ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2015) Volume 26, Issue 1
The knowledge about, beliefs and attitudes of medical students regarding vaccination against the human papillomavirus, in South Africa: A Cross- Sectional Study.
1Graduate School of Business and Leadership, University of KwaZulu-Natal (Westville Campus), South Africa.
2Medical Sociology and Health Policy, University of Antwerp, Belgium.
- *Corresponding Author:
- Muhammad Hoque
Graduate School of Business and Leadership
University of KwaZulu-Natal (Westville Campus)
South Africa
Accepted date: September 30 2014
There are two vaccines for cervical cancer and both are available in South Africa. Both these vaccines are currently being considered for a national vaccination programme. The successful implementation of a vaccination programme will largely depend on how future clinicians are oriented regarding these vaccines. The purpose of this study was to investigate the knowledge, attitude and beliefs of medical students in South Africa concerning vaccination against the human papillomavirus (HPV). This was a cross-sectional study conducted among 100 medical students using a self-administered questionnaire. More than two-thirds (71%) of the respondents were aware of HPV and among them 81.2% mentioned vaccination against HPV. The majority (81.7%) were aware that persistent HPV infection is a cause of cervical cancer. Only 14.5% of the medical students knew that between 60 – 80% of cervical cancers is caused by HPV types 16 and 18. Overall, knowledge regarding HPV infection was low among the medical students as the average score was 3.23 (possible range was 0 to 9). The majority of the students (72.9%) indicated that the vaccine should be given to girls before the onset of sexual activity. Overall, 86.7% of respondents intend to prescribe HPV vaccines. In conclusion, overall, knowledge regarding HPV vaccination among the medical students in South Africa was low. But they had a positive attitude towards it. There is a strong need to provide more education to medical students about the relationship of HPV infection and cervical cancer and the benefits of vaccinating adolescent girls to prevent cervical cancer in the future.
Keywords
Vaccine, cervical cancer, HPV, cross sectional study
Introduction
Cervical cancer is the most common gynecological cancer among women worldwide. More than half a million women are diagnosed with cervical cancer contributing to around 275,100 deaths, across the globe annually. More than 85% of the deaths occur in developing countries that have minimal resources to cope with the situation [1]. Thus, globally it is a public health problem. The discovery of the human papillomavirus (HPV), the fact that HPV is responsible for virtually all cervical cancers and the development of HPV vaccines opens up exciting new possibilities for controlling this disease [2].
In South Africa, cervical cancer is one of the leading causes of death among women [3]. Each year, more than 3,000 women die from cervical cancer and it is estimated that more than 4,000 women will die each year by the year 2025. The age-standardized incidence rate of cervical cancer in South Africa is approximately 22.8 per 100,000 and mostly black women are affected [4,5]. The differences might be related to unequal access to healthcare, differences in socioeconomic status and exposure to HPV and HIV infection [5]. It is reported that a majority of HIV positive women are co-infected with HPV [6]. Researchers concluded that there was a 2-to 22 times higher risk of developing cervical cancer among HIV positive women than among HIV negative women [7]. In South Africa, because of the high prevalence of HIV and TB, cervical cancer has been looked upon in a stepmotherly way. Also because of poor quality of cancer preventative services there is a high incidence of cervical cancer in South Africa [8].
The bivalent vaccine CervarixTM, for HPV types 16 and 18; and the quadrivalent vaccine GardasilTM, for HPV types 16 and 18, as well as non-oncogenic HPV types 6 and 11, which are the most common types causing genital warts are available in South Africa [9]. Both vaccines are given in a three-dose schedule: 0, 1 and 6 months for the bivalent vaccine; 0, 2 and 6 months for the quadrivalent vaccine [9]. These vaccines are currently being considered for a national vaccination programme in South Africa, which will almost certainly make a significant difference in the cervical pre-cancer and cancer incidences in the future.
To implement HPV vaccine program successfully in any country, an awareness program should be conducted at various levels regarding HPV infection and cervical cancer. In a few years time medical students will be the practicing clinicians. They will be the first line information resources for the population they will serve. Therefore, the objective of this study is to investigate the knowledge, attitude and beliefs of medical students in South Africa concerning vaccination against HPV.
Materials and Methods
This was a cross-sectional study conducted among all the 1,199 medical students who were registered at the University of Limpopo (Medunsa Campus) during 2013.
Sample size for the study was calculated based on the following information: assuming 90% had sufficient knowledge regarding the HPV vaccine, with 5% reliability, and design effect as 1, the study required 91 students. We added 20% more to the sample size for incompleteness thus the final sample size became 109 students. The study sample was selected using multistage sampling techniques. Firstly, students were stratified according to year of study. Secondly, probability proportional to sampling method was used to select the samples. Part-time and non-medical students were excluded from the study. A self-administered questionnaire, with closed and a few open-ended questions, was developed for this study, based upon the Model for Clinical Prevention [10]. This model was chosen because it takes into consideration predisposing factors for physicians (health, beliefs and attitudes), and enabling factors (knowledge). The questionnaire consisted of three sections assessing: (1) General information, (2) HPV infection and its prevention (58 items), and (3) demographic characteristics. On average, the study questionnaire took about 15–20 min to complete.
Approval from the Medunsa Research Ethics Committee of the University of Limpopo, and from the Deputy Vice- Chancellor of Medunsa was obtained before commencing with the study. All the participants were informed fully about the study. It was also highlighted that participation in the study was voluntary and anonymity and confidentiality would be maintained at all times as no names of the participants appeared on the questionnaire.
The main researcher collected data from the students. The researcher allocated dates for different academic years. Prior to the allocation of dates, the researcher selected classes randomly and then communicated with the corresponding lecturer about the data collection procedure. Once the lecturer agreed, the researcher went to the corresponding lecturers’ lecture room and attended the lecture. Upon completion of the lecture, the lecturer then introduced the researcher to the class. The researcher then provided an explanation of the study and outlined the purpose and objectives of the study. Each participant signed a consent document before completing the questionnaire in the presence of the researcher.
Data were entered into a Microsoft Excel 2003 spread sheet and imported into SPSS 21.0. for Windows for analysis. For nine knowledge items, a “True–False–I do not know” scale was used. One point was given for each correct answer. For items measuring perceived professional and societal support/barriers and perceived benefit from vaccination, as well as the intention to recommend an HPV vaccine, a 4-point Likert scale, ranging from strongly disagree (one point) to strongly agree (four points) was used.
The analysis of the results was summarized using descriptive summary measures: expressed as mean (SD) for continuous variables and percentages for categorical variables. A multivariate logistic regression model was carried out to determine variables independently associated with the intention to prescribe HPV vaccination.
Results
A total of 110 medical students completed the questionnaire. Ten questionnaires (0.5%) were excluded from the analysis because of incompleteness. Results indicated that 36.6% of the respondents were 20 years or below, 45.1% were between 21 and 24 years, and the rest were 25 years old or above. Average age of the students was 22.59 yrs (SD=4.14yrs). More than half of the students were female students (62.4%). Regarding years of study, 26% were from the second year, followed by the third year (21.9%), the fourth year (21.9%), the fifth year (21.9%), and the sixth year (8.3%).
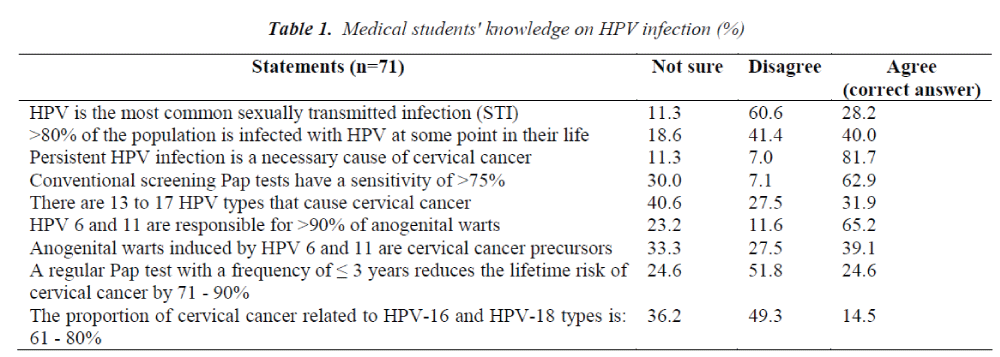
More than two-thirds (71%) of the respondents were aware of HPV and among them 81.2% knew about HPV vaccination. Only those students who were aware of HPV were asked further questions concerning HPV infection and cervical cancer screening which are reported in Table 1. Only 28.2%of the respondents knew that HPV is the most common sexually transmitted infection. Among those who were aware of HPV, 81.7% knew that persistent HPV infection is the pivotal cause of cervical cancer. A large proportion of students (62.9%) mentioned that the sensitivity of conventional Pap tests is >75%. The fact that between 60 – 80% of cervical cancers is caused by HPV types 16 and 18, is known by only 14.5% of the medical students. More than half ( 60.9% ) of the respondents did not know that anogenital warts induced byHPV6 and HPV11 are cervical cancer precursors. Overall, knowledge regarding HPV infection was low among the medical students as the average score was 3.23 (possible range was 0 to 9). The majority of the students (87.7%) reported that they do not have sufficient information regarding HPV infection.
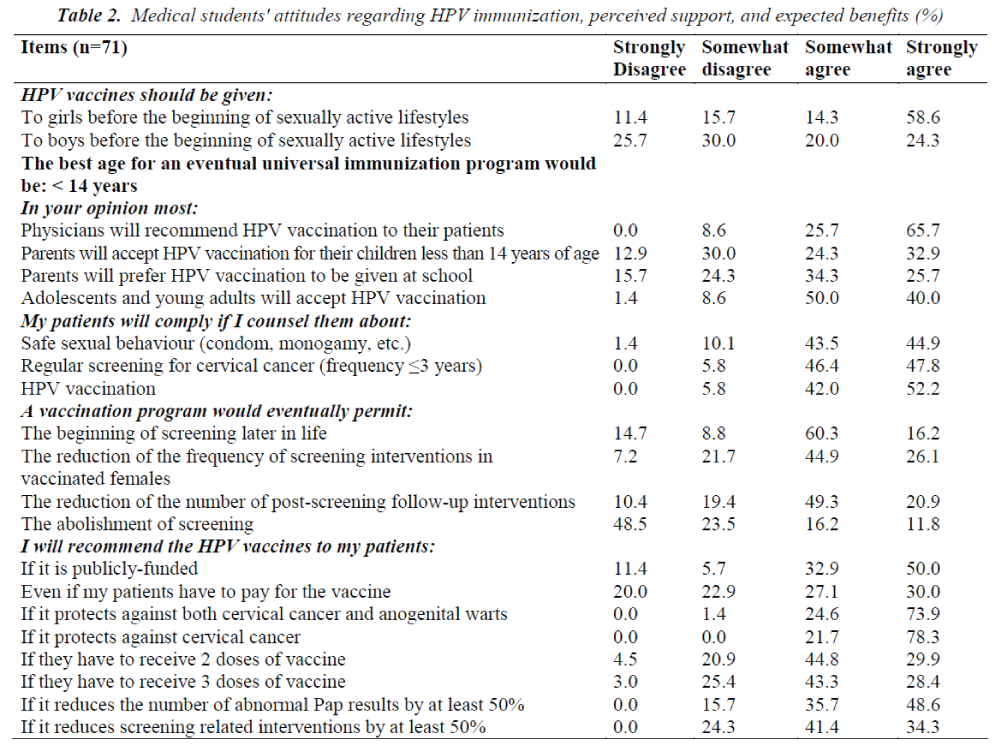
Table 2 summarizes students’ opinions, attitudes and intentions towards potential HPVvaccine use. The majority of the students (72.9%) indicated that the vaccine should be given to girls before the onset of sexual activity and 69.6% believed that girls become sexually active by the age of 14 years. More than half (54.3%) of the students mentioned the age of 14 – 18 years as the best age for an eventual universal vaccination program, followed by less than 14 years (27.1%) and the rest (18.6%) reported more than 18 years. No significant difference (p = 0.30) regarding the best age for an eventual universal vaccination program was observed between male and female students.
More than 90% of the students believe that physicians will support HPV vaccination and adolescents and young adults will accept HPV vaccination. More than half (57.2%) believe thatparents will accept HPV vaccination for their children under the age of 14 years and 60% believethat parents will prefer HPV vaccination to be given at school. Almost three-quarter (71%) of respondents expect that the vaccination will reduce the frequency of screening in vaccinated women, and 70.2% believe that it will reduce the number of post-screening followupinterventions. The majority (82.9%) of respondents intend to recommend HPV vaccination if it’s publicly funded and 57.2% if patients have to pay for the vaccine. Almost all (98.6%) students intend to recommend a vaccine that protects against both cervical cancer and anogenital warts, while all the students reported that they will recommend a vaccine that protects against only cervical cancer.
Overall, 86.7% of respondents intend to prescribe HPV vaccines. Applying stepwise logistic regression analysis, the study did not find any significant predictor for prescribing the HPV vaccine (data not shown).
Discussion
The present study investigated medical students’ knowledge, attitude and beliefs concerning vaccination against HPV. The majority (71%) of the respondents was aware of HPV and among them 81.2% mentioned HPV vaccination. An Indian study conducted among medical students reported that 75.6% of respondents were aware of the availability of a vaccine against cervical cancer [11]. A Malaysian study conducted among university students found that only 21.7% had heard of HPV and 10.3% had heard of the HPV vaccine [12]. In a Ghanaian study conducted among women where a majority of the participants had received higher education, only 40% had heard about a HPV vaccine [13].
Results from the current study indicated that a majority of the students knew that persistent HPV infection is the primary cause of cervical cancer. This finding is similar to the study conducted among medical students in India [11]. A higher proportion of incorrect responses were observed for statements related to Pap test sensitivity and the impact of the regular screening on the lifetime risk of cervical cancer than for other knowledge items. An important proportion of the medical students wrongly associated anogenital warts induced by HPV6 andHPV11 with cervical cancer precursors. This might send a wrong message to their patients. In addition, some respondents overestimated the proportion of cervical cancer related to HPV16and HPV18, which may lead to an overestimation of the expected vaccine impact. Studies conducted among women from South Africa, Kenya, and Botswana found that women had little knowledge about cervical cancer or the HPV vaccine [11,14,15].
Overall, knowledge regarding HPV infection was low. But, first and second year students had lower knowledge score (2.17 vs 3.38) than their older counterparts. This finding is in contrast with the study from Malaysia [16]. The Malaysian study conducted among medical and pharmacy students found a high level of knowledge regarding HPV vaccination. A possible reason for this could be that the Malaysian study included students from the third year whereas the present study included students only from the first and the second years. First year and second year students do not come into contact with clinical issues and this might have led to them not having enough information compared to older students.
Similar to a Chinese study, a large number of medical students in the present study did not know that HPV vaccination should be taken before sexual debut, after which the risk of infection with HPV increases dramatically [17]. Two studies conducted among Fellows of the American College of Obstetricians and Gynecologists and family physicians supported vaccination of 9 to 13-yearold girls [18,19]. A Brazilian study found that physicians and medical students reported preferences for vaccinating girls at ages ranging from 14 to 18 years [20]. Among South African girls, the perceived median age of sexual activity is considered between 9 and 15years. A qualitative study conducted at policy, health service and community levels of enquiry investigating key challenges and barriers towards the introduction of HPV vaccine in the Western Cape Province, South Africa reported that some providers and community respondents suggested commencing at the age of 9 due to high levels of sexual abuse and early onset of sexual activity in many communities [21].
It has been demonstrated that in general people are likely to accept vaccination and that clinicians and other healthcare providers are the most trusted people to disseminate this evidence. The present study found that a majority of the students believe that physicians will support HPV vaccination and intend to prescribe the HPV vaccine. This finding is in contrast with other studies conducted among doctors. For example, American clinicians are not always the strongest advocates of HPV vaccination. One study conducted among medical specialties found that only35% of responders would always recommend vaccination to young adolescents [22]. Another study conducted among paediatricians found only 46% were willing to recommend vaccination for girls under 12, rising to 77% for 13– 15 year olds [23]. A very recent study conducted among family medicine residency graduates in the USA reported that 79% offer the HPV vaccine atleast most of the time to their adolescent female patients in their practice [24].
Study limitations
According to the authors, the present study is the first to investigate the knowledge, attitudes and belief about the HPV vaccine among the future health care professionals in South Africa. However, the study had some limitations. It was based on convenience sampling. Medical students from only one university were included which might not reflect the overall awareness of medical students in South Africa. These limitations should be taken into consideration before interpreting the findings.
Conclusion
HPV vaccination is a relatively new concept for primary prevention of cervical cancer. Overall, knowledge regarding the HPV vaccine among the medical students in our study is low. But they had a positive attitude towards it. Many of them are willing to prescribe the vaccine to their adolescent patients. The academic curriculum in the medical schools needs to focus more on such high priority practical upcoming issues. There is a strong need to provide more education for medical students about the relationship of HPV infection and cervical cancer and the benefits of vaccinating adolescent girls to prevent cervical cancer in the future.
Competing interests
None declared.
Acknowledgement
The authors wish to thank all the medical students who voluntarily participated in the study.
References
- Jemal A, Bray F, Center MM, Ferlay J, Ward E, Forman D. Global cancer statistics. CA Cancer J Clin 2011; 61: 69-90.
- Muñoz N, Bosch FX, de Sanjosé S, Herrero R, Castellsagué X, Shah KV, Snijders PJ, Meijer CJ. Epidemiologic classification of human papilloma virus types associated with cervical cancer. N Engl J Med 2003; 348: 518-527.
- Francis SA, Nelson J, Liverpool J, Soogun S, Mofammere N, Thorpe RJ Jr. Examining attitudes and knowledge about HPV and cervical cancer risk among female clinic attendees in Johannesburg: South Africa. Vaccine 2010; 28: 8026-8032.
- WHO/ICO Information Centre on HPV and Cervical Cancer (HPV Information Centre). Human Papillomavirus and Related Cancers in South Africa. Summary Report 2010. Available at: www.who.int/hpvcentre [Date accessed: 25 February 2013].
- Mqoqi N, Kellett P, Sitas F, Jula M. Incidence of histologically diagnosed cancer in South Africa, 1998– 1999. Johannesburg: National Cancer Registry of South Africa, National Health Laboratory Service, 2004.
- Denny LA, Franceschi S, de Sanjosé S, IHeard I, Anna Barbara Moscicki, Palefsky J. Human Papilloma virus, Human Immunodeficiency Virus and Immunosuppression. Vaccine 2012; 30S: F168-F174.
- De Vuyst H, Lillo F, Broutet N, Smith JS. HIV, human papilloma virus, and cervical Neoplasia and cancer in the era of highly active antiretroviral therapy. Eur J Cancer Prev 2008; 17: 545-554.
- Mayosi BM, Flisher AJ, Lalloo UG, Sitas F, Tollman SM, Bradshaw D. The burden of non-communicable diseases in South Africa. Lancet 2009; 374: 934-947.
- World Health Organization: Human papilloma virus vaccines. WHO position paper. Wkly Epidemiol Rec 2009; 84: 118-131.
- Walsh JME, McPhee SJ. A systems model of clinical preventive care: an analysis of Factors influencing patient and physician. Health Educ Q 1992; 19: 157-175.
- Pandey D, Vanya V, Bhagat S, Binu VS, Shetty J. Awareness and attitude towards Human papilloma virus (HPV) vaccine among medical students in a premier medical school in India. PLoS ONE 2012; 7: e40619.
- Wong LP, Sam IC. Ethnically diverse female university students’ knowledge and Attitudes toward human papilloma virus (HPV), HPV vaccination and cervical cancer. Eur J Obstet Gynecol Reprod Biol 2010; 148: 90-95.
- Coleman MA, Levison J, Sangi-Haghpeykar H. HPV vaccine acceptability in Ghana, West Africa. Vaccine 2011; 29: 3945-3950.
- Becker-Dreps S, Otieno WA, Brewer N, Agot K, Smith JS. HPV vaccine acceptability among Kenyan women. Vaccine 2010; 28: 4864-4867.
- DiAngi YT, Panozzo CA, Ramogola-Masire D, Steenhoff AP, Brewer N. A cross Sectional study of HPV vaccine acceptability in Gaborone, Botswana. PLoS ONE2011; 6: e25481.
- Rashwan HH, Saat NZNM, Manan DNA. Knowledge, Attitude and Practice of Malaysian Medical and Pharmacy Students Towards Human Papilloma virus Vaccination. Asian Pacific J Cancer Prev 2012; 13: 2279- 2283.
- Riedesel JM, Rosenthal SL, Zimet GD, Bernstein DI, Huang B, Lan D, Kahn JA. Attitudes about human papilloma virus vaccine among family physicians. J Pediatr Adolesc Gynecol 2005; 18: 391-398.
- Raley JC, Followwill KA, Zimet GD, Ault KA. Gynecologists’ attitudes regarding Human papilloma virus vaccination: A survey of Fellows of the American College of Obstetricians and Gynecologists. Infect Dis Obstet Gynecol 2004; 12: 127-33.
- de Carvalho NS, Teixeira LM, Pradel EM, Gabardo J, Joly C, Urbanetz AA. Vaccinating against HPV: physicians’ and medical students’ point of view. Vaccine 2009; 27:2637-40.
- Chow SN, Soon R, Park JS, Pancharoen C, Qiao YL, Basu P, Ngan HY. Knowledge, attitudes, and communication around human papilloma virus (HPV) vaccination amongst urban Asian mothers and physicians. Vaccine 2010; 28: 3809-17.
- Harries J, Moodley J, Barone MA, Mall S, Edina SE. Preparing for HPV vaccination in South Africa: Key challenges and opinions. Vaccine 2009; 27: 38-44.
- Vadaparampil ST, Kahn JA, Salmon D, Lee JH, Quinn GP, Roetzheim R, Bruder K, MaloTL, Proveaux T, Zhao X, Halsey N, Giuliano AR. Missed clinical opportunities: provider recommendations for HPV vaccination for 11–12 year old girls are limited. Vaccine 2011; 29: 8634-41.
- Daley MF, Liddon N, Crane LA, Beaty BL, Barrow J, Babbel C, Markowitz LE, Dunne EF, Stokley S, Dickinson LM, Berman S, Kempe A. national survey of pediatrician knowledge and attitudes regarding human papilloma virus vaccination. Pediatrics2006; 118: 2280-9.
- Post RE, Carek PJ, Mainous AG 3rd, Diaz VA, Johnson SP. Factors Affecting HPV Vaccine Use Among Recent Family Medicine Residency Graduates. Fam Med 2013;45: 90-4.