve identification of Group A Streptococcus infections which are responsible for only 10-20% of URTI in general practice [7-9]. The centor criteria are a set of criteria which may be used to identify the likelihood of a Streptococcal pharyngitis infection in adult patients, complaining of a sore throat [7]. Points derived from the criteria of presence of fever, tonsillar exudates and tender anterior cervical lymphadenopathy, absence of cough and age of patient were used to guide management of a sore throat in terms of the need for antibiotic prescribing. Patients with a score of 4 or 5 are at high risk of streptococcal pharyngitis, and empiric treatment may be considered [10]. If centor score is zero or 1, streptococcal pharyngitis risk is very low and there is no need for further testing (i.e., the throat culture or Rapid Antigen Detection Testing (RADT)) or antibiotic therapy. A score of 2-3 requires RADT or throat culture to warrant antibiotic therapy with positive results [8]. The presence of all 4 variables shows a 40-60% positive predictive value for a culture of the throat to test positive for Group A Streptococcus bacteria. The absence of all 4 variables shows a negative predictive value of greater than 80% [11]. The high level of negative predictive value suggests that the centor criteria can be more effectively used to rule out than to diagnose strep throat. Evidence-based, constantly updated with current literature and guidelines, self-learning clinical decision support systems and diagnosis/treatment algorithms are needed to provide physicians to follow and apply current information, improve the quality and efficiency of health care, improve clinical outcomes and minimize the risk of medical errors, help increasing quality while decreasing the cost of care. Nowadays, computer-based systems have become one of the required features of the health sector. Improvement of communication and internet connections has enabled widespread use of this technology in the health sector. Creation of clinical practice based computer software has facilitated the implementation of clinical information systems in hospitals [12]. In this study, we aimed to compare changes in patient-physician behaviors and therapeutic approaches and costs with use of URTI algorithms in primary care.
Materials and Methods
This study is a randomized, controlled clinical field study, which was performed with the participation of 34 volunteer family physicians that were, later, divided into 2 groups as algorithm group and control group, with respect to their family center. An information meeting, describing general outline of the study and surveys, and implementation of the study was held for each group separately. To the algorithm group, modified McIsaac diagnostic criteria were described, and to investigate the effectiveness of treatment, participants were told to consider these criteria for management of patients having inclusion criteria. The control group was told to make no change in their own daily diagnostic and treatment protocols. Both groups were asked to fill surveys that were designed specifically for each group. The patient selection criteria were as follows: Age ≥ 18 y, voluntary, literate, having URTI symptoms for less than 3 d and have no previous medical treatment for URTI symptoms. Local ethics committee approval for the study was obtained from the Eskişehir Osmangazi University Clinical Investigations Ethics Committee (80558721/28, No. 09, February 08, 2016). All data were statistically analyzed. This study was performed between February 15, 2016-May 27, 2016. Acute pharyngitis (bacterial and viral) and acute tonsillitis were included under the general heading of Upper Respiratory Infections. Acute otitis media and acute sinusitis were not included. Patients meeting inclusion criteria signed informed consent forms. Then, physicians filled out a questionnaire, prepared by the research group. Patients were invited for control examination 10 d later and a control form was filled. Differences in therapeutic approaches and treatment costs were compared for both algorithm using and not using physician’s groups. At the end of the study, participant physicians were asked to answer a 12- question survey to assess their therapeutic approach to URTI. Information from current drug prices list and active ingredients table were matched to survey data.
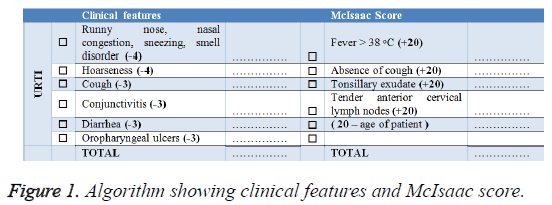
Algorithm: We evaluated centor and McIsaac criteria and to provide a broader perspective we developed a new table by adding clinical symptoms of viral infections. 20 points were given for each finding listed in the McIsaac criteria. An age score was obtained by subtracting patient’s age from 20. In addition, a total of 20 points, the equivalent of 1 criteria for viral symptoms, was added. Physicians of algorithm group were advised to start antibiotic treatment in scores above 60. However, they were free to use any treatment including antibiotics even for scores below 60 (Figure 1).
Statistical analysis
In our study, frequency tables, mean and Standard Deviation (SD) and for comparisons Pearson chi-square, the Fisher exact test, t-test and logistic regression analysis were used.
Results
A total of 460 patients were included to study. Of all cases 64.6% (n=297) were included to Algorithm group and 35.4% (n=163) were included to control group. 37.6% of patients in the study were male (n=173), 62.4% (n=287) were female and the average age was 38.3 y (SD=14.8) (37.4 y (SD=13.8) for females, 39.7 y (SD=16.1) for males). The average educational period of patients was 9.5 y (SD=4.3) (9.2 y (SD=4.4) for females; 10.0 y (SD=4.1) for males). Working status of patients were as full-time in 32% (n=147), part-time in 2% (n=9) and non-working in 66.1% (n=304). The most commonly identified occupational group was housewives. Some features observed in control visits were compared with antibiotic usage among groups (Table 1).
| Group | Compliance with treatment | Continuation of the complaint | Admitting to another physician | Start antibiotic on its own | |||||
|---|---|---|---|---|---|---|---|---|---|
| Yes | No | Yes | No | Yes | No | Yes | No | ||
| Algorithm | 60>Antibiotic treatment initiated | 11 | 0 | 0 | 11 | 0 | 11 | 0 | 11 |
| 60<Antibiotic treatment initiated | 12 | 0 | 2 | 10 | 1 | 11 | 0 | 12 | |
| 60<Antibiotic treatment is not initiated | 266 | 8 | 38 | 236 | 13 | 261 | 6 | 268 | |
| Control | Antibiotic treatment initiated | 63 | 2 | 11 | 54 | 2 | 63 | 2 | 63 |
| Antibiotic treatment is not initiated | 97 | 1 | 21 | 77 | 2 | 96 | 1 | 97 | |
| Total | 449 | 11 | 72 | 388 | 18 | 442 | 9 | 451 | |
Table 1
There was no significant difference both in terms of criteria scores and between groups. When antibiotic prescribing rates were compared between the groups, significantly fewer antibiotics were prescribed in the algorithm group (Table 2).
| Antibiotics use | Group | |||
|---|---|---|---|---|
| Algorithm | Control | Total | ||
| Yes | Count | 23 | 65 | 88 |
| % | 0.077 | 0.399 | 0.191 | |
| No | Count | 274 | 98 | 372 |
| % | 0.923 | 0.601 | 0.809 | |
| Total | Count | 297 | 163 | 460 |
| % | 1 | 1 | 1 | |
Table 2: Antibiotics use in groups.
Antibiotic prescribing rates in algorithm group patients with body temperature levels below 38°C were found lower than that of the control group. Although antibiotics were prescribed to all patients of control group having body temperature levels above 38°C, antibiotics were not prescribed to some patients in algorithm group (Table 3).
| Group | Temperature measurement | Total | |||
|---|---|---|---|---|---|
| 38+ | 38- | ||||
| Algorithma | Antibiotic | Given | 16 | 4 | 20 |
| Not given | 8 | 162 | 170 | ||
| Total | 24 | 166 | 190 | ||
| Controlb | Antibiotic | Given | 10 | 35 | 45 |
| Not given | 0 | 64 | 64 | ||
| Total | 10 | 99 | 109 | ||
| Totalc | Antibiotic | Given | 26 | 39 | 65 |
| Not given | 8 | 226 | 234 | ||
| Total | 34 | 265 | 299 | ||
Table 3: Comparison of antibiotic prescribing and baseline temperature measurements.
While there was a significant inverse relationship between the presence of a cough and antibiotic prescribing in algorithm group, no such relation was observed in control group. High body temperature was more likely to affect antibiotic prescribing in algorithm group. While a sore throat was significantly affecting antibiotic prescribing in control group, no such relation was observed in the algorithm group. In control visits performed 10 d after initiation of treatment, 97.6% of cases (n=449) were compliant with treatment and 84.3% (n=388) were reported relieved symptoms. There was no significant difference between compliance to treatment and antibiotic prescribing with antibiotic prescribing and case groups.
Patient behaviors in URTI
Among patients, only 2.4% (n=11) performed body temperature measurement at home. Post-treatment body temperature measurement rates did not change. 3.9% of cases (n=18) admitted to a different physician. There was no significant difference between groups for admitting to a different physician (chi-square p=232). At 10th d visits 5.4% of cases (n=25) used drugs other than recommended. Half of these drugs were antibiotics (n=12), and almost 1/3 of people who recommended these drugs were not doctors (n=7). Of cases 18.9%, mostly female patients (chi-square p=0.032), used alternative treatments. Variables like education level, marital status and high fever did not affect the use of alternative treatments. There was no difference between groups in terms of using alternative treatments. Alternative treatment using rates were found higher in cases with persisting symptoms (chi-square p=0.001). These alternative treatments were composed of herbal teas, especially linden.
Physician behaviors in URTI
To the second survey, 31 physicians were participated. The average age of physicians is 41.8 (SD=4.8), 48.4% were male (n=15), 51.6% were female (n=16). Among participants 77.4% (n=24) were married, 12.9% (n=4) were single and 9.7% (n=3) were divorced; 54.8% (n=17) were graduated from Osmangazi University. 29% (n=9) were specialist doctors, the mean duration of medical practice was 16.3 y (SD=4.8), average duration of primary care practice was 13.0 (SD=6.7) y. Average number of patients examined per y was 9890 (SD=2046). Ranking of URTI symptoms are shown in Table 4.
| Symptom | 1st line | 2nd line | 3rd line | 4th line | 5th line | Total | % study |
|---|---|---|---|---|---|---|---|
| Nasal Discharge | 24 | 24 | 24.1 | ||||
| Sore throat | 6 | 22 | 1 | 29 | 48 | ||
| Cough | 5 | 17 | 1 | 1 | 24 | 27 | |
| Fever | 3 | 3 | 8 | 14 | 8.3 | ||
| Stuffiness | 1 | 2 | 4 | 12 | 19 | 9.1 |
Table 4: URTI symptom ranking of patients.
The symptoms observed by the physicians and derived by the study were consistent. Top 3 antibiotics preferred by physicians were shown in Table 5.
| Antibiotic | 1st choice | 2nd choice | 3rd choice | Total |
|---|---|---|---|---|
| Amoxicillin and clavulanic Acid | 22 | 4 | 2 | 28 |
| Oral penicillin | 3 | 11 | 2 | 16 |
| Parenteral penicillin | 2 | 2 | 1 | 5 |
| Cephalosporin | 9 | 9 | 18 | |
| Ampicillin sulbactam | 8 | 8 |
Table 5: The first 3 ranks of antibiotic preferences of the participating physicians.
The most commonly preferred supportive treatments were antiinfluenza combinations (n=26), followed by analgesics and antipyretics (n=20), and oral rinse/spray (n=17). Only one physician recommended herbal tea as an alternative treatment. The most commonly reported URTI symptoms were nasal congestion (n=30), sneezing (n=26), cough (n=25), serous nasal discharge (n=23) and headache (n=14). Injectable preparations were preferred in 1.6% of all patients. In all groups, preferred drug forms for an average prescription were 1.60 (n=662) tablet/capsule, 0.43 (n=179) syrup, 0.15 (n=66) gargle and 0.45 (n=186) spray form. Each prescription contained an average of 2.8 drugs. Due to the use of combination drugs, containing more than one active ingredient, the number of active ingredients per prescription was found as 5.87. The number of drugs and active ingredients per prescription was 2.59 drugs and 5.50 active ingredients for algorithm group; 3.10 drugs and 6.43 active ingredients for the control group. The most commonly prescribed agents are shown in Table 6. The average recipe price for the entire study was 19.9 TL (SD=14.6). The average of prescription costs was found significantly lower in the algorithm group. Algorithm groups average prescription cost is 15.4 TL and control groups average prescription cost is 26.9 TL.
| Active ingredient | Count | % | |
|---|---|---|---|
| 1. | Paracetamol | 295 | 71 |
| 2. | Pseudoephedrine HCL | 242 | 58 |
| 3. | Chlorpheniramine Maleate | 144 | 34 |
| 4. | Benzydamine HCL | 143 | 34 |
| 5. | Ibuprofen | 121 | 29 |
| 6. | Chlorhexidine Gluconate | 116 | 28 |
| 7. | Phenylephrine HCL | 83 | 20 |
| 8. | Dextromethorphan HBR | 79 | 19 |
| 9. | Butamirate Citrate | 55 | 13 |
| 10. | Acetylcysteine | 51 | 12 |
| 11. | Levodropropizine | 48 | 11 |
| 12. | Amoxicillin-Clavulanic Acid | 42 | 10 |
| 13. | Caffeine | 38 | 9 |
| 14. | Flurbiprofen | 36 | 8 |
| 15. | Iopamidol HCL | 33 | 7 |
| 16. | Acetylsalicylic Acida | 29 | 7 |
| 17. | Vitamin Cb | 19 | 4 |
| 18. | Cefuroxime Axetilc | 9 | 2 |
| 19. | Cefdinirc | 7 | 1 |
Table 6: Sorting of the active ingredients in the patient's prescriptions.
Discussion
Because of its viral origin, the absence of specific treatment beyond the control of symptoms, and a small number of patients that will benefit from antibiotic treatment, URTI has been emerging as an issue to focus on evidence-based management and rational drug use in primary care practice [13]. While we were planning this study, we intended to distribute physicians equally to groups. However, because of unequal numbers of physicians working in family medicine health care centers, and to prevent interaction between physicians in health care center, equal numbers of physicians in algorithm and control group could not be achieved. Also, because of the limited period of study, the numbers of patients followed by each physician were not equal. The number of participants was also affected by changing number of patients admitting for control visits, taking drugs which were not recommended a by physician however that could change patient’s clinic presentation. These patients were excluded from the study. Despite these limitations, there was no difference in socio-demographic and baseline clinical features between the groups. Although literature states that the majority of URTI are viral, field works show much more antibiotic usage [14]. Serious side effects of streptococcal pharyngitis affect both antibiotic usage and algorithms in URTI. Both centor and McIsaac criteria do not include viral symptoms. Mıstık et al. used fever below 37.5°C and absence of tonsillar exudate as viral markers [15]. In our study, we create a negative effect by converting age criteria of McIsaac to continuous variable and viral markers to 20 points equivalent to 1 criteria. In our own scoring by not exceeding 20 points for 6 viral parameters, we remained at the McIsaac scoring limits. Although we defined the algorithm as a guideline that should be taken into consideration by the physician’s decision mechanisms, not a necessity, the antibiotic prescription rate was 7.7% in the algorithm group. This ratio was 39.9% in the control group. As it is seen, the rate of antibiotic treatment of the algorithm group is 19% of the control group. The URTI, which is the most frequent cause of referral to family health centers, is naturally the most frequent cause of prescribing [16]. In our study, prescription fees were also compared. Algorithm group showed a significant decrease in prescription costs, and the most important factor affecting these prescription costs is the presence of antibiotics.
Conclusions
With this study, it is shown that 39.9% of antibiotic prescription rates of control group decreases to 7.7% (80% decreases) with the use of an algorithm with similar clinical results at 10th d visits. The given algorithm directly affected the antibiotic preference. Predominant factors affecting antibiotic prescription are the absence of cough and presence of high fever in algorithm group, sore throat in control group. The antibiotic prescription also directly affected the prescription price, and the average prescription price of the control group was found significantly higher. Although there are guidelines in the primary care practice, this behavioural change after a single training suggests that more training are necessary and application of record-based algorithm systems is required.
References
- Heikkinen T, Jarvinen A. The common cold. Lancet 2003; 361: 51-59.
- Fokkens W, Lund V, Mullol J. European position paper on rhinosinusitis and nasal polyps. Rhinol Suppl 2007; 20: 1-136.
- Gonzales R, Malone DC, Maselli JH, Sande MA. Excessive antibiotic use for acute respiratory infections in the United States. Clin Infect Dis 2001; 33: 757-762.
- Leblebicioglu H, Canbaz S, Peksen Y, Gunaydin M. Physician’s antibiotic prescribing habits for upper respiratory tract infections in Turkey. J Chemother 2002; 14: 181-184.
- Gill JM, Fleischut P, Haas S, Pellini B, Crawford A, Nash DB. Use of antibiotics for adult upper respiratory infections in outpatient settings: a national ambulatory network study. Fam Med 2006; 38: 349-354.
- Centor RM, Allison JJ, Cohen SJ. Pharyngitis management: defining the controversy. J Gen Intern Med 2007; 22: 127-130.
- Cento RM, Witherspoon JM, Dalton HP, Brody CE, Link K. The diagnosis of strep throat in adults in the emergency room. Med Decis Making 1981; 1: 239-246.
- McIsaac WJ, White D, Tannenbaum D, Low DE. A clinical score to reduce unnecessary antibiotic use in patients with sore throat. CMAJ 1998; 158: 75-83.
- Hart WJ. Streptococcal Pharyngitis-a demonstration of the inaccuracy of clinical diagnosis without culture: Can Fam Physician 1976; 22: 34-39.
- Choby BA. Diagnosis and treatment of streptococcal pharyngitis. Am Fam Physician 2009; 79: 383-390.
- Marin JC, Cubillo AS, Gomez-Escalonilla NC, Garzon JI, Benito LO, Reyes Fernandes MN. Is streptococcal pharyngitis diagnosis possible? Aten Primaria 2007; 39: 361-365.
- Pemberton J, Buehring A, Stonehouse G, Simpson L, Purves I. Issues and trends in computerisation within UK primary health care. Logistics Inform Manag 2003; 16: 181-190.
- Set T, Avşar Ü. Birinci basamakta üst solunum yolu enfeksiyonları. Eur J Family Med 2013; 2: 51-56.
- Higashi T, Fukuhara, S. Antibiotic prescriptions for upper respiratory tract infection in Japan. Intern Med 2009; 48: 1369-1375.
- Mistik S, Gokahmetoglu S, Balci E, Onuk FA. Sore throat in primary care project: a clinical score to diagnose viral sore throat. Fam Pract 2015; 32: 263-268.
- Yilmaz M, Mayda AS, Yüksel C, Filiz B, Seval O, Bayindir K, Sevinçer S. Bir aile hekimliği merkezi’ne başvuran hastalara konulan tanılar. Düzce Üniversitesi Sağlık Bilimleri Enstitüsü Dergisi 2012; 2: 7-13.