ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2020) Volume 31, Issue 6
A paradigm shift in the cost of illness of T2DM in south India: A prevalence based study.
Introduction: Objective of the study was to estimate the cost of illness of uncomplicated versus complicated type 2 diabetes mellitus. The study also aimed to find out the trend of cost of illness of the disease over a decade.
Methodology: A prevalence based bottom-up approach study was carried out in two tertiary care hospitals after ethical approval. Data of annual laboratory, pharmacy, consultation, hospital bed, surgical costs of 238 diabetics in 2008 and 340 diabetic patients in 2017 respectively were obtained. Patients were divided in to six groups, uncomplicated and different complications of diabetes. Different costs incurred in 2008 and 2017 in these groups were compared, to study the trend of cost of illness using suitable statistical tests.
Results: Uncomplicated patients incurred significantly lower costs (P<0.0001) compared to other groups. Patients with IHD had highest medical expenses (P<0.0001), followed by DN and DF (P<0.0001). Cost incurred in management of DM in 2017 was found to be higher 1.4-2.7 times when compared to that in 2008.
Conclusion: It is evident from the study that the economic burden due to T2DM is substantial. It poses a significant financial burden on healthcare system, individual and society.
Keywords
COI, Diabetes mellitus, A bottom-up approach, Economics.
Introduction
Diabetes Mellitus (DM) is a disease that has significant economic impact on both for the patient and the health- care provider due to its chronicity and multi-organ involvement which results in frequent visit and admission to health facilities. High prevalence and higher rate of Complications endanger substantial negative implication on the economies.
Costs involved in the management of diabetes can be classified into direct and indirect or intangible costs. Direct cost includes hospital services, including consultation charges, laboratory tests, and the daily management of DM, which includes the availability of products such as insulin, syringes, oral hypoglycemic agents, and blood glucose testing equipment which are known as pharmacy costs. Due to coexisting complications, patients may have hospital admissions and undergo various interventions/ surgeries which enormously increase the direct costs. Transportation cost is known as direct non-medical cost. Costs range from relatively low-cost items, such as primary- care consultations and hospital outpatient episodes, to very high-cost items, such as long hospital inpatient stays for the treatment of complications [1]. Indirect cost includes loss of productivity due to sickness, absenteeism, disability, premature retirement, and premature mortality of the patients. Due to these expenses, DM poses a great economic burden on the society which is of great concern[2,3].
Shobhana et al. reported a total annual cost of INR 4510 in a public sector hospital at Chennai in 1999, whereas the same author reports cost for hospitalization INR 5925 in 2004 [4]. In 2005, three study reports are available to the best of our knowledge, among which cohort study in Northern India by Grover et al. reported a total cost of INR 4966.2 over 6 months in patients with diabetes inclusive of consultations, investigations, nursing, and infrastructure. He also reported an indirect cost due to loss of wages was INR 2086.74, which also included drugs, food, and travel [5]. However, small sample size was the limitation of the study. Kumar et al. reported a total direct cost of INR 6212.4, inclusive of tests, drugs, monitoring, etc., in his cohort study conducted in Delhi [6]. Ramachandran et al., in a cross-sectional study covering seven states in India, reported an annual direct cost of INR 8130 which included drugs, tests, hospitalization, surgery, and consultation [7]. A regional cohort study by Shivprakash et al. suggests a consultation charge of INR 363 [8]. In our previous report, we found that annual cost per diabetic person was INR 10,584, 19,326, and 25,960 for uncomplicated, complicated but not admitted, and complicated and admitted diabetics, respectively, in 2009 [9]. A study by Kumpatla et al. reports an annual expenditure of INR 4493 and 15280 with and without complications, respectively, in Chennai in 2009 [10]. A cross-sectional study from Maharashtra, by Kuchake et al. in 2010, reported a consultation cost of INR 116.85 and a Punjab-based study by Joshi et al. reported a consultation cost of INR 166 [11,12]. In 2012, Hanamkonda-based cohort study by Akari et al. reported an annual direct cost of USD 314.15 in complicated diabetic patients and USD 29.91 in uncomplicated diabetic patients [13]. In a South India based randomized clinical trial by Abdi et al. reported a drug cost of USD 13.42 [14].
There are various studies which tried to evaluate the economic burden due to DM, but each one of them has its own limitations due to lack of standardization of the methods used, improper documentation of data, lack of follow-up, etc. This study is an attempt to evaluate the economic burden of diabetes in coastal district of Karnataka.
The expensive cost of treating Type 2 Diabetes and the rising prevalence will impose a heavy burden on economy, and major challenges to health policy makers in developing countries in managing this chronic disease. Non-standardized methods used in assessing and reporting economic burden and poor quality of documentation of secondary data in most developing countries are the obstacles faced in the evaluation of diabetes mellitus. The availability and accuracy of data of cost of illness study is most important to assess the current approach in management of this chronic disease.
Objective of the study was to estimate the cost of illness of uncomplicated versus complicated type 2 diabetes mellitus in Coastal Karnataka, India. The study also aimed to find out the trend of cost of illness of the disease over a decade.
Hypothesis
Health care cost incurred due to diabetes mellitus poses an economic burden on the society in India. Health care cost is more in complicated diabetics as compared to those without any complications. Health care cost is directly proportional to the duration of the disease.
Objectives
Primary objectives were to
1. Compare direct costs like, annual medical cost (AMC), annual laboratory cost (ALC), annual pharmacy cost(APC), annual consultation cost (ACC), annual hospital bed costs(AHBC) and annual surgical/intervention cost(ASC) in type 2 diabetes mellitus (T2DM) patients, with and without complications.
2. Compare AMC and other costs in diabetics with various complications
3. Find out total cost incurred in hospitalized complicated diabetics.
4. Find out correlation between cost incurred to duration of diabetes.
5. Find relationship between glycemic status, complications of DM and cost incurred.
6. Compare the health care cost incurred with the data obtained in the past decade in the same geographical area.
Methodology
Study design
Type of study: Prevalence based bottom up approach
Study population: 238 diabetics and 340 diabetic patients respectively from two hospitals were obtained from the medical record sections.
Inclusion criteria
A prevalence based bottom-up approach study was carried out in two tertiary care hospitals located in Coastal Karnataka after ethical approval. 340 T2DM patients, 18 to 55 years of either gender, attending Justice KS Hegde Hospital, Nitte University, Mangalore for at least 1 year were included in the study (2017-18). Patients attending the hospital services, with and without complications were included in the study. Patients with T2DM were identified by American Diabetic Association guidelines 2017. Diabetes complications and co-morbidities were identified using ICD codes. Systematic sampling was conducted for 340 identified DM patients after obtaining permission from the Medical superintendent and institutional ethics committee.
238 diabetics attending TMA Pai hospital in the year 2008-09 with or without complications were also included in the study.
Exclusion criteria
Type 1 diabetics, gestational diabetes and those with any other associated illnesses, other than diabetic complications, like liver disorders etc. were excluded from the study.
Study period
Data was collected from the medical records of diabetics who obtained treatment between 2008-2009 and 2017- 2018.
Sampling technique
The non-interventional retrospective study with prevalence based bottom up approach was conducted in a multispecialty teaching hospital attached to a medical college. It caters tertiary health care service to the costal district of Karnataka state, India. The data of patients such as age, gender, duration of illness, complications of diabetes, number of hospital visits per annum for consultation and admission, glycated haemoglobin (HbA1C) levels, Annual Medical Cost (AMC) like Annual Pharmacy Costs(APC), Annual Consultation Cost (ACC), Annual Laboratory Cost (ALC), Annual Hospital Bed Charges(AHBC), annual surgery cost (ASC) of patients who have been receiving regular treatment for type 2 diabetes mellitus from July 2016 to, June 2017 were collected from the hospital medical record department. Patients were classified into six groups i.e. patients with no complications (uncomplicated) (UC), group I, patients with diabetic complication who were hospitalized during one year with different complications like diabetic retinopathy (DR)-group II, diabetic nephropathy (DN) group III, diabetic foot (DF) group IV, diabetic neuropathy (DNeu)- group V, ischemic heart disease/coronary vascular diseases (IHD)-group VI. The AHBC, ALC, APC, ACC, ASC and total annual cost medical cost (AMC) during hospitalization were calculated separately for each group. Data was collected from the hospital medical record section.
A retrospective study was also conducted in a multispecialty teaching institute which caters tertiary health care service to the costal district of Karnataka state, India in 2008- 2009. The research protocol was approved by the Manipal university ethics committee. The data of 238 patients such as age, sex duration of illness, complications of diabetes, number of hospital visits per annum for consultation and admission, glycosylated haemoglobin levels, Annual Medicine Cost (AMC), annual consultation cost (ACC), Annual Laboratory Cost (ALC), annual hospital bed charges (AHBC), Annual Surgery Cost (ASC) who were receiving regular treatment for type 2 diabetes mellitus from Jan 01, 2008 to Dec 31, 2008 were collected from the hospital medical record department. We classified the patients into six groups as mentioned above. The AMC & ACC spent in a year was calculated for each patient and the mean value was calculated for each group. In addition the AHBC, AMC, ACC, ASC and total annual cost during hospitalization were also calculated.
The data obtained in 2017 was compared to the data collected in 2008-2009, both from the private medical college teaching hospitals in the same geographical area so as to study the trend of the disease.
Estimation of costs
Direct DM-related costs were classified by the type of service, including inpatient hospitalisation, Accident and Emergency (A&E) and ambulatory outpatient care (physician visits, allied health visits, laboratory tests and medications). Allied health visits include foot screening, eye screening. The total medical costs were estimated by the total before-subsidy charges, which is the total medical bill before any deduction for government subsidies or insurance claims. All costs were reported in INR. The cost of inpatient care and A&E services were estimated by the total charge based on the length of stay and resources used. Any A&E visits that resulted in hospitalization were included as inpatient care costs. Unit costs used in the estimation of physician visits, which included visits to physicians and other consultants, were noted. Therefore, costs were estimated by multiplying the number of physician visits by the unit cost of a visit. The cost for drugs used for treatment of complications in addition to anti-diabetic medications were be included under pharmacy cost. Direct non-medical costs, such as transportation expenses were also included.
Data was collected from the Medical Record Department of Justice KS Hegde Medical Hospital, where patient records were fully computerized as per ICD classification.
Delimitations
An intangible cost that may occur due to loss of pay due to absenteeism or loss of productivity was not taken in to account in the present study. Monthly income as well as educational status of patients was not included in the study as the data collection was from medical records and it was not directly from patients.
Data analysis and interpretation
The data collected was scrutinized and coded before entering in computer. The data was analysed using the software SPSS version 16. The entered data was verified and checked for data errors during coding and data entry.
Data availability statement
Individual de-identified may be shared.
Statistical tests used
Descriptive statistics was used for calculating mean, standard error of mean (SEM), percentage, median.
Kruskal Wallis test followed by post-hoc test, Dunn’s test was used to compare median costs between the groups, as well as to compare costs in different groups based on duration of illness as well as complications. Spearman’s correlation test was used to find the correlation between duration of illness and direct medical cost as well as glycemic status and medical costs (Table 1).
| Characteristics | |
|---|---|
| Gender | Male: female – 60:40 |
| Mean age in years | 58.96 ± 2.56 |
| Duration of disease in years | 8.41 ± 1.09 |
| Hb1Ac (%) | 7.69 ± 0.11 |
Table 1: Demographic profile with glycemic parameters.
Results
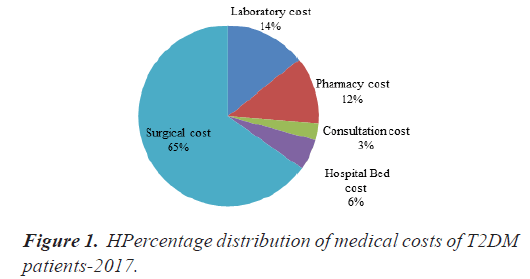
Total direct mean and median medical costs of patients are depicted in Table 2. Comparison of mean and median costs in different groups is depicted in Table 3. Post hoc test results depicting comparison of costs incurred in different groups in individual costs are depicted in Tables 4-10.Percentage contributions of ALC, APC, ACC, AHBC and ASC to total direct medical cost (AMC) are depicted in Figure 1.
| Costs in INR (Mean ± SEM) | Median | |
|---|---|---|
| Annual total medical cost(AMC) | 31500 ± 1841.94 | 17587.5 |
| Annual Laboratory cost(ALC) | 5874.23 ± 325.4 | 4118.9 |
| Annual pharmacy cost(APC) | 4772.42 ± 367.75 | 2399.9 |
| Annual consultation cost(ACC) | 1239.46 ± 92.059 | 949.55 |
| Annual hospital bed cost(AHBC) | 2246.49 ± 155.699 | 1147.55 |
| Annual surgical cost(ASC) | 26500 ± 1605.65 | 14629 |
| Annual transportation cost(ATC) | 1800 ± 145.1 | 1750 |
Table 2: Annual mean and median costs in T2DM.
| Costs in INR | UC (I) (n=117) | DR(II) (n=32) | DN(III) (n=41) | DF(IV) (n=25) | DNeu(V) (n=54) | IHD(VI) (n=71) |
|---|---|---|---|---|---|---|
| AMC | 14230 ± 1564.6 | 23643 ± 3223.4 | 39374 ± 4141.1 | 39520 ± 5010.1 | 25021 ± 3802.2 | 61769 ± 5560.6 |
| ALC | 3369.3 ± 307.3 | 6296.9 ± 1086.3 | 7032.1 ± 1081.1 | 7537.2 ± 1293.6 | 5221.8 ± 844.02 | 9601.9 ± 780.91 |
| APC | 1651.3 ± 259.77 | 4013.3 ± 676.4 | 6433.6 ± 1119.5 | 8884.3 ± 2331.7 | 3893.8 ± 685.5 | 8328.8 ± 912.5 |
| ACC | 826.5 ± 78.7 | 1686.9 ± 485.5 | 1767.4 ± 248 | 1752.6 ± 224.9 | 1483 ± 278.1 | 2799.1 ± 333.25 |
| AHBC | 1150.6 ± 154.54 | 1631 ± 522.44 | 1883.9 ± 296.51 | 2692 ± 685.29 | 1354.2 ± 220.46 | 3274.2 ± 483.38 |
| ASC | 11652 ± 136.21 | 19900 ± 2764.9 | 28237 ± 2865.1 | 37189 ± 4909.2 | 21437 ± 3429.9 | 53724 ± 4910.2 |
Table 3: Mean costs incurred in uncomplicated and complicated diabetes mellitus.
| Costs in INR | UC (I) (n=117) | DR(II) (n=32) | DN(III) (n=41) | DF(IV) (n=25) | DNeu(V) (n=54) | IHD(VI) (n=71) | P value |
|---|---|---|---|---|---|---|---|
| AMC | 7750 | 17587.5 | 35875 | 30980 | 15237.5 | 55450 | <0.0001 |
| ALC | 1919.8 | 3758.5 | 6405 | 6695 | 3016.05 | 10462.3 | <0.0001 |
| APC | 936.5 | 3161.9 | 5540 | 5758 | 2418.65 | 8801.6 | <0.0001 |
| ACC | 490 | 1154.8 | 1667.2 | 1765 | 915.5 | 1535 | <0.0001 |
| AHBC | 552 | 784.6 | 1514.4 | 1569 | 614.4 | 2183.9 | <0.001 |
| ASC | 6631 | 14936.4 | 30402.5 | 31631 | 12743.65 | 48860 | <0.0001 |
Table 4: Median costs incurred in uncomplicated and complicated diabetes mellitus.
| Groups | P value |
|---|---|
| I vs. III | <0.0001 |
| I vs. IV | 0.001 |
| I vs. VI | <0.0001 |
| II vs. VI | <0.0001 |
| III vs. VI | 0.001 |
| IV vs. VI | 0.014 |
| V vs. VI | <0.0001 |
Table 5: Comparison of AMC in different groups.
| Groups | P value |
|---|---|
| I vs. III | 0.003 |
| I vs. IV | 0.013 |
| I vs. VI | <0.0001 |
| V vs. VI | <0.0001 |
Table 6: Comparison of ALC in different groups.
| Groups | P value |
|---|---|
| I vs. III | <0.0001 |
| I vs. IV | <0.0001 |
| I vs. VI | <0.0001 |
| II vs. IV | 0.028 |
| II vs. VI | 0.008 |
| IV vs. V | 0.010 |
| V vs. VI | 0.001 |
Table 7: Comparison of APC in different groups.
| Groups | P value |
|---|---|
| I vs. III | 0.004 |
| I vs. IV | <0.0001 |
| I vs. VI | <0.0001 |
| II vs. VI | <0.0001 |
| III vs. VI | <0.0001 |
| V vs. VI | <0.0001 |
Table 8: Comparison of ASC in different groups.
| Groups | P value |
|---|---|
| I vs. VI | <0.0001 |
| V vs. VI | 0.002 |
Table 9: Comparison of ASC in different groups.
| Groups | P value |
|---|---|
| I vs. VI | <0.0001 |
| II vs. VI | 0.034 |
| V vs. VI | 0.001 |
Table 10: Comparison of AHBC in different groups.
A very highly significant differences (P<0.0001) in AMC, ALC, APC, ACC, AHBC and ASC between all the groups (Table 2).
Uncomplicated patients (Gp I) had significantly lower costs (P<0.0001) compared to other groups. Patients with IHD (Gp VI) had highest expenses (P<0.0001), followed by DN (Gp III) and DF (Gp II) (P<0.0001).Cost incurred in DNeu (Gp V) was almost the double compared to uncomplicated group, but AMC was minimum among other diabetic complications. DR (Gp II) had higher expenses compared to DNeu (Gp V) (Table 3 and 4).The similar pattern of distribution was observed in other individual costs.
When we consider total direct medical cost, cost due to surgery/intervention contributed to 65%, lab charges 14%, pharmacy and medications 12%, bed charges due to hospital admissions 6% and consultation charges 3% (Figure 1).
On analysing different costs in all the six groups, it was found that surgical/interventional costs contribute to 59%- 69% of total direct medical costs, ALC to 12%-19%, APC made up to 9%-15%, ACC contributed to 3%-5% and AHBC accounted for 4%-6% of annual direct medical cost (AMC) (Table 3).
A positive correlation was observed between duration of complications and cost incurred (r=0.743, P<0.001).There was a negative correlation between the glycemic status and cost incurred (r=-0.604, P<0.001).
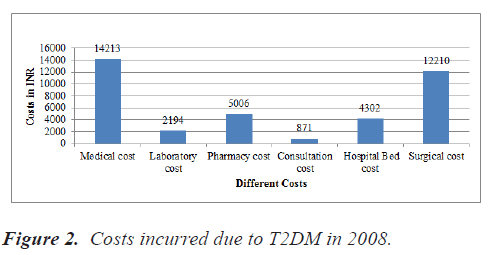
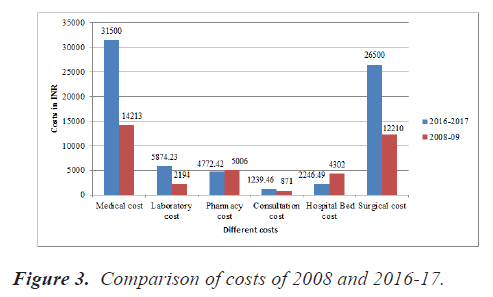
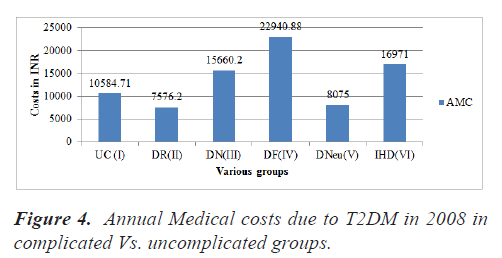
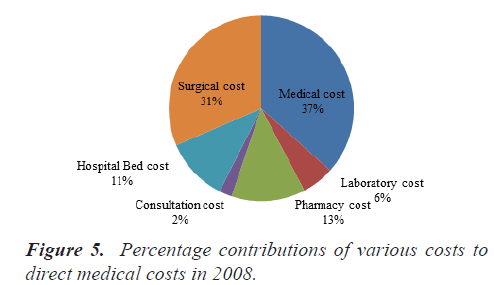
Costs incurred in T2DM in 2008, comparison of various costs of 2008 and 2017, annual medical costs incurred due to T2DM in 2008, percentage distribution of various costs in 2008 are depicted in Figures 2-5 respectively.
On comparison of data of 2008-09 with that of 2016-2017, it was observed that AMC raised by 2.22 times, ALC 2.68 times, ACC 1.42 times and ASC raised by 2.17 times over 8 years of duration. On the contrary, a lowered APC by 0.95 times and AHBC declined by 50% (Figure 3). Figures 4 and 5 depict total direct costs in various complications and percentage contribution of different costs to direct medical cost in T2DM in the year 2008.
The medical cost includes both direct and indirect cost spent by the patient. The different direct type of direct medical cost spent by the patient in 2008 and 2017, inflation adjusted cost and percentage change in the cost spent by the patient in each category were depicted in Table 11. It was evident that hospital bed charges and pharmacy costs have significantly decreased even after considering the inflation from 2008 to 2017. There was no change in the annual consultation cost. However the rest of the costs i.e. total medical cost, laboratory cost and surgery cost were significantly increased.
| Type of Cost | Cost incurred in 2008 (In INR) | Cost incurred in 2017 (In INR) | Inflation adjusted Cost (In INR) | Percentage increase of cost incurred (%) |
|---|---|---|---|---|
| Medical | 14213 | 31500 | 20229.36 | 35.77 |
| Lab | 2194 | 5874 | 3122.72 | 44.83 |
| Pharmacy | 5006 | 4272 | 7125.3 | -66.79 |
| Consultation | 871 | 1239 | 1239.69 | 0 |
| Hos. Bed | 4302 | 2246 | 6123.03 | -172.61 |
| Surgery | 12210 | 26500 | 17378.49 | 34.42 |
Table 11: Cost incurred in 2008 and 2017 with the trend in change in cost in various groups.
The annual cost spent by the patient in six different groups in 2008 and 2017 were mentioned in Table 12. Except in uncomplicated diabetes patient group, all the other groups have seen an increase in cost spent annually.
| Type of Annual Medical Cost | Cost incurred in 2008 (In INR) | Cost incurred in 2017((In INR) | Inflation adjusted Cost((In INR) | Percentage increase of cost incurred (%) |
|---|---|---|---|---|
| Uncomplicated diabetes | 10584 | 14230 | 15064.52 | -5.53 |
| Diabetic retinopathy | 7576 | 23643 | 10783.14 | 54.39 |
| Diabetic nephropathy | 15660 | 39374 | 22289.34 | 43.39 |
| Diabetic foot | 22940 | 39520 | 32651.19 | 17.38 |
| Diabetic neuropathy | 8075 | 25021 | 11493.38 | 54.06 |
| Ischemic heart disease | 16971 | 61679 | 24155.33 | 60.83 |
Table 12: Cost incurred in 2008 and 2017 with the trend in change in cost in various groups.
Discussion
A very highly statistically significant differences (P<0.0001) were observed in AMC, ALC, APC, ACC, AHBC, and ASC between all the groups (Table 2). Uncomplicated patients (Group I) had significantly lower costs (P<0.0001) compared to other groups. Patients with IHD (Group VI) had highest expenses (P<0.0001), followed by DN (Group III) and DF (Group II) (P<0.0001). Cost incurred in DNeu (Group V) was almost the double compared to uncomplicated group, but AMC was minimum among other diabetic complications. DR (Gp II) had higher expenses compared to DNeu (Group V) (Table 4). The similar pattern of distribution was observed in other individual costs.
It is evident from our study that direct health-care costs for treating diabetes and its complications are on the rise. The study revealed that the average cost of treating and managing diabetes-related IHD complications (Group VI) was the highest among all other complications. AMC was 7.2 times higher as compared to that in uncomplicated Group I. This increase in AMC is due to corresponding rise in laboratory charges (5.4 times), pharmacy charges (9.4 times), consultation charges (3.1 times), and hospital bed charges (4 times) due to probable increase in frequency and duration of admissions, higher surgical/intervention charges (7.4 times).
The maximum contribution is from medical appointments, tests, outpatient catheterization procedures, medications in use, and transport of the patient to the hospital, etc. In addition to hypoglycemic drugs, cardiologist’s prescriptions might contribute significantly to APC. We assumed that the drugs were purchased by the patients at pharmacies using their own resources without government subsidies and were taken with 100% treatment adherence. Additional laboratory tests to monitor cardiac functions and lipid profiles contributed to ALC. Cardiac and imaging tests included were myocardial scintigraphy (stress and resting), Echocardiography (stress and resting) exercise test, Holter, Ambulatory Blood Pressure Monitoring (ABPM), chest X-ray, carotid and vertebral Doppler echocardiography, venous colour Doppler, echocardiography, and chest tomography make major contribution to investigations. Hospital treatment consists of hospitalization days, Intensive Care Unit days, laboratory and diagnostic tests, angioplasty procedures with or without stent implantation, cardiac catheterization, and coronary artery bypass surgery performed during hospitalization made a huge contribution to ASC or intervention costs. Our results are supported by a recent Brazilian study by Schlatter et al., which showed that the direct costs of longitudinal IHD treatment were high and were primarily driven by chronic pharmacological treatment and days of hospitalization and interventions [15].
DN (Group III) was the second highest expensive complication of diabetes. AMC, ALC, APC, ACC, AHBC, and ASC were higher by 4.6, 3.3, 5.9, 3.4, 2.7, and 4.6 times, respectively, compared to uncomplicated group. Higher cost incurred might be due to frequent investigations, consultations, and drugs. A recent study by Jose et al., focused on pharmacoeconomic aspects of DN from India, reported that monthly cost of dialysis contributed most (37%) to the total cost in DN patients [16]. An earlier study from India reported that cost per dialysis in India ranged from INR 150 in government hospitals to INR 2000 in private hospitals [17]. In most of the private hospitals, the average cost of dialysis per patient per month was INR 12,000 and the yearly cost is INR 140,000 equivalent of USD 3000, and this is in sharp contrast to the annual cost of USD 60,000 in the United States and the United Kingdom. In the study by Jose et al., monthly average cost of dialysis per patient was INR 9060 [16]. The patients on an average underwent eight dialysis sessions per month in the study which was comparable with a study by Satyavani et al. done in a South Indian state [18]. This was not affordable to many patients as around 89% belonged to lower to middle-class socioeconomic strata in the study [16]. In a study by Satyavani et al., the cost for a person on haemodialysis was 4 times higher than for persons with chronic kidney disease (CKD) only (INR 61,170 vs. 12,664) [18]. A study by O’Brien et al. in Canada showed that early stage complications (e.g., microalbuminuria: USD 62 event cost; USD 10 state cost) had relatively low financial burden compared to more costly advanced stages (e.g., end-stage renal disease [ESRD], USD 63,045 state cost) [19]. Kidney transplantation remains the most cost-effective treatment for ESRD, offering considerable savings and improvement in the quality of life in these patientsas shown in a study by Satyavani et al. [18,20]. The total median cost of treatment of diabetic patients with ESRD was very high (on average INR 500,000) compared with transplant patient (INR 3,45,000) over a period of 2 years, whereas the average cost of treatment of diabetes with and without CKD was INR 100,000 and INR 30,000, respectively [21]. Strict glycemic and blood pressure control can reduce the incidence and slow the progression of DN [22]. Improvement in diabetes control, early diagnosis of DN, and treatment has the potential to reduce the direct cost involved in treatment of DN [21].
Our results are supported by the study by Kumpatla et al. who reported that total expenditure for treating renal, cardiovascular, and retinal complications was more or less similar among type 2 diabetic patients [10]. Satyavani et al. studied the direct cost of treating CKD in type 2 diabetic patients in India. The authors assessed the comparative cost of treatment of diabetic patients without CKD, those with Stage 1-4 CKD, who needs dialysis, and those with kidney transplantation [18]. They determined cost of treatment at two levels: Cost of hospitalization and total cost of treatment over the previous 2 years taking into account costs of hospitalization, consultation, medication, laboratory tests, dialysis treatment, transplantation surgery, and transportation. Ramachandran and Jha demonstrated that even kidney transplantation, the most cost-effective form of renal replacement therapy, in a public sector hospital can have catastrophic financial consequences pushing the majority of families into severe poverty [23].
DKD is preventable. There is substantial evidence that early and effective therapeutic intervention in Type 2 Diabetes can prevent DKD and retard the progression of established DKD.
DF (Group IV) was the next costliest complication. AMC, ALC, APC, ACC, AHBC, and ASC were higher by 4, 3.5, 6.1, 3.6, 2.8, and 4.8 times compared to uncomplicated group. Some studies have shown 15% of diabetic patients will be suffering from DF ulcer during their lifetime [24]. DF ulcer is the most general cause of hospitalization in diabetic patients [25]. Lower extremity amputation is associated with prolonged hospitalization and rehabilitation and also required home care and social support which contribute to the economic burden [26]. It should be considered that the burden of DFrelated neuropathy is two folds than the burden of DR or nephropathy currently. 85% of DF amputations are preventable with appropriate care and education. Ideal management for prevention and treatment of DF is as follow: Regular perception of foot, determine at-risk foot, education to patient and health staff, appropriate foot coverage, and early treatment of foot problems [27].
DR (Group II) was in fourth place to contribute to the health-care cost among the complications of DM. AMC, ALC, APC, ACC, AHBC, and ASC were 2.3, 2, 3.4, 2.4, 1.4, and 2.3 times, respectively, higher compared to uncomplicated group. The increased cost could be attributed to screening, retinography, treatment costs, antivascular endothelial growth factor drugs, etc. There are hardly many studies done in this area in Indian settings. Average health-care costs increased considerably with the severity of retinopathy, which suggests that preventing progression of DR may lower health-care cost.
DNeu (Group V) had minimum expenses among the complications of diabetes, but AMC, ALC, APC, ACC, AHBC, and ASC of this group were 2, 1.6, 2.6, 1.9, 1.1, and 1.9 times higher, respectively, than those in uncomplicated group.
As expected, the group without any complications had reduced cost pattern for all the parameters, which is evident that high costs for diabetes care are not just due to the disease but due to its associated complications. Our reports are supported by a recent study by Leelavathi et al. carried out in the same geographical area [28]. According to the study, average cost per diabetic patients without complications is Rs. 917.73 compared to the diabetic patients with complications Rs. 1448.51 per month. Annual cost of medication was found to be 1.6 times higher for diabetes with complication compared to those without complications. Cost-of-illness (COI) for DM with complication was reported to be 1.4 times higher than those without complications. Those patients who undergo dialysis in addition to the complications spend 7.3 times higher than those without complications. Patients who undergo cardiology intervention along with complications spend 7.4 times higher than patients who do not have complications. It also reports that hospitalization charge was 1.2 times higher for DM with complications. As per this study, cost per DM patient on dialysis (usually 2 times per week) is Rs. 97,920.00 per annum. Cost per diabetic patient undergoing cardiac intervention is Rs. 72,120.00 per intervention. It showed that annual cost of treatment for those who were on dialysis was 6.8 times higher and annual cost of treatment for cardiac intervention was 5 times higher than patients who did not have any intervention. Moreover, there may not be much difference in the cost of investigations, consultation cost, transportation, and indirect cost involved in diabetic care. They found that total COI for diabetic care without any complication was Rs. 22,456.97/- per patient per annum. Median of total COI for diabetic care with complication was Rs. 30,634.45/- per patient per annum, it was 1.4 times higher, median of COI for diabetic care with complication plus dialysis was Rs. 164,211.40/- per patient per annum, it is 7.3 times higher and the median COI for diabetic care with complication plus cardiac intervention was Rs. 166,785.85/- per patient per annum which is 7.4 times higher and statistically significant difference observed between these groups. A similar study conducted by Metgud showed that cost of outpatient care for diabetic patient with chronic renal failure (CRF) requiring dialysis was 15 times higher than the cost of outpatient care for a diabetic patient without CRF (excluding dialysis cost) [29].
Compared to our study, costs mentioned in the above study were more. We cannot arrive at any conclusion by comparing numbers, as the costs are different in different settings. Even though cost variations exist, in general, we can conclude that diabetes poses economic burden which is amplified several times when associated complications.
The studies have reported the cost of managing diabetic patients with or without microvascular and macrovascular complications. Patients with microvascular complications had higher the cost of management, and those with macrovasular complications had even higher cost of management. Difference in the cost and proportions in different studies may be due to the period of study, place, method of collecting the data, and economic values. However, all the studies have concluded that diabetes is diseases associated with significant economic burden and diabetes complication make it more expensive. It is not only a burden to the patient, his family but also to the nation.
Our results support well-established fact that complications get worsen with longer duration of diabetes. Our study is in accordance with a report by Leelavathi et al. [28]. According to this study, regarding the duration of diabetes in the study population, 60.8% diabetic patients in without complication group had <5 years of history of diabetes, whereas in diabetes with complication group, 64.6% of diabetic patients had above 5 years of history of disease.
The total expenditure correlated significantly with age and duration of diabetes. The expenditure involved in treating long-term complications was significantly associated with duration of diabetes and presence of complications in the current study.
The duration of stay in the hospital, number of visits made for postsurgical dressings, hospital charges, laboratory charges, and medical consultations are the factors which significantly contribute to the increased cost in DF. The duration of hospital stay which is substantially longer in patients with foot complications increase the cost. Such information on hospital stay days and costs may help to emphasize earlier intervention and prevention of complications of diabetes.
The cost of diabetes can be a major burden as the disease does not have cure, and its complications increase with increasing duration of the disease. This was seen in a study by Chandra et al., a positive correlation of increasing cost with duration of diabetes [30].
Factors such as education and socioeconomic condition of the patient do contribute the cost in case of diabetes. It has been documented that urban people spend more money on diabetes compared to rural counterpart not only due to better awareness but also due to greater affordability [31].
A study by Hussain et al. suggested that the requirement of resources could be minimized by better care, treatment, and understanding of the disease [32]. Anandayani et al. suggested that intensified glycemic control is important in reducing complications and also to improve the quality of life in diabetic patients [33].
On comparison of data of 2008-09 with that of 2016- 2017, it was observed that AMC raised by 2.22 times, ALC 2.68 times, ACC 1.42 times and ASC raised by 2.17 times over 8 years of duration. On the contrary, a lowered APC by 0.95 times and AHBC declined by 50% (Figure 3).The percentage of cost incurred varied in different groups based on the severity of complication, duration of illness, status of their glycemic control. Difference in costs observed in 2008 and 2017-18, may be due to progression of disease and complications, change in economy, inflation etc. Higher ASC suggests a more number of patients developing complications and required interventions. Increased ACC suggests probable referrals and consultations of different speciality consultants. Higher APC observed in the previous study could be due to additional costs of drugs used in the treatment of associated co-morbidities in addition to anti diabetic drugs. Higher AHBC in the past decade could be due to confounding factors. Patients admitted to general, semi special, special, deluxe and super deluxe rooms in to consideration. Probably higher AHBC observed in 2008, might be due to inclusion of more number of special and deluxe room patients. Lower APC in 2017 could be due to lowered drug costs because of emerging new companies and their competition.
On comparing various costs incurred in diabetics in 2008 and 2017, annual surgical/intervention cost as well as lab charges were more than doubled (31% to 65% and 6% to 14% respectively) over 8 years. This fact could be attributed to the faster progression of disease demanding more investigations and interventions.
We have witnessed a decrease in annual cost spent in hospital beds and pharmacy in our study in as well as money spent by the patient in uncomplicated diabetes in 2017. Since majority of the patients were having subsidized health facility, the consultation fee, hospital bed charges and pharmacy cost (generic drugs), there was no change or reduction in annual cost spent by the patient during 2017.
The novel treatments can lead to increase longevity of diabetic patients and the risk of chronic complications such as eye involvement, renal, cardiovascular and diabetic foot and also cause to impose heavy economic burden on the health system [34].
People with diagnosed diabetes, on average, have medical expenditures approximately 2.3 times higher than what expenditures would be in the absence of diabetes in developed countries like U.S [35]. Purchase of medicines was the chief economic burden accounting for almost half the direct expense of the disease followed by surgical (12.6%) and Lasers treatment (3.2%).The clamour for generic drugs that would greatly reduce the cost of medicines is serious and rightful issue and would greatly reduce the economic burden of this disease, especially in lower middle class and poor patients [36].In this study, of the average direct cost, only 10.4% was spent on doctor’s consultation fees.
Diabetic patients should be educated that if they have regular check-ups the cost of managing their disease shall be less, not more, as their diseases would have fewer complications. Mohan et al. found that only 75% of residents in Chennai knew of diabetes [37]. Only 22% were aware that it was preventable, while only 12% knew of its risk factors. Even in known diabetics, only 40.6% were aware of its complications. The medical fraternity, pharmaceutical industry and the governments need to increase awareness regarding the cause, preventable nature and potential complications of diabetes. Only proper health education would ensure that people take the disease seriously and ensure strict control by regular check-ups.
Diabetes unlike common cold, typhoid, accidents, broken bones or cataracts is not a one-time disease but one is the lifelong companion to the patient. Unless patients do not understand the cause and the risks of the diseases and its complication, good control is difficult and poor control associated with spiralling cost. On comparison of data of 2008-09 with that of 2017,it was observed that AMC raised by 2.22 times, ALC 2.68 times, ACC 1.42 times and ASC raised by 2.17 times over 8 years of duration. On the contrary, APC was lowered by 0.95 times and AHBC declined by 50% (Figure 3). Figures 4 and 5 depict total direct costs in various complications and percentage contribution of different costs to direct medical cost in T2DM. The increased health care cost could be attributed to the disease progression as well as lack of awareness about importance of regular check-ups, screening for complications among patients.
Despite several advances in the field of diabetology, it is unfortunate that there exists a low awareness of the disease among public. This explains the findings of a recent study, which has shown that for every one person known to have diabetes, there are more than two people who have undiagnosed diabetes. This means that a substantial proportion of people with diabetes may already have developed at least one diabetic complication by the time they are diagnosed. It has been demonstrated that in type-1 diabetes, early detection of nephropathy by screening for micro albuminuria and immediate recourse to improved control with anti-hypertensive medications, not only increases life expectancy significantly but also concomitantly reduces total health care costs [38]. An intensive education program can improve the foot care knowledge and behaviour of high-risk patients [39,40].
Early detection and appropriate treatment are the cornerstones for delaying the onset and progression of the diabetic complications viz. retinopathy, nephropathy, neuropathy, stroke, peripheral vascular disease and ischemic heart disease. Meta-analyses and reviews of the diabetes literature have shown that diabetes education, awareness and improving motivation for self-care improves care, reduces complications and may thus reduce overall economic costs of diabetes [41,42].
Limitations of the Study
There are a few limitations in our study design. It is important to note that the data collected is from medical college teaching hospitals and the generalizability of results may be limited to certain private healthcare centres, the projected cost estimates were mainly based on urban patients whose pattern of disease may be different compared to rural patients. We could not assess the indirect cost and the cost of care for structured and comprehensive assessment of disability in this study. Educational and other socioeconomic details of patients could not be accessed as it was a hospital based study.
Conclusion
• Diabetes mellitus is a costly disease which imposes an economic burden.
• The total annual medical costs are significantly higher in complicated diabetics as compared to those without complications.
• Diabetics with ischemic heart disease had the highest expenses, followed by diabetic nephropathy,diabetic foot,diabetic retinopathy and diabetic neuropathy which was least expensive.
• There was a paradigm shift (increase in direct costs like annual medical cost. laboratory cost, consultation cost. surgical costs over a decade.
• Positive correlation between duration of diabetes and cost incurred and negative correlation of glycemic control and cost incurred, suggest a need for strategies that aim at reducing the escalating cost burden by achieving targeted glycemic control, prompt and effective management of complications, operationalize regular and early screening for complications.
• Awareness creation on primary and secondary prevention of diabetes and its complications is the need of the hour, alongside capacity strengthening of medical and paramedical professionals involved in diabetes care.
References
- Diabetes: The Cost of Diabetes, Fact Sheet No. 236. World Health Organization 2002.
- Shobhana R, Rao PR, Lavanya A, Williams R, Vijay V, Ramachandran A. Expenditure on health care incurred by diabetic subjects in a developing country? A study from southern India. Diabetes Res Clin Pract 2000; 48: 37-42.
- Shobhana R, Rao PR, Lavanya A, Williams R, Padma C, Vijay V. Costs incurred by families having Type 1 diabetes in a developing country - A study from Southern India. Diabetes Res Clin Pract 2002; 55: 45-48.
- Rao KD, Bhatnagar A, Murphy A. Socio-economic inequalities in the financing of cardiovascular and diabetes inpatient treatment in India. Indian J Med Res 2011; 133: 57-63.
- Grover S, Avasthi A, Bhansali A, Chakrabarti S, Kulhara P. Cost of ambulatory care of diabetes mellitus: A study from north India. Postgrad Med J 2005; 81: 391-395.
- Kumar A, Nagpal J, Bhartia A. Direct cost of ambulatory care of Type 2 diabetes in the middle and high income group populace of Delhi: The DEDICOM survey. J Assoc Physicians India 2008; 56: 667-674.
- Ramachandran A, Ramachandran S, Snehalatha C, Augustine C, Murugesan N, Viswanathan V. Increasing expenditure on health care incurred by diabetic subjects in a developing country: A study from India. Diabetes Care 2007; 30: 252-256.
- Shivaprakash G, Nishith RS, Basu A, Pallavi S, Adhikari P, Gopalakrishna HN. Dispensing patterns and cost of glucose lowering therapies in diabetes mellitus patients at a tertiary care hospital in Southern India. Drug Invent Today 2012; 4: 671-673.
- Adiga S, Adiga U. Health care cost incurred by patients of diabetes mellitus in a tertiary care hospital setting in coastal Karnataka district. J Glob Pharm Technol 2010; 2: 8-12.
- Kumpatla S, Kothandan H, Tharkar S, Vishwanathan V. The costs of treating long term diabetic complications in a developing country: A study from India. J Assoc Physicians India 2013; 61: 102-109.
- Kuchake V, Kumbhar P, Dighore P, Patil P. Comparison of lipid profile pattern in obese and non-obese Type 2 diabetic patients and to study the prescription pattern of ant diabetic drugs. Int J Pharm Sci Rev Res 2010; 4: 53-58.
- Joshi A, Mohan K, Grin G, Perin DM. Burden of healthcare utilization and out-of-pocket costs among individuals with NCDs in an Indian setting. J Community Health 2013; 38: 320-327.
- Akari S, Mateti UV, Kunduru BR. Health-care cost of diabetes in South India: A cost of illness study. J Res Pharm Pract 2013; 2: 114-117.
- Abdi AH, Churi S, Kumar YS. Study of drug utilization pattern of antihyperglycemic agents in a South Indian tertiary care teaching hospital. Indian J Pharmacol 2012; 44: 210-214.
- Schlatter RP, Hirakata VN, Polanczyk CA. Estimating the direct costs of ischemic heart disease: Evidence from a teaching hospital in BRAZIL, a retrospective cohort study. BMC Cardiovasc Disord 2017; 17: 180.
- Jose JV, Jose M, Devi P, Satish R. Pharmacoeconomic evaluation of diabetic nephropathic patients attending nephrology department in a tertiary care hospital. J Postgrad Med 2017; 63: 24-28.
- Khanna U. The economics of dialysis in India. Indian J Nephrol 2009; 19: 1-4.
- Satyavani K, Kothandan H, Jayaraman M, Viswanathan V. Direct costs associated with chronic kidney disease among Type 2 diabetic patients in India. Indian J Nephrol 2014; 24: 141-147.
- O’Brien JA, Patrick AR, Caro JJ. Cost of managing complications resulting from Type 2 diabetes mellitus in Canada. BMC Health Serv Res 2003; 3: 7.
- Karlberg I, Nyberg G. Cost-effectiveness studies of renal transplantation. Int J Technol Assess Health Care 1995; 11: 611-622.
- Olivera EM, Duhalde EP, Gagliardino JJ. Costs of temporary and permanent disability induced by diabetes. Diabetes Care 1991; 14: 593-596.
- Zoungas S, de Galan BE, Ninomiya T, Grobbee D, Hamet P, Heller S. Combined effects of routine blood pressure lowering and intensive glucose control on macrovascular and microvascular outcomes in patients with Type 2 diabetes: New results from the advance trial. Diabetes Care 2009; 32: 2068-2074.
- Ramachandran R, Jha V. Kidney transplantation is associated with catastrophic out of pocket expenditure in India. PLoS One 2013; 8: e67812.
- Reiber GE, Lipsky BA, Gibbons GW. The burden of diabetic foot ulcers. Am J Surg 1998; 176: S5-S10.
- Lobmann R. Diabetic foot syndrome. Internist (Berl) 2011; 52: 539-548.
- Bakker K, Riley PH. The year of the diabetic foot. Diabetes Voice 2005; 50: 11-14.
- International Working Group on the Diabetic Foot: International Diabetes Federation Report: In