ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2023) Volume 34, Issue 1
Accuracy and validation of self-reported visual acuity by smart phone peek acuity application.
Talvir Sidhu1, Mohit Goyal1, Gurleen Kaur2, Vishu Bansal1, Kuldip Singh3, Chiman Lal1*
1Department of Ophthalmology, Government Medical College and Rajindra Hospital, Patiala, Punjab-147001, India
2Department of Anaesthesia, Government Medical College and Rajindra Hospital, Patiala, Punjab-147001, India
3Department of Biochemistry, Government Medical College and Rajindra Hospital, Patiala, Punjab-147001, India
- Corresponding Author:
- Chiman Lal
Department of Ophthalmology
Government Medical College and Rajindra Hospital
Patiala
Punjab-147001
India
Accepted date: March 3, 2023
Background: Testing visual acuity at home has become possible with advent of smart phone visual acuity applications like Peek. With increasing penetration of smart phones in developing countries like India, the general public can test their visual acuity at home. However, we do not know the accuracy and ease of use of these visual acuity applications at home, by the general public.
Aims: This study was conducted to determine self-measuring and self-reporting of visual acuity using Peek acuity application at home and further validation of the Peek acuity application compared to standard visual acuity testing.
Methods: The participants of age 18 and above, presenting to the Outpatient department, for non-opl acuiththalmic consultations, were invited to join the study by email or social media messaging platform. They were provided the link to the Peek acuity application and a link to the Google form questionnaire to self-report the visuay online. The participants who reported the visual acuity using the application were invited to report to the hospital, where visual acuity was repeated by Peek acuity application and Snellen’s standard visual acuity for validation.
Results: 501/625 (80%) invited participants did self-reporting of visual acuity done at home. The mean Peek acuity reported from home was 0.53 ± 0.33. 91% of participants reported that visual acuity application was easy to use at home. 199 eyes (100 persons), who presented to hospital, the mean home-based Peek acuity was 0.34 ± 0.33; hospital-based Peek acuity was 0.47 ± 0.31; hospital-based Snellen’s acuity was 0.45 ± 0.30. The sensitivity of hospital-based Peek acuity for detection of visual impairment (visual acuity<6/18) is 90.1% and specificity is 97.5%.
Conclusion: The response rate of self-visual acuity reporting was 80% using Peek acuity, suggesting it can be used in general public for vision reporting with a small risk of overestimation of visual impairment with selfreporting. However, there is excellent agreement between hospital-based Peek and Snellen’s acuity.
Keywords
Self visual acuity, Peek acuity, Home based vision testing, Peek validation.
Introduction
Blindness and visual impairment are a major health issue in the developing countries. According to National Programme for Control of Blindness and Visual Impairment (NPCBVI) India survey 2015-2019, cataract and refractive error collectively cause more than 80% of visual impairment in 50 years plus aged population and >50% of visual impairment in below 50 years aged population in India. Among avoidable causes, treatable causes of blindness and visual impairment are 68.1% and 85.7%. Early screening of visual acuity can help in early referral and treatment in major causes of visual impairment. The screening of visual acuity is largely being done for patients who seek eye related health care in hospital/clinic settings by eye care professionals. According to National Programme for Control of Blindness and Visual Impairment (NPCBVI) India survey 2015-2019, the prevalence of uncorrected visual impairment and blindness in population aged ≥ 50 years in India is 13.76% [1].
In addition to the huge population of visually impaired people, there is a lack of eye health care professionals in developing countries. In developed countries the ratio of Ophthalmologist to the population is 1:15800, while in India it is 1:100,000. This ratio is much less, 1:219,000 in rural to urban population-1:25000 [2]. In addition to the ophthalmologists, optometrists also play a vital role in detection of visual impairment and blindness, who are also <50,000 in number and <10,000 of them have a four-year training in optometry [3]. This suggests the need for addressing the problem of vision screening in the population for visual impairment at a lesser cost.
Visual acuity can be tested, to screen for visual impairment, in clinics using standardized tools like Snellen’s acuity charts, ETDRS LogMAR chart. The current gold standard of visual acuity testing is the LogMAR chart with retroillumination. It requires a five-optotype chart placed at four-meter distance for visual acuity testing. The Snellen’s chart, however, is a more commonly used chart for visual acuity testing across the globe and is comparable to LogMAR chart in clinic settings.
Incorporation of smart phone technology in daily medical practice has been increasing over the years due to its potential in health care information delivery, online tele-consultation, data collection software and patient monitoring [4]. There are various smart visual acuity testing applications freely available for android and iOS users such as EyeChart [5] and Peek Acuity [6]. The development and standardization of online applications for visual acuity testing applications like Peek visual acuity application makes it easy to measure visual acuity in absence of the above charts. At home visual acuity can be done to screen for visual impairment [7]. Peek acuity application (Ver. 3.5.13, London, UK) is a freely available application for visual acuity testing online. It has been developed by Peek Vision Ltd registered offices (90a High Street, Berkhamsted, Hertfordshire, England HP4 2BL (UK) and Unit G3, Victoria House, Plot 132 Independence Avenue, Gaborone (Botswana). It is used to test visual acuity using a smart-phone device at a distance of 2 meters. General public can test their visual acuity at home, thus, limiting in-person examination or facilitate early presentation of visual impairment [8,9].
We wish to evaluate the accuracy of self-examination of visual acuity at home using Peek acuity application and further validation of Peek acuity at hospital.
Materials and Methods
This prospective study was conducted on 625 participants recruited from both rural and urban community of Punjabi population to probe into self-reporting and self-measuring of visual acuity and easy instalment of smart visual acuity applications, who were presenting to the Government Medical College and Rajindra Hospital, Patiala for non-ophthalmic consultation like medicine, surgery, dermatology, ENT etc. Ophthalmologists/ optometrists/ trained opticians were excluded from the study. The subjects were invited to join the study by email or social media messaging platform like Whatsapp (Figure 1). They were provided the link to Peek acuity application and instructions to use the application in English as well as in vernacular language. Participants were instructed to watch the tutorial before checking and reporting the visual acuity. Along with the application and tutorial link, the subjects were provided a link to an online questionnaire for reporting their results and ease of administration of visual acuity. A written and informed consent was taken from the subjects in the questionnaire. 501 subjects participated to self-test their own visual acuity and report the results via online questionnaire.
Ease of use of application was assessed using four questions
1. Were you able to install the app easily?
2. Was the tutorial easy to understand?
3. Were you able to easily use the application?
4. Can you use it easily in a non-professional setting like at home?
Each question had 4 options on Likert scale: Very Easy, Easy, Difficult and Asked For Help, which were scored as Very Easy=4, Easy=3, Difficult=2, Asked For Help=1. Further, the scores of all questions were added and classified as EASY (final score 13-16), MODERATE (final score 9-12) and DIFFICULT (final score 4-8).
All 501 participants were invited telephonically to the hospital for validation of Peek acuity application for comparing to standard visual acuity testing. 100 subjects who tested their own visual acuity at home presented to hospital for checking of visual acuity using Peek as well as Snellen’s acuity with available correction. The visual acuity at the hospital was checked by Peek and Snellen’s acuity chart using available correction by separate observers. The self-reported Peek visual acuity and the agreement between hospital-based Peek and Snellen’s were analysed.
The visual acuity values were converted to decimal values for comparison and validation of applications. The definition of visual impairment and blindness was taken from the National Programme for Control of Blindness and Visual Impairment (NPCBVI) survey of India [1].
Biostatistical analysisData entry was done in Microsoft excel. STATA software version 12.1 (Stata Corp LP, College Station, TX) was used for data analysis. A P-value less than 0.05 was considered statistically significant.
Ethical Clearance in the study protocol was approved by the Institutional Ethics Committee vide letter no-Trg. (310)2022/24756, dated: 27/07/2022. The study details were explained to the participants and a written informed consent was taken voluntarily before participating into the study.
Results
Baseline data
Baseline data observed in the study are summarized in Table 1. A total of 625 persons were sent the link to the application. Out of the 625, 501 (80%) persons responded to the questionnaire, out of which 256 (51%) were females and 245 (49%) were males. The mean age of the participants was 35.19 ± 14.33 years; 36.7 ± 14.3 in females and 33.6 ± 14.2 in males, P=0.15. The participants were educated to graduate level in 35%, 12th pass in 33.2%, postgraduate in 15.7%, 10th pass in 8.9%, and elementary school educated in 7.1% of cases. A total of 380/501 (76%) subjects used spectacles and 121/501 (24%) did not use spectacles. Out of the total 380 subjects using spectacles, 223 (44%) used only distance glasses, 43 (8.6%) used only near glasses and 114 (22.7%) used both near and distance glasses. The average age of subjects who used distance glasses was 28 ± 9.7 years as compared to persons who used both near or near distance glasses 50 ± 13.2 years.
| Males | Females | Total | |
|---|---|---|---|
| Total | 245 | 256 | 501 |
| Age categories | |||
| 0-19yrs | 22 (9.0%) | 18 (7.0%) | 40 (8.0%) |
| 20-29yrs | 113 (46.1%) | 88 (34.4%) | 201 (40.1%) |
| 30-39yrs | 25 (10.2%) | 31 (12.1%) | 56 (11.2%) |
| 40-49yrs | 38 (15.5%) | 55 (21.5%) | 93 (18.6%) |
| 50-59yrs | 35 (14.3%) | 52 (20.3%) | 87 (17.4%) |
| 60-69yrs | 9 (3.7%) | 10 (3.9%) | 19 (3.8%) |
| 70-79yrs | 3 (1.2%) | 2 (0.8%) | 5 (1.0%) |
| Education Status | |||
| Elementary | 12 (4.9%) | 24 (9.4%) | 36 (7.1%) |
| 10th pass | 17 (6.9%) | 28 (10.9%) | 45 (8.9%) |
| 12th pass | 86 (35.1%) | 80 (31.3%) | 166 (33.1%) |
| Graduate | 95 (38.8%) | 80 (31.3%) | 175 (34.9%) |
| Post-Graduate | 35 (14.3%) | 44 (17.2%) | 79 (15.7%) |
| Spectacle use | |||
| Distance | 119 (48.5%) | 104 (40.6%) | 223 (44.5%) |
| Near | 19 (7.75%) | 24 (9.4%) | 43 (8.6%) |
| Bifocal | 48 (19.6%) | 66 (25.8%) | 114 (22.8%) |
| None | 59 (24.1%) | 62 (24.2%) | 121 (24.2%) |
Table 1: Baseline characteristics of participants.
Peek acuity testing and reporting from home
Peek visual acuity measurement at home were converted to decimal values. The mean decimal visual acuity reported at home in right eye was 0.54 ± 0.32 and in left eye was
0.52 ± 0.33. Further visual acuity grouping was done in 4 groups 6/6-6/12, <6/12-6/18, <6/18-6/60 and <6/60. The older age group >59 years of age reported significantly lower mean decimal visual acuity of 0.29 ± 0.21 as compared to younger age groups (P<0.001). Visual acuity of 6/6-6/12 was reported in 48% right eyes and 46.5% left eyes. Visual acuity of <6/12-6/18 was reported in 28.5% right eyes and 25.15% of left eyes. Visual acuity of <6/18- 6/60 was reported in 15% right eyes and 18.16% left eyes. Visual acuity of <6/60 was reported in 8% right eyes and 10.18% left eyes (Table 2). It was noted that majority of participants reported similar visual acuity in both eyes. 25.6% of eyes were visually impaired.
| Visual acuity | Right eye | Left eye | Total eyes | |||||
|---|---|---|---|---|---|---|---|---|
| No | % | Mean age ± SD | No | % | Mean age ± SD | No | % | |
| 6/6-6/12 | 243 | 48.5% | 33.71 ± 13.04 | 233 | 46.50% | 33.17 ± 12.91 | 476 | 47.5% |
| <6/12-6/18 | 143 | 28.5% | 35.86 ± 14.61 | 126 | 25.15% | 36.24 ± 14.35 | 269 | 26.8% |
| <6/18-6/60 | 75 | 15.0% | 39.33 ± 16.19 | 91 | 18.16% | 39.01 ± 15.78 | 166 | 16.5% |
| <6/60 | 40 | 8.0% | 34.33 ± 15.68 | 51 | 10.2% | 35.60 ± 16.36 | 91 | 9.1% |
Table 2: Number and mean age of 501 persons who reported visual acuity in either eye from home.
Visual impairment using peek acuity
Out of 501 persons, 121 (24%) reported visual impairment and 23 (4.6%) reported blindness. There was no significant difference between number of males or females having visual impairment; P=0.43. The mean age of persons who had normal vision and visual impairment was statistically insignificant; P=0.23 (Table 3).
| Males | Females | Total | |
|---|---|---|---|
| Normal | 179 (73.1%) | 178 (69.5%) | 357 (71.6%) |
| Visual Impairment | 55 (22.4%) | 66 (25.8%) | 121 (24.2%) |
| Blindness | 11 (4.5%) | 12 (4.7%) | 23 (4.6%) |
Table 3: Visual acuity reporting from home in 501 persons. Visual Impairment=Vision<6/18 in better eye. Blindness=Vision<3/60 in better eye.
Ease of using the peek application
The mean score for ease of installation of application was 3.4 ± 0.77. 94% of people reported that it was very easy or easy for them to install the application whereas 6% asked for help to install the application. The tutorial for the application was found easy or very easy by 89% of participates, while it was difficult or they had to ask for help in 11% of cases. The use of application to provide visual acuity was found easy by 86%, whereas 14% found it difficult or asked for help in using the application. 91% participants found the application easy to use in a nonprofessional setting like at home and 9% had to ask for help to use the application. (M:F P=0.35) We found that people educated upto elementary school found it more difficult to perform the self-visual acuity testing at home. P<0.001 471(94%) percipients reported that the application was reliable for checking visual acuity further at home on selfbasis. The mean final score for application was 13.2 ± 2.9 (4-16). It was graded to derive the overall ease of using the application at home as EASY in 312/501(62%) (final score 13-16), MODERATE in 152/501 (30%) (final score 9-12) and DIFFICULT in 37 (8%)(final score 4-8) (Table 4).
| Number of Participants | Were you able to install the app easily? | Was the tutorial easy to understand? | Were you able to easily use the application? | Can you use it easily in a non-professional setting like at home? |
|---|---|---|---|---|
| Asked for Help (Score=1) | 29 | 32 | 56 | 40 |
| Difficult (Score=2) |
2 | 22 | 13 | 5 |
| Easy (Score=3) |
175 | 193 | 210 | 252 |
| Very Easy (Score=4) |
295 | 254 | 222 | 204 |
| Can you rely on it for checking visual acuity further at home on self-basis? | Yes = 471 | No= 30 | ||
Table 4: The number of persons according to the score in the application based upon 4 questions.
Agreement of home-based peek, hospital-based peek acuity with snellen’s acuity
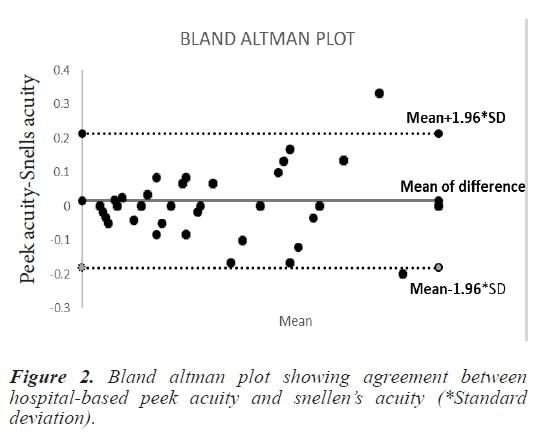
199 eyes of 100 participants who visited the hospital after use of Peek acuity underwent visual acuity testing using Peek and Snellen’s chart and refraction at the hospital using standard Snellen’s chart at 6 m. The mean age of these participants was 45 ± 15.7 years. The persons who presented to the hospital were older as compared to the persons who reported the home-based visual acuity. When compared the Home-based Peek acuity to Hospitalbased Peek acuity, the mean home-based Peek acuity was 0.34 ± 0.33; hospital-based Peek acuity was 0.47 ± 0.31; hospital-based Snellen’s acuity was 0.45 ± 0.30 and a mean difference of -0.015 ± 0.10. The median homebased Peek acuity was 0.3, hospital-based Peek acuity was 0.4 and median hospital-based Snellen’s acuity was 0.5. 54/199 (27.1%) eyes had a visual acuity difference >0.1 between home-based vs. hospital-based Peek. The difference in home-based Peek vs. hospital based Peek acuity was attributed to poor understanding of instructions or not using glasses while testing visual acuity. The median difference between home-based Peek and hospitalbased Peek acuity was 0. The median difference between hospital-based Peek and Snellen’s was 0. In 141 (70%) eyes recorded a difference of less than ± 0.08 between hospital-based Peek and Snellen’s visual acuity. On the Bland Altman analysis, there was good agreement between hospital-based Snellen’s acuity and Peek acuity (Figure 2). The sensitivity of hospital-based Peek for detection of visual impairment (visual acuity <6/18) is 90.1% and specificity is 97.5%.
Discussion
Amongst the smart visual acuity applications, Peek has been standardized for measuring visual acuity in normal as well as diseased eyes. The smart phone penetration rate has increased from 23% in 2016 to 54% in 2020 [10]. With the availability of smart phone based visual acuity applications, visual acuity can be easily tested at home. We found that 62% people found it easy to use the application and were able to report the visual acuity. Majority of participants had visual acuity more than 6/60 in 92%, while very few had less than 6/60 vision. Majority of participants who responded to the study were 10th class pass or above, with <15% being elementary school education. Only 8% participants found the application difficult and had to ask for help in using the application, majority of them had lower education. We found that 80% of the patients who were given the link were able to test and report their visual acuity through an online survey. Out of the people who reported the visual acuity from home, 28% of the persons were not able to correctly report their visual acuity. Since majority of people were educated and had good visual acuity, therefore this study cannot give an estimate whether this application can be used with similar ease in less educated individuals; or similar accuracy in people with low vision.
Davara et al., also studies the feasibility of using the Peek app to measure visual acuity at home and found that vision measurements of Peek Acuity app were comparable with COMPlog. They measured the acuity both at baseline and after 1-week measurement, and found that it did not depend upon the underlying ocular condition or educational level of the caregivers/patients. Most caregivers (95%) felt the app was easy to use [11]. Painter et al., studied home based visual acuity testing in children which was undertaken by their parents. They found that home testing uptake depended upon the subjects. They also reported that majority families found it easy to test visual acuity at home. They also found a bias of 0.14 LogMAR in visual acuity with home based acuity being lesser than hospital based acuity [12]. Peter et al., studied educated participants and their willingness to test the visual acuity using smart phone based applications. They noted that 96% of persons found it easy to test their visual acuity using the smart phone applications [13]. Although Peek acuity has a high test-retest reliability [6], it is apparent that home based acuity testing is dependent upon the participants ability to understand the process of testing visual acuity.
When we compared home-based Peek to hospital based Peek acuity, we found a median difference of 0.1 in the decimal visual acuity values which suggests that homebased readings were lower as compared to hospital-based readings. The rate of moderate-severe visual impairment in India is 13.77% in population aged >50 years and 2.55% in all age groups. The high rate of visual impairment (24%) in our study is because the participants did not use glasses while reporting their visual acuity. Peek acuity application tutorial does not give any clear instruction whether participants should wear distance glasses while testing visions.
When we compared the Snellen’s application to visual acuity by Peek (in hospital testing), we found a mean difference of only -0.015, which translated to less than one line difference on Snellen. We also found that 50% of eyes did not show any difference between Peek and Snellen acuity. A study by Bhaskaran et al., comparing Peek to Snellen acuity found a mean difference of -0.02 between the methods, which is clinically acceptable. Bastawrous et al., found a mean difference of -0.07 between Peek and Snellen’s acuity in the clinic and a mean difference of 0.029 between home based Peek and home based Snellen’s [14]. Satgunam et al., found that Peek acuity had comparable results to COMPlog [15]. It is also important to note that while Snellen acuity comes in discrete decimal values of 1, 0.67, 0.5, 0.33, 0.25 etc., Peek acuity application gives extra or midway values between these decimals, such as 0.8, 0.4. These subtle differences between the decimal values lead to lower agreement scores between two applications despite visual acuity difference of less than one line.
The major advantage of our study is that we studied the application for home based visual acuity and we validated the visual acuity studied in a subset of eyes by inviting the patients to hospital for visual acuity measurement. The limitations of our study are that Peek acuity reports more visual impairment due to unclear instructions, whether to use glasses or not and the decimal values which fall in between the Snellen lines, thereby giving a falsely high difference. Also, we were not able to compare the effect of education on the use of this application as less than 15% of our participants were elementary school educated.
This study bridges the knowledge gap related to utility of self-diagnosis in ophthalmology for visual acuity. We find that Peek visual acuity is accurate and can be used by people at home to screen for vision at home, after carefully watching the tutorial. According to this study, it can be implicated that these smart visual acuity applications prove to be of immense help in self-diagnosing visual impairment.
Conclusion
This study shows that 80% of people who were sent an application link were able to report their visual acuity through an online survey, which suggests the possibility of collecting this data on a large scale in educated population. More than 90% of participants reported that the Peek visual acuity application was easy to use and reliable to record visual acuity. Almost one third of persons who reported the visual acuity from home, reported morethan- one-line lower visual acuity as compared to hospitalbased Peek acuity, which suggests overestimation of visual impairment when visual acuity is tested at home by the participants. The hospital-based Peek visual acuity application validated with standard Snellen’s visual acuity, in a subset of population who presented to the hospital, showed excellent agreement.
Acknowledgment
We thank the participants for being a part of the study.
Conflict of Interest
None