ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2010) Volume 21, Issue 4
A prevalence of thyroid dysfunction in Kathmandu University Hospital, Nepal
1Department of Biochemistry, Kathmandu University School of Medical Sciences/ Dhulikhel Hospital-Kathmandu University Hospital, Dhulikhel, Kavre, Nepal.
2Laboratory of Genetics, Department of Microbiology and Immunology, Institute for Medical Science, Chonbuk National University Medical School, Chonju, Chonbuk 561-756, South Korea.
- *Corresponding Author:
- Madhukar Aryal
Department of Biochemistry
Kathmandu University School of Medical Sciences
Dhulikhel, Kavre,
Nepal
E-mail: madhukararyal@kusms.ku.edu.np
Thyroid dysfunction is one of the most commonly encountered endocrine abnormalities. The screening of thyroid dysfunction is recommended in Nepal with its high risk population. Many factors are responsible for exacerbating the thyroid dysfunction in the context of Ne-pal. Therefore, this study was designed to assess the prevalence of thyroid dysfunction in Dhulikhel Hospital-Kathmandu University Hospital (DH-KUH). In this hospital based retro-spective study, 825 subjects (resident of Kavre) that were subjected to thyroid function test panel (free tri-iodothyronine, free thyroxine and thyroid stimulating hormone) were enrolled and the thyroid dysfunction was stratified as hypothyroidism, subclinical hypothyroidism, hyperthyroidism, subclinical hyperthyroidism with reference to hormonal levels. Among 825 subjects, the prevalence of thyroid dysfunction was 25%. Females had more thyroid dysfunc-tion than males. Hypothyroidism (8%) and subclinical hypothyroidism (8%) had higher prevalence compared to subclinical hyperthyroidism (6%) and hyperthyroidism (3%). Higher prevalence of thyroid dysfunction was observed in subjects with age above 30 years. In conclusion, this study revealed the higher prevalence of abnormal thyroid function and concurs with previous reports in other populations. Hypothyroidism and subclinical hypo-thyroidism are preponderant followed by subclinical hyperthyroidism. Females and ad-vanced aged people are more vulnerable to thyroid dysfunction in the population. Since, it was a hospital-based study; the prevalence of thyroid dysfunction may not be applicable to the general population. Extensive field-based countrywide epidemiological studies are neces-sary to provide accurate data about thyroid dysfunction in the community.
Keywords
Thyroid hormones, Thyroid dysfunction, Hypothyroidism, Hyperthyroidism, Nepal
Introduction
Thyroid dysfunction is defined as the altered serum thy-roid stimulation hormone (TSH) level with normal or al-tered thyroid hormones (free tri-iodothyronine- fT3 and free thyroxine- fT4). Thyroid dysfunction is a common endocrine disorder affecting about 300 million people worldwide and over half are presumed to be unaware of their condition [1]. Thyroid dysfunction is also a major health problem of Nepal with prevalence of nearly 30% of the population affected in eastern region of Nepal alone [2]. However, the prevalence and pattern of hypothyroid-ism depend on ethnic, geographic, and environmental factors including iodine intake status [1,3]. Hypothyroid-ism and hyperthyroidism are two widespread thyroid problems, of which hypothyroidism is much more com-mon. These disorders are eight times more common in women than in men [1].
The prevalence of thyroid dysfunction, by definition, is the testing of patients in various geographic regions, pri-mary care clinics and in population that have not been screened previously [4,5]. Thyroid function test panel is commonly used test for screening and evaluating thyroid dysfunction. The American Thyroid Association recom-mends that adults be screened for thyroid dysfunction by measurement of the serum thyrotropin concentration, be-ginning at age 35 years and every 5 years thereafter [6]. The screening of thyroid dysfunction is strongly recom-mended in high risk population such as goiter, iodine de-ficiency disorder, autoimmune disorder etc [7]. Nepal is one of the high risk populations with its high prevalence of iodine deficiency disorder [8]. Thus, the study was de-signed with an objective to assess the prevalence of thy-roid dysfunction in the Kavre region of Nepal which had yet to be assessed.
Material and Methods
Study Design
This was a hospital based study conducted in the Depart-ment of Biochemistry, Dhulikhel Hospital-Kathmandu University Hospital (DH-KUH). In this retrospective study, the subjects visiting DH-KUH from year January 2005 to June 2009 were enrolled. Those patients who had performed the thyroid function test, {i.e. free tri-iodothyronine (fT3), free thyroxine (fT4) and thyroid sti-mulation hormone (TSH)} were enrolled in the study. Subjects with incomplete thyroid function test were ex-cluded from the study. The age and sex of the subjects were also noted. Most of the subjects of study were resi-dent of Kavre district.
Collection of Blood samples
2.0 ml of venous blood was collected from the subjects attending DH-KUH. Blood collected in plain vial was allowed to clot and centrifuged at 3000 rpm for 15 min-utes. The separated serum was stored at -20°C for hor-mone assay.
Assay of thyroid function panel
Thyroid function test panel (fT3, fT4 and TSH) were as-sayed by the ELISA method using standard kit. fT3 and fT4 were assayed by competitive immunoassay method and TSH was assayed by sandwich immunoassay method. All three parameters were estimated by following the same standard protocol provided by the manufacturer (RFCL, India). For each analyte, 100 μL of enzyme con-jugates of corresponding analytes were added to the wells after the addition of the 50 μL samples and incubated for 60 minutes and washed thrice with the wash buffer to wash the excess of the conjugate. After this 100 μL of TMB (Tetramethyl benzidine) substrate was added to each well and incubated for exactly 15 minutes and reac-tion stopped with the 50 μL of 0.1 N HCl solution. The reading of each well was taken at 450 nm against a differ-ential filter of 690 nm.
Criteria of thyroid dysfunction
The reference interval for fT3, fT4 and TSH were 1.4--4.2 pg/ml, 0.8--2.0 ng/dl and 0.4--6.0 IU/ml respectively. Thyroid function is considered normal (Euthyroidism) when subjects were presented with normal fT3, fT4 and TSH. Abnormal thyroid function was further categorized as hyperthyroid (Increased fT3, fT4 and decreased TSH), Subclinical hyperthyroid (increased fT3, fT4 and normal TSH), hypothyroidism (decreased fT3, fT4 and increased TSH), and Subclinical hypothyroidism (decreased fT3, fT4)
Statistical analysis
Data were entered and analyzed by Software Package for Social Sciences version 11.5 (SPSS 11.5). Data were rep-resented as percentage, frequency, mean and standard error. Chi-square test, ANOVA test and Mann Whitney Test were applied. Data were considered significant at P<0.05
Results
In present retrospective study, a total of 825 subjects were enrolled from January 2005 to June 2009. Among these subjects 596 were female and 229 were male. The sub-jects were classified according to thyroid status as Hypo-thyroidism, Hyperthyroidism, Subclinical hypothyroid-ism, Subclinical hyperthyroidism and Euthyroidism tak-ing reference of thyroid function test. Total hypothyroid-ism includes hypothyroidism plus subclinical hypothy-roidism and total hyperthyroidism represents hyperthy-roidism and subclinical hyperthyroidism.
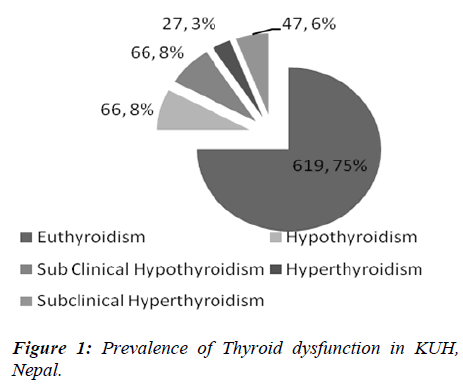
Figure 1 represents the prevalence of thyroid dysfunction in the population of Kavre. Among 825 subjects, 25 % of the subjects had thyroid dysfunction. Among deformity subjects, 132 subjects were total hypothyroid and 74 sub-jects were total hyperthyroid. The high proportions of subjects were suffering from hypothyroidism and sub-clinical hypothyroidism.
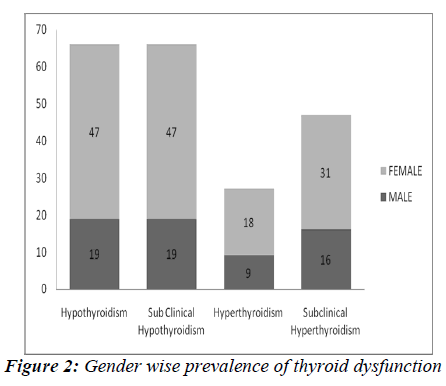
In the present study, the female to male ratio is 2.7:1. Among euthyroid subjects, 453 were females and 166 were males. The prevalence of thyroid dysfunction is 24% (n= 143) in 596 female subjects and 28% (n= 63) in 229 male subjects as shown in Figure 2. The numbers of fe-male subjects with thyroid dysfunction were greater than males.
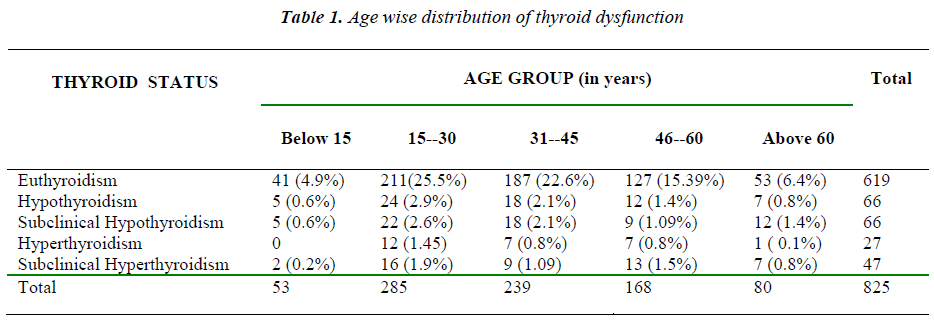
Table 1 represents the distribution of thyroid dysfunction with various groups. Among different age groups, highest number of subject lies between age group of 15-45. High number of total hypothyroidism was observed in 15-30 age groups. In age below 15 years, no cases of hyperthy-roidism was observed, hypothyroidism and subclinical hypothyroidism were prevalent. In all age group, high prevalence of hypothyroidism and subclinical hypothy-roidism were observed.
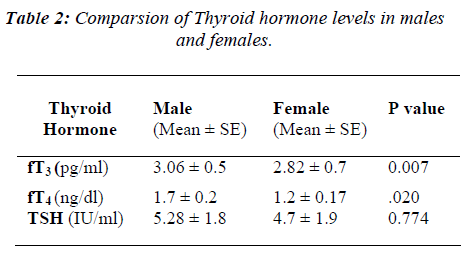
Table 2 represents the comparison of thyroid hormone levels in male and females. The mean TSH level in the male was higher than female but it was not statistically signficant. fT3 and fT4 levels were significantly different in males and females when the Mann Whittney Test was applied.
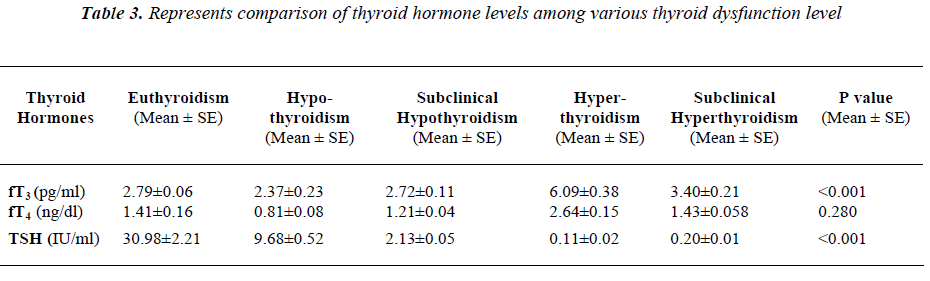
Table 3 represents comparison of thyroid hormone levels among various thyroid dysfunction level. The ANOVA test was applied to check the significant difference of variables between each group. fT3 and TSH were significantly different in various groups of thyroid dysfunction.
Discussion
Estimates of the prevalence of thyroid dysfunction depend upon methodological factors, classifications of hypothy-roidism, and composition of the community examined by age, ethnicity, and gender, making comparisons between studies of limited value. The prevalence and pattern of hypothyroidism depend on ethnic, geographic, and envi-ronmental factors including iodine intake status.
The prevalence of thyroid dysfunction was high in subjects attending DH-KUH. The similar study observed nearly 30% of the population were suffering from thyroid dysfunction in eastern part of Nepal [2]. The prevalence of hypothyroidism in various studies from around the world shows a considerable variation and its current pre-valence ranges from as low as 1% to as high as 20% for subclinical and 1 – 2% for overt hypothyroidism [3].
In the present study, the females more thyroid dysfunction than males. But contrasting result was observed by Baral N et al. (2002), where they reported equal proportion of thyroid dysfunction in male and female [2]. It has been reported earlier that 20% overall prevalence of thyroid dysfunctions in eastern Nepal in subject above 20 years of age [9]. Few studies were concordant with the present study which reported the subclinical hypothyroidism and overt hypothyroidism were higher in female as compared to males [10,11]. In other similar study, the prevalence of thyroid dysfunction was more common among women than men. The percentage of thyroid dysfunction among women was 13% and among men was 5% [3].
In the present study, the prevalence of hypothyroidism were higher than hyperthyroidism. Hypothyroidisms are generally associated with iodine deficiency and Nepal is an endemic area of iodine deficiency with prevalence of approximately 26.5% of iodine deficiency disorder [8]. The iodine deficiency and hypothyroidism may be exacerbated with geographical structure and food habit. Soil erosion with washing away of iodine from soil in hilly areas, use of non-iodized salts and intake of various goitrogens may also have aggravated the problem. In study conducted by Niafar M et al. (2009) hypothyroid-ism was common in Iranian population, as 12.8% of women and 4.7% of men had hypothyroidism; however, most of them were mildly hypothyroid. These data are consistent with reports of the high prevalence of hypothy-roidism in other iodine-sufficient populations. As in other studies in developed countries, hypothyroidism tends to increase with age and is more common in women, and people with goiter [12].
Furthermore, hypothyroidism is the most common thyroid disorder in the adult population and is more common in older women [13]. However, thyroid dysfunction in eld-erly individuals often occurs unnoticed, and methods for accurate detection may be controversial [14]. Hypothy-roidism is usually autoimmune in origin, presenting as either primary atrophic hypothyroidism or Hashimoto's thyroiditis and rarely pituitary or hypothalamic disorders can result in secondary hypothyroidism [13]. Similarly Baral N et al. (2002) have reported high prevalence of hypothyroidism among thyroid dysfunction [2]. By con-trast hyperthyroidism is much less common compared to hypothyroidism. Graves' disease is the most common cause and affects primarily young adults. Toxic multi-nodular goiters tend to affect the older age-groups [13]. In present study, the prevalence of total hyperthyroidsim was 9% including both subclinical hyperthyroidism(6%) and hyperthyroidism(3%). One similar study showed con-trasting result where the overall prevalence of thyroid dysfunction in the sample was 12.7%; relatively low compared with the present study. Of the 73 participants with high TSH levels, 15 (20.5%) had overt hypothyroid-ism, and of the 54 participants with low TSH levels, 12 (22.2%) had overt hyperthyroidism. Only one participant (1.85%) had T3 toxicosis [12].
Although all age group presented with thyroid dysfunc-tion a high number of subjects was observed between age groups of 15-45 years of age. One similar study reported the mean age of thyroid dysfunction is approximately 39 years of age, which showed the accumulation and manifestation of disorder symptoms in this age group. Few studies have revealed that incidence of thyroidism increases with advancing age [10,14-18]. Children under 15 have presented with hypothyroidism which may be associated with iodine deficiency disorder or Downs syndrome which ultimately retards physical and mental growth and develpoment [8,19]. Few studies have shown obesity, diabetes and metabolic syndrome have strong association with thyroid dysfunction [9,13]. Some studies have also shown the association of hypothyroidism with depression [20,21].
There were few limitations of our study. The TSH test result is an excellent tool for screening new patients for thyroid disease but the complete thyroid panel is needed for an accurate diagnosis and assessment of thyroid func-tion. First, the present study was based on routine thyroid function test i.e. serum free T3, free T4 and TSH meas-urement. The present study could have been strengthened if Total T4, Total T3, thyroglobulin, anti-thyroperoxidase (anti-TPO), anti-thyroglobulin (anti Tg), TSH receptor antibodies and Thyroid stimulating immunoglobulin (TSI) were included in stratifying thyroid dysfunction. Second, the possibility that TSH cut-offs used in the present study may have understated health risk. The cut-offs used were those recommended by the manufacturer of the kit and other studies because Nepal does not have its own refer-ence interval for thyroid function test panel.
Conclusion
Because the present study was a hopital based study, it may not represent the whole population. But, the study has identified the burden of thyroid dysfunction in Kavre and can be used as baseline data for future studies. The present study has revealed the prevalence of thyroid dysfunction typically hypothyroidism and subclinical hypothyroidism were higher in the Kavre region but the etiology of the disease remains unidentified. Moreover, the disease were preponderant in women and the elderly.
Recommendation
Further population based epidemeological studies are needed to establish the accurate prevalance and predominent etiological factors of thyroid dysfunction in this region of the country. In addition, the role of depression, obesity and diabetes must be extensively studied and explicitly defined. The study recommends thyroid dysfunction screening and treatment campaigning in the population of Kavre district to reduce the burden of disease.
Acknowledgement
We acknowledge the valuable financial support from Dhulikhel Hospital-Kathmandu University Hospital. The authors are grateful to all the staff at the Clinical Bio-chemistry Laboratory, Dhulikhel Hospital-Kathmandu University Hospital for their co-operation and skillful technical assistance.
References
- Peter PAS eds. Epidemiology of Thyroid dysfunction-hypothyroidism and hyperthyroididm. Thyroid Interna-tional 2009; 2: 1-16
- Baral N, Lamsal M, Koner BC, et al. Thyroid dysfunc-tion in eastern Nepal. South Asian J Trop Med Public Health 2002; 33: 638-641.
- Aminorroaya A, Janghorbani M, Amini A et al. The prevalence of thyroid dysfunction in an iodine-sufficient area in Iran. Arch Iranian Med 2009; 12: 262 - 270.
- Parle JV, Franklyn JA, Cross KW, et al. Circulating lipid and minor abnormalities of thyroid function. Clin Endocrinology 1992; 37: 411-414.
- Friedman MN. Screening for thyroid disease. Ann Med 1999;130: 161-162.
- Ladenson Paul W. American thyroid association guide-lines for detection of thyroid dysfunction. Arch Intern Med. 2000; 160: 1573-1575.
- Staub JJ, Althaus BU, Engler H et al. Spectrum of sub-clinical and overt hypothyroidism: effect on thyrotro-pin, prolactin, and thyroid reserve and metabolic im-pact on peripheral target tissue. Am J Med 1992; 92: 631-642.
- Gelal B, Aryal M, Das BKL, et al. Assessment of io-dine deficiency status among school age children of Nepal by urinary iodine assay. South Asian J Trop Med Public Health 2009; 40: 538- 543.
- Shrestha S, Das BKL, Baral N, et al. Association of metabolic syndrome and its component with thyroid dysfunction in females. Int J Diab Dev Ctries 2007; 27: 24-26.
- Tunbridge WMG, Evered DC, Hall R, et al. The spec-trum of thyroid disease in a community: the Whickham survey. Clin Endocrinol 1977; 7: 481-483.
- Surks MI, Chopra IJ, Mariash CN et al. American thy-roid association guidelines for use of laboratory tests in thyroid disorders. J A M A 1990; 263: 1529-1532.
- Niafar M, Aliasgharzadeh A, Bahrami A, et al. Preva-lence of thyroid dysfunction in the elderly women of Iran. Endocrine Abstracts 2009; 20: 137.
- Wu Patricia. Diabetes and thyroid disease. Clinical Diabetes 2008; 18: 111-118.
- Dos Remedios LV, Weber PM, Feldman R et al. De-tecting unsuspected thyroid dysfunction by the free thy-roxine index. Arch Intern Med 1980; 140: 1045-1049.
- Eggertsen R, Petersen K, Lundberg PA, et al. Screening for thyroid disease in a primary care unit with a thyroid stimulating hormone assay with a low detection limit. Brit Med J 1988; 297: 1586- 1592.
- Falkenberg M, Kagedal B, Norr A. Screening of an elderly female population for hypo- and hyperthyroid-ism by use of a thyroid hormone panel. Acta Med Scand 1983; 214: 361-365
- Wang C, Crapo LM. The epidemiology of thyroid dis-ease and implications for screening. Endocrinol Metab Clin North Am 1997; 26: 189-218.
- Arem R, Patsch W. Lipoprotein and apolipoprotein levels in subclinical hypothyroidism: effect of levothy-roxine therapy. Arch Intern Med 1990; 150: 2097-2100.
- Shaw CK, Thapalia A, Nanda S, Shaw P. Thyroid dys-function in Down Syndrome. Kathmandu Univ Med J 2006; 4: 182-186.
- Das BKL, Baral N, Shyangwa PM, et al. Altered serum levels of thyroxine, triiodothyronine and thyroid stimu-lating hormone in patients with depression. Kathmandu Univ Med J 2007; 5: 330-334.
- Chakrabarti K, Singh PM, Joshi SP. Thyroid dysfunc-tion in depression. Nepal Med Coll J 2006; 8: 47-48.