ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 21
64-Slice spiral CT angiography study of bronchial artery imaging characteristics and its clinical value in patients with lung cancer
1Yantaishan Hospital, Yantai, Shandong, China
2Yantai Infectious Disease Hospital, Yantai, Shandong, China
3Jining No.1 People’s Hospital, Jining, Shandong, China
#These authors contributed equally to this work
Accepted date: November 07, 2017
Objective: To study the characteristics and clinical value of Bronchial Artery (BA) imaging in patients with lung cancer by 64-slice spiral CT angiography (CTA).
Methods: The data of 67 patients who were diagnosed as primary lung cancer and 67 healthy persons in the same period were selected from July 2016 to July 2017. The primary lung cancer patients were grouped into the study group, and the healthy persons were classified as the control group. CT scan was performed on the two groups, respectively, for the characteristics observation records and value analysis.
Results: The display number of left and right BA cases in the study group was more than that in the control group, and the total display number of AB was more in the study group. The diameter of the ipsilateral BA in the left lung cancer was larger than that in the control group. The diameter of the ipsilateral BA in the right lung cancer was larger than that in the control group. The BA diameter of the affected side in the lung cancer group was larger than that of the healthy side. The BA manifestations of primary lung cancer were interlaced, tortuous and intermittent, and the associated pulmonary artery was wrapped around, with a residual root shape, narrowing by invasion or truncation.
Conclusion: The application of 64-slice spiral CT in the detection of primary lung cancer can provide more clear and comprehensive diagnostic data for patients.
Keywords
CT, Vascular imaging, Lung cancer, Bronchial artery, Imaging characteristics.
Introduction
Primary lung cancer is one of the most common malignant tumors, with more dangerous conditions, high incidence, and mostly poor prognosis, which makes it become a serious threat to human health and disease [1]. For a long time, there is still controversy about whether pulmonary artery is involved in lung cancer blood supply, which can be summarized into the following 3 representative viewpoints: pulmonary artery is the main blood supply artery of lung cancer, pulmonary artery participates in blood supply of primary lung cancer, and only systemic circulation predominated by Bronchial Artery (BA) is involved in blood supply of primary lung cancer, and the pulmonary artery is not involved in blood supply. At present, most scholars [2] support the 3rd view. The author and many other scholars think that the reason for the problem of blood supply of lung cancer is that there is still a lack of uniform and accepted criteria for the determination of the blood supply arteries of lung cancer, and there are some aspects needing further rigorous research in the conclusion of pulmonary artery involvement in the blood supply of lung cancer. With the advancement of medicine, 64-slice spiral CT Angiography (CTA) is being widely used in the detection of BA in lung cancer patients [3]. The purpose of this study was to analyse the characteristics and clinical value of CTA in detecting Bronchial Artery (BA) imaging in patients with primary lung cancer.
Materials and Methods
General materials
The data of 67 cases of patients admitted in our hospital and diagnosed as primary lung cancer from July 2016 to July 2017 and 67 healthy persons in the same period were selected. The primary lung cancer patients were included in the study group, and the healthy persons were included in the control group. 40 males and 27 females were included in the study group, and they were aged 52-88 y old, at an average age of 65.59 ± 4.36, weight 50-80 kg, at an average weight of 26.72 ± 3.68 kg. 38 males and 29 females were included in the control group, and they were aged 50-87 y old, at a mean age of 64.16 ± 4.03, weighted 49-81 kg, at a mean weight of 50.15 ± 3.22 kg; there was no statistically significant baseline data between the two groups (P>0.05).
Methods
The scanning instrument is the US GE 64-slice light speed spiral CT scanner, scanning range: From 2-3 cm above the thoracic entrance to the lung bottom. The scanning parameters were set as follows: The conventional thickness was 5mm, its reformation thickness was 0.625 mm, its pitch was 0.984:1, FOV (Field of View) was 50 cm, the tube voltage was 120 kV, the current was 250 mAs, and the contrast agent was 75 ml of the Non-ionic contrast agent Youwei. The high-pressure type syringe was used, and the injection speed was controlled at 3.5 ml/s. The sweep time was 10 s, and the delay was 30 s. The scanned images were reconstructed by thin slices for VR (Volume Reconstruction), MIP (Maximum Density Projection), MPR (Multiplanar Reconstruction), etc., and then the treatment of BA and pulmonary artery was carried out, and the examination results were analysed and observed by multi-angle rotation and cutting.
Observation index
The morphological characteristics of primary lung cancer tumors in the blood supply arteries were observed and recorded. An artery that starts from systemic circulation, through the root of porta pulmonis to lung bronchus was determined as a BA. Each BA was identified as one BA after entering the root of porta pulmonis. BA diameter evaluation: Dilation with the transverse diameter of more than 2 mm.
Statistical analysis
The SPSS20.0 statistical software was used for analysis, and the measurement data was expressed as mean ± standard deviation. T-test was used in the comparison between groups. The number of cases was used as the count data, Chi-square was used in the group ratio comparison, and paired comparison was used for the ipsilateral BA diameters. All data first underwent normality and variance homogeneity analysis. Then, the T test was used for the data that satisfied the conditions, and the Mann-Whitney-U test was used for the data that did not satisfy the conditions. T-Test or Mann-Whitney-U test of lung cancer affected BA diameter and contralateral BA diameter, P<0.05 is statistically significant for difference.
Results
Display of lung cancer in the BA
The display number of cases in left and right BA in the study group was more than that in the control group, and the total display number of cases in AB was more in the study group (Table 1).
| Group | Number of cases | Display number of total cases | Display number of right BA cases | Display number of left BA cases |
|---|---|---|---|---|
| Control group | 67 | 50 (74.63) | 40 (59.70) | 31 (46.27) |
| Study group | 67 | 63 (94.03) | 22 (32.84) | 13 (19.40) |
| χ2 | 9.54 | 9.72 | 10.96 | |
| p | 0.002 | 0.002 | 0.001 |
Table 1: Comparison of postoperative rehabilitation of patients between two groups.
Changes of BA diameter in lung cancer
Comparison of the lung cancer group with the control group: The diameter of the ipsilateral BA in the left lung with cancer was larger than that in the control group. The diameter of the ipsilateral BA in the right lung with cancer was also larger than that in the control group.
Comparison of diameters of affected and healthy side BAs in the lung cancer group: The BA diameter of the affected side in the lung cancer group was larger than that of the healthy side in the lung cancer group (Table 2).
| Class | Right BA | Left BA |
|---|---|---|
| Control group | 1.30 ± 0.41 | 1.20 ± 0.11 |
| Right lung cancer in the study group | 2.67 ± 0.63 | 2.05 ± 0.30 |
| Left lung cancer in the study group | 2.01 ± 0.52 | 2.37 ± 0.43 |
Table 2: Changes of BA diameters in lung cancer.
Characteristics of blood-supply BA in the CTA in patients with lung cancer
The BA manifestations of primary lung cancer were interlaced, tortuous and intermittent, and the associated pulmonary artery was wrapped around, with a residual root shape, narrowing by invasion or truncation. The BA in the control group showed that the right BA went to the right wall of the aorta from the T5 horizontally, with a BA diameter of about 1.38 mm. In the study group, 63 cases of BA were displayed clearly, and 46 cases of them could clearly show the cross of the lump in BA and the formation of tumor vessels.
CTA imaging characteristics of typical cases
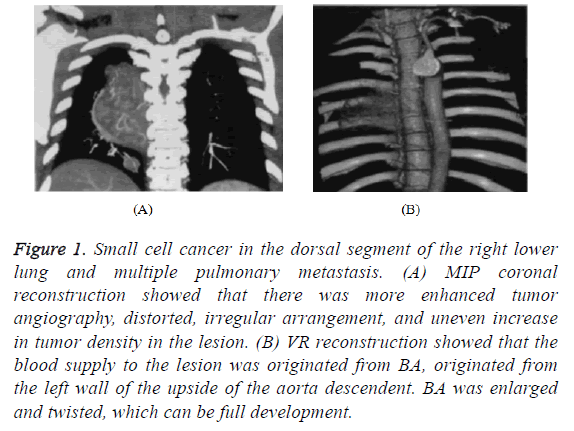
A patient, female, small cell cancer in the dorsal segment of the right lower lung and multiple pulmonary metastasis (Figure 1).
Figure 1: Small cell cancer in the dorsal segment of the right lower lung and multiple pulmonary metastasis. (A) MIP coronal reconstruction showed that there was more enhanced tumor angiography, distorted, irregular arrangement, and uneven increase in tumor density in the lesion. (B) VR reconstruction showed that the blood supply to the lesion was originated from BA, originated from the left wall of the upside of the aorta descendent. BA was enlarged and twisted, which can be full development.
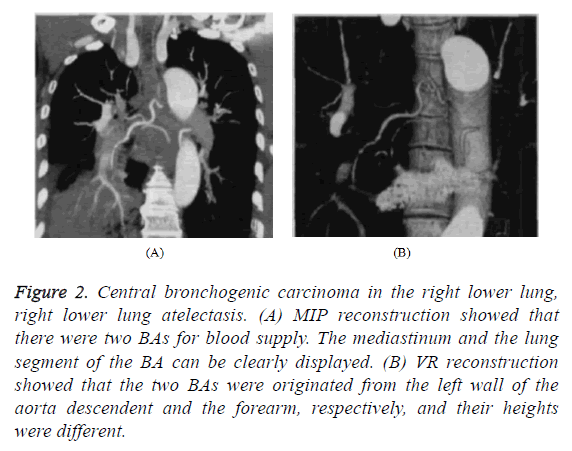
Another patient, male, central bronchogenic carcinoma in the right lower lung, right lower lung atelectasis (Figure 2).
Figure 2: Central bronchogenic carcinoma in the right lower lung, right lower lung atelectasis. (A) MIP reconstruction showed that there were two BAs for blood supply. The mediastinum and the lung segment of the BA can be clearly displayed. (B) VR reconstruction showed that the two BAs were originated from the left wall of the aorta descendent and the forearm, respectively, and their heights were different.
Discussion
As time goes by, the incidence of lung cancer in China is gradually increasing, and now the incidence of lung cancer in men accounted for the main part, and in women, it is also increasing, causing serious economic burden on people as well as serious threat to the health of patients [4,5]. Therefore, the implementation of its early diagnosis and treatment is significant for patients, and diagnostic tools in the inspection play an important role. With the continuous progress of medical imaging, the main tools for examination of lung cancer are CY ray, X-ray, MRI, etc. MRI is a multi-plane to show the structure of the mediastinal anatomy, but its specificity is relatively low, and it is expensive; X-ray is the most commonly used diagnostic tool for lung cancer examination, but the misdiagnosis rate is relatively high; CT is a noninvasive examination of the highest value in the diagnosis and staging of lung cancer [6-10].
In this study, the display number of cases in the left and right BA of the study group was higher than that in the control group, and the total display number of AB was more in the study group. The display rate of AB was 94.03% (63/67) in the study group, which was higher than the control group (74.63%) (50/67). The results were similar with that of Chen [11]. The reason for this is that the concentration and amount of contrast agent will affect the display quality of the image. In this study, the traditional fixed-time scanning method was used. The delayed sweeping time was 30s, and the CT value in the BA beginning part reached 300 Hu or so, of which 67 cases, only 4 cases were not shown. According to the study, both the BA diameter of the right lung and that of the left lung in the study group were larger than that in the control group. The BA diameter of the right lung was 2.67 ± 0.63 mm in the study group, larger than that in the control group. The results were similar with that of Gao et al. [12]. The reason for this is that the injection rate of contrast agent was set to 3.5 ml/s in this study, and hence the size of BA diameter was similar with that of related literature. Meanwhile, the influence factors of the other aspects on the imaging were the individual aspects of the patients, including nervousness, cough, and involuntary movement of breathing. Therefore, there were artifacts from heart movement, contrast agent in the superior vena cava and contrast agent in the adjacent pulmonary artery; there was a correlation with the concentration of contrast agents. This study used 300 mg/ml concentration of non-ionic contrast agent, which could clearly show BA small blood vessels. In the CAT image processing technology, continuous observations were made to the axial thin slice images of the BAs. First, the origins of BA openings were found. As BA blood vessels were slim, whose diameters were about 2 mm. Therefore, the axial thin slice images of the BAs in the lung segment and mediastinum were not clear. However, after post-processing of the images by real-time VR, MPR and MIP, the whole view of the blood vessels can be observed from any angle of view. When the BA diameter was measured in this study, it is found that the related BAs will be significantly larger, and the branches will increase when the lung cancer occurs. The main manifestations of tumor blood vessels were blood paste, reticular, spotted and earthworm-like staining. The blood vessels were not tapering from near to far, but their sizes varied greatly. The distal ends of the blood vessels were relatively larger than the proximal ends when observed in a certain range, which was opposite to the normal blood vessels. At present, some scholars [13-15] consider that BA is the main blood supply artery of lung cancer. Therefore, the preoperative imaging of BA in the CTA can provide important information for patients to receive more targeted treatment. In this way, the use of radiation dose is substantially reduced; meanwhile, the operation time can be shortened, and the success rate of BA intubation can be comprehensively increased. The number of samples taken from this study was limited, and the results were further studied.
In summary, the 64-slice spiral CT angiography can provide clear morphological characteristics of BAs that supply blood for lung cancer and provide reliable information for early treatment of patients.
References
- Tang X, Li Z. The value of Spiral CT angiography in the treatment of lung lobectomy. Chinese J CT MRI 2016; 14: 40-42.
- Fang Y, Xie W, Sha Z. Preoperative evaluation of computer imaging angiography and digital subtraction angiography on non-small cell lung cancer. J Clinic Med Pract 2016; 20: 22-28.
- Qiao Y, Dai R. The value of spiral CT in the clinical diagnosis of peripheral lung cancer. Chinese J CT MRI 2017; 15: 64-66.
- Li BG, Ma DQ, Xian ZY. The value of multislice spiral CT features of cavitary walls in differentiating between peripheral lung cancer cavities and single pulmonary tuberculous thick-walled cavities. Br J Radiol 2012; 85: 147-152.
- Vernhet H, Dogas G, Bousquet C. Value of thoracic CT in the management of severe hemoptysis. J De Radiologie 2003; 84: 685-691.
- Lu G, Wang Z, Zhu H. The advantage of PET and CT integration in examination of lung tumors. Int J Biomed Imag 2007; 2007: 17131.
- Jayaprakash V, Loewen GM, Dhillon SS. Early detection of lung cancer using CT scan and bronchoscopy in a high-risk population. J Cancer Ther 2012; 3: 388-396.
- Vansteenkiste J, Crino L, Dooms C. 2nd ESMO Consensus Conference on Lung Cancer: early-stage non-small-cell lung cancer consensus on diagnosis, treatment and follow-up. Ann Oncol Off J Eur Soc Med Oncol 2014; 25: 1462-1474.
- Turner MO, Mayo JR, Muller NL. The value of thoracic computed tomography scans in clinical diagnosis: a prospective study. Canadian Resp J 2006; 13: 311-316.
- Rinaldi MF, Bartalenaa T, Rinaldi G. Incidental lung nodules on CT examinations of the abdomen: Prevalence and reporting rates in the PACS era. Eur J Radiol 2010; 74: 84-88.
- Felix SY. Formulation and in-vitro evaluation of floating microbaloons of stavudine. Univ J Pharm Res 2016; 1: 13-17.
- Gao Y, Wang J, Zhou X. Multislice spiral CT analysis of peripheral lung cancer morphological features-MPR orthogonal reformation combined with MIP. J Sun Yat-sen Univ Med Sci 2016; 37: 925-929.
- Zhiyong LI, Dong Y, Jianlin WU. Three-dimensional imaging of multi-slice spiral CT in bronchial artery correlative study on blood supply of central lung cancer and its clinical significance. Chinese-German J Clin Oncol 2005; 4: 40-42.
- Zhao LX, Gao Q, Liu YJ. Study on 256-slice spiral CT bronchial artery imaging of common pathological types of central-type lung cancer. Eur Rev Med Pharmacol Sci 2016; 20: 3211-3216.
- Lv Y, Jin Y, Yan Q. The value of 64-slice spiral CT perfusion imaging in the treatment of liver cancer with argon-helium cryoablation. Oncol Lett 2016; 12: 4584-4588.