ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 8
Importance of antivenom in management of scorpion envenomation with epidemiologic and clinical characteristics
Ali Duman*, Bekir Dagli, Ayhan Akoz, Mucahit Avcil, Serhat Orun and Kenan Ahmet Turkdogan
Department of Emergency Medicine, Adnan Menderes University, Aydin, Turkey
- *Corresponding Author:
- Ali Duman
Department of Emergency Medicine
Adnan Menderes University, Aydin, Turkey
Accepted date: February 07, 2017
The management of scorpion stings, especially those including antivenom treatment, remains a subject of controversy. The purpose of this study was to offer the epidemiologic and clinical characteristics of patients with scorpion sting and to determine the efficacy of antivenom treatment in the management of these patients. A total of 106 adult patients admitted for scorpion sting to our ED between January 2013 and December 2015 were evaluated and 98 patients were included in the study. The clinical severity and treatment of each case was evaluated using Abroug’s classification. According to Abroug’s classification, there were 75 (76.5%), 15 (15.3%), and eight (8.2%) patients in grade I, II, and III, respectively. Length of stay of the Abroug grade II patients who did not receive scorpion antiserum was longer than grade II patients who received scorpion antiserum. However, length of stay of the grade III patients who did not receive scorpion antiserum was shorter than grade III patients who received scorpion antiserum. It was observed that even though scorpion antiserum can have serious side effects, the administration of a low dose of antivenom relieved severe pain that was not relieved by symptomatic treatment or narcotic analgesics and the Abroug’s classification grades of the cases and not requiring antivenom treatment at the beginning can change or require antivenom in the following period. It was concluded that patients with local symptoms should be followed up for 6-12 hours or to be referred to centers performing this follow up.
Keywords
Antivenom treatment, Scorpion sting, Abroug’s classification, Local symptoms, Systemic symptoms.
Introduction
Scorpion envenomation, or scorpionism, remains a serious health problem worldwide [1]. Although scorpion stings occur on all continents (except Antarctica), the epidemiology of scorpionism is still poorly known [2,3]. Accidents seem to be more common in some areas of the world, and there is considerable geographical variation, either in incidence or severity [2,3]. Scorpionism is relevant in at least 7 limited areas of the world. The incidence and severity of envenomation are higher in the northern Sahara, the southern and eastern regions of Africa, the Middle East, South India, Mexico, Brazil, and the Amazonian basin area (Guyanas, Venezuela, and northern Brazil) [3].
Scorpions are distributed worldwide, and nearly 100,000 scorpion sting cases, 800 of which result in fatality, are reported around the world [4]. Nearly 30 of 1500 species of scorpions are recognized as potentially dangerous to humans [5]. In Turkey, 15 species belonging to four families Buthidae, Euscorpiidae, Iuridae, and Scorpionidae have been identified thus far [5]. The most venomous species appear to be L. quinquestriatus and A. crassicauda from the family Buthidae [6].
Scorpion envenomation is a life-threatening emergency and can cause serious health problems, such as cardiac dysfunction and respiratory failure, in tropical and subtropical regions [7]. Scorpion venom has local and local or systemic symptoms [8]. Mortality caused by scorpion sting is related to systemic symptoms such as pulmonary edema [9] and cardiac dysfunction such as ECG changes, including increased PR interval, QT dispersion, corrected QpT value and Pmin [10]. Despite the global occurrence and the hazard of scorpionism, epidemiological data are still limited due to unreported cases and few studies regarding this issue [3,7].
The management of scorpion stings remains a subject of controversy. The use of anti-scorpion serum, which is the only specific treatment, is disputed by some specialists [11], and symptomatic or adjuvant treatments, the importance of which is now recognized by all experts, require precisely useful drugs, indications, and dosages in many places [12,13].
The purpose of this retrospective study was to offer the epidemiologic and clinical characteristics of scorpion sting and share experience of antivenom treatment in the management of these patients.
Materials and Methods
All aspects of the study protocol were approved by the medical ethics committee and the local health authorities before conducting this study (Date: 11.12.2014; Protocol No: 2014/491). In Turkey, manufactures IgG (or Fab) antivenom from the venom of A. crassicauda is used for all scorpion sting cases [14].
A total of 106 adult patients admitted for scorpion sting to our ED, between January 2013 and December 2015 were included in the study. Our department is located in Aydin in the western region of Turkey. The population of the city center of Aydin is 256,000, and the population of the province is 1,050,000.
Patients aged 18 years and over who were admitted to the ED for treatment due to scorpion sting were included in the study. Because patients younger than 18 years of age were taken to the paediatric ED for treatment, they were excluded from this study. Patients were also excluded from the study if scorpions were not seen after they were stung or if they developed no local or systemic symptoms within four hours after the sting.
The following information was collected retrospectively: age, sex, month of admission, location of the incident, and follow up time in the ED, sting site, number of stings, local and systemic symptoms, treatment received, and patient’s condition. The clinical severity of each case was evaluated using Abroug’s classification [11]. The patients were monitored after their medical histories were taken and their physical examinations were completed. Abroug’s classification includes Grade I: pain and/or paresthesia at the site of scorpion sting; Grade II: fever, chills, nausea/vomiting, hypertension, and priapism; and Grade III: cardiovascular, respiratory, and/or neurologic symptoms. Adjuvant treatment was administered to patients according to the severity of local and systemic symptoms, and antivenom treatment was administered to the patients in case of need. The antivenom administration started with doses of two to five vials based on the severity of the symptoms, and repeat doses were administered when deemed necessary.
The Statistical Package for the Social Sciences 18 (SPSS Inc., Chicago, IL, USA) software package was used to carry out the statistical analyses for the data of the study. Normally distributed numerical variables were shown as mean ± standard deviation, and non-normally distributed numerical variables were shown as median (minimum-maximum) and categorical variables were shown in percentages. Intergroup differences were analyzed using Fisher’s test or chi-square test based on the features of the data. A p value <0.05 was accepted as statistically significant.
Results
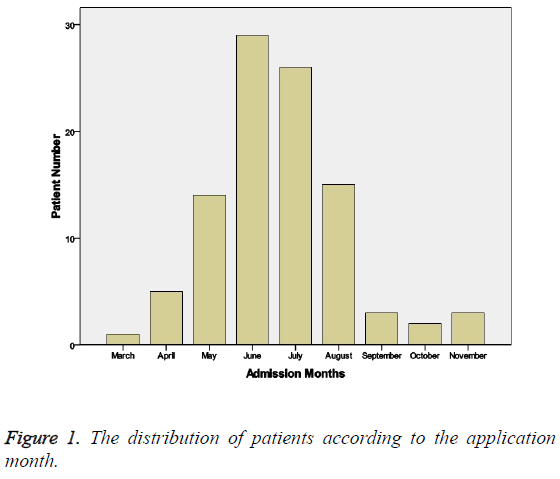
One hundred six patients who were admitted to our ED and who were hospitalized and followed up between 01 January 2013 and 31 July 2015 were included in the study. 8 cases were excluded from the study because their data could not be obtained. The average age of our patients was 45.9 ± 17.8 years (min 18, max 89). When classified based on age range, 57 (37 women, 20 men) of the patients were in the 18-49 year range, 26 (15 women, 11 men) were in the 50-64 year range, and 15 (6 women, 9 men) were 65 years of age and older. When classified based on sex, 40 (40.8%) of the patients were men. Thirty-nine (39.8%) of the patients came from the city center, 36 (36.7%) from the district, and 23 (23.5%) from a village (Table 1). When patient admissions were examined by month, 29 (29.6%) patients were admitted in June, 26 (26.5%) in July, 15 (15.3%) in August, 14 (14.3%) in May, five (5.1%) in April, three (3.1%) in September, three (3.1%) in November, two (2%) in October, and one (1%) in March (Figure 1). No cases of scorpion sting that included local or systemic symptoms and required follow up occurred in January, February, or December in our region in this approximately 2.5- year case review.
| Grade 1 | Grade 2 | Grade 3 | |
| n:75 | n:15 | n:8 | |
| Age | 45.72 ± 17,60 | 43.87 ± 18.47 | 51.63 ± 20.56 |
| Male/female Urban Rural |
31/44 29 46 |
4/11 6 9 |
5/3 4 4 |
| Duration of hospitalization/day | 0.85 ± 0.80 | 0.80 ± 0.90 | 1.50 ± 1.07 |
| Symptomatic treatment | 75 | 15 | 8 |
| Antivenom treatment | 12 | 3 | 4 |
| Multiple stings | 3 | 2 | 3 |
| Upper limb stings | 42 | 7 | 5 |
| Lower limb stings | 31 | 7 | 3 |
| Body stings | 1 | 1 | 0 |
| Head/Neck stings | 1 | 0 | 0 |
Table 1: Demographic and Clinical Characteristics of Patients according to the Abourg's Classification.
When the patients were classified according to Abroug’s classification, there were 75 (76.5%), 15 (15.3%), and eight (8.2%) grade I, II, and III cases, respectively. Local, systemic and cardiac and/or neurologic symptoms of our patients were presented in Table 2. Hospitalization period was 0.9 ± 0.8, 0.8 ± 0.9, and 1.5 ± 1.1 days for grades I, II, and III, respectively. The differences in hospitalization period between grades I and III and between grades II and III were statistically significant (p<0.005).
| Patients n (%) | |
|---|---|
| Local symptoms | |
| Pain in the sting region | 98 (100%) |
| Edema in the sting region | 30 (30.6%) |
| Local numbness | 8 (8.2%) |
| Systemic symptoms | |
| Pain in the whole body | 12 (12.2) |
| Fever | 9 (9.2%) |
| Numbness in the whole body | 8 (8.2%) |
| Nausea and vomiting | 7 (7.1%) |
| Dizziness | 4 (4.1%) |
| Vaginal bleeding | 1 (1%) |
| Diffuse edema | 1 (1%) |
| Hemoptysis | 1 (1%) |
| Urticarial rash/pruritus | 1 (1%) |
| Cardiac and/or neurologic symptoms | |
| Hypotension | 3 (3.1%) |
| Dyspnea | 2 (2%) |
| Cardiac rhythm disorders | 2 (2%) |
| Unconsciousness | 1 (1%) |
| Seizure | 1 (1%) |
Table 2: Local, systemic and cardiac and/or neurologic symptoms.
When the grades of our patients were examined according to age range, it was found that 45 (78.9%) of the 57 patients in the 17-49 year range were grade I, ten (17.5%) were grade II, and two (3.5%) were grade III. Nineteen (73.1%) of the 26 patients in the 50-64 year range were grade I, three (11.5%) were grade II, and four (15.4%) were grade III. Eleven (73.3%) of the 15 patients older than 65 years were grade I, two (13.3%) were grade II, and two (13.3%) were grade III.
When assessed based on site of the scorpion sting, it was found that 54 (55.1%) of the patients were stung in an upper extremity, 41 (41.8%) in a lower extremity, two (2%) in the torso, and one (1%) in the head/neck area; eight (8.2%) of the patients had multiple contacts.
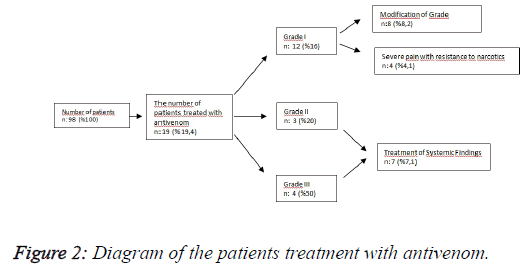
When symptomatic treatment (n=79, 80.7%) and antivenom treatment (n=19, 19.4%) were compared according to Abroug’s classification, antivenom treatment was administered to 12 (16%) grade I patients, three (20%) grade II patients, and four (50%) grade III cases (Figure 2). Although this difference was not statistically significant (p=0.069), the patients’ rates of receiving antivenom treatment increased as their grade increased according to Abroug’s classification. Thirteen of the 19 patients who were administered scorpion antiserum received one vial of antivenom, two patients received two vials, one patient received four vials, one patient received five vials, one patient received 20 vials, and one patient received 25 vials. The mean hospitalization period of the Abroug grade II patients who did not receive scorpion antiserum was 0.83 ± 0.93 days, and the mean hospitalization period of the grade II patients who received scorpion antiserum was 0.67 ± 1.15 days; this difference was not statistically significant (p=0.795). The mean hospitalization period of the grade III patients who did not receive scorpion antiserum was 0.75 ± 0.96 days, and the mean hospitalization period of the grade III patients who received scorpion antiserum was 2.25 ± 0.50 days; this difference was statistically significant (p=0.032).
The treatments administered to the patients were also examined according to Abroug’s classification. In the grade I group, antihistamines were administered to 53 (70.7%) patients, steroids to 50 (66.7%) patients, antibiotics to nine (12%) patients, scorpion antiserum to 12 (16%) patients, and narcotic analgesics to four (5.2%) patients. In the grade II group, antihistamines were administered to 11 (73.3%) patients, steroids to 13 (86.7%) patients, adrenalin to one (6.7%) patient, and scorpion antiserum to three (20%) patients. In the grade III group, steroids were administered to eight (100%) patients, adrenalin to three (37.5%) patients, and scorpion antiserum to four (50%) patients. Analgesic treatment was administered to all grade I, II, and III patients.
When hospitalization periods of the patients were examined, 40 patients (40.8%) stayed in the hospital for one day, 18 patients (18.4%) for two days, and four patients (4.1%) for three days; 36 patients (36.7%) were followed up for less than 24 h. When average age and hospitalization period of the patients were examined, the average age of the patients followed up for less than 24 h was 43.7 ± 17.7 years, and the average age of the patients followed up for 24 h and more was 53.7 ± 16.7; the difference between them was statistically significant (p=0.019). Patient grade according to Abroug’s classification increased with increasing age. In addition, hospitalization period increased as the patients’ Abroug’s classification increased; this difference was found to be statistically significant (p=0.019). Hospitalization period of the patients with no systemic symptoms was 1.2 ± 0.4 days, and hospitalization period of the patients with systemic symptoms was 1.5 ± 0.5 days; this difference was statistically significant (p=0.002).
Discussion
While the incidence of scorpion stings is underestimated due to a lack of exhaustive reporting of the cases; the mortality rate is probably better known. While more than 1,200,000 scorpion stings occur annually, the number of deaths could exceed 3250. According to the study of Altinkaynak et al. scorpion stings were mostly seen in Mugla (37.3%), Aydin (37%), and Denizli (19%) in the Aegean region of Turkey [14,15]. In our clinic, we hospitalized and followed up 98 scorpion sting cases over nearly 2.5 years, and one of our patients passed away.
When scorpion sting cases have been examined in terms of sex, most studies have reported that the number of male patients is higher, whereas some studies have stated that the number of female patients is higher. Jahan et al., Al-Asmari et al., and Hammoudi-Triki et al., reported a male to female ratio of 1.9:1, 2.6:1, and 2.9:1 respectively [16-18]. In the study of Ad?güzel et al. women were stung more often compared to men (60% and 40%, respectively), and 75% of the patients were older than 15 years of age [13]. On the other hand, one study reported that females were stung more frequently than males [16]. Jahan et al. reported a lower average age of 23.1 ± 16.8 in Saudi Arabia [16]. In Brazil, one study reported an average age of 33.6 ± 18.3 for scorpion sting cases [18]. In our study the average age of our patients was 45.9 ± 17.8, and 58.2% of our patients were in 18-49 year age range. In our study female/male ratio was 1.5:1 in 98 cases. We concluded that the reason why the female rate among our patients was higher and the affected group was mainly young and middle aged was that young and middle-aged women are more active in working areas, such as orchards, gardens, and fields, which are the habitats of scorpions in Turkey, especially in our region.
Scorpion sting cases are subject to seasonal variation all around the world. The majority of the scorpion stings are more prevalent in summer than in winter [17,19]. Morocco, Saudi Arabia, Iran and Texas have a high incidence of scorpion stings between June and September, May and September, April and October, and May and June [4,16,20,21]. Our study had a high incidence of scorpion stings between May and August; while June was the month when the cases were most frequent, we did not have any cases in December, January, or February. We think this finding is associated with the fact that people in our region often go to areas where scorpions are frequently found in order to work or have fun (e.g., fairs, picnics, countryside weddings, sports); in addition, people prefer to sleep on balconies and roofs more often during these months.
Epidemiologic studies have reported that scorpion stings are more common in the extremities [13,20,22]. Y?lmaz et al. found that while 95.2% of stings took place in the extremities, including hands, arms, legs, thighs, and feet, the stings most commonly involved the upper extremities (61.8%) [23]. Although, scorpion stings commonly involve the upper extremities in Turkey (55.1%), the literature data suggest a lower extremity predominance (58.6%) [6,14]. Thus, our findings are not in agreement with the literature. Our city is located in a very warm region of Turkey, and most people are engaged in agriculture. Our agricultural workers are mostly stung by scorpions on their hands and arms, as they work without taking adequate safety precautions, mostly due to either extreme temperature or lack of education.
Scorpion venom may cause local effects such as pain, heat, edema and systemic effects respiratory failure, cardiovascular toxicity, hemolysis, renal failure within the first 12–24 h after the sting [24]. Y?lmaz et al. stated that local symptoms such as pain, redness, and sensitivity in the extremity were most common; most of their patients were grade I according to Abroug’s classification, and none of their patients developed systemic symptoms [23]. In our study, 23.5% of the 98 cases we followed up were accompanied by systemic symptoms.
According to Abroug’s classification, 75 of our patients were classified as grade I, 15 were grade II, and eight were grade III. While 40.8% of our patients were hospitalized for one day, 18.4% for two days, and 4.1% for three days, 36.7% were followed up for less than 24 h. The grade I and II patients were followed up for an average of 20 hours in our clinic, whereas, the grade III patients were followed up for an average of 36 hours. The average age of our patients who were followed up for less than 24 h was 43.7 ± 17.7 years, and the average age of those who were followed up for 24 h and longer was 53.7 ± 16.7 years. The hospitalization period of the patients with no systemic symptoms was 1.2 ± 0.4 days, and the hospitalization period of those with systemic symptoms was 1.5 ± 0.5 days.
The Abroug’s classification grades of our patients increased with increasing age, and as the grade increased, the hospitalization period increased as well. We have considered that the differences in occurrence of local and systemic symptoms in different regions between our study and the literature and different hospitalization periods are associated with the scorpion species living in these regions, ages of the people stung, and the different amounts of venom injected in each case. Moreover, our results showed that the severity of the scorpion stings increased with age; therefore, we suggest that all clinicians should approach elderly scorpion sting patients with increased caution.
Many authors have emphasized the importance of earlier and better treatment in managing patients [20,21]. Treatment can be divided into two parts: antivenom therapy and symptomatic treatment [25]. Antivenom therapy is still debated: while many authors consider this therapy to be unnecessary, others advise its use [22,26]. In general, mild symptoms should be controlled with analgesics and antihistamines, whereas patients with systemic symptoms should be administered antivenom [27]. Touloun et al. stated that about 40% of scorpion stings in Morocco were treated exclusively with traditional medicine, 27% with both traditional and modern medicines, 28% with modern medicine alone, and 7% went without treatment [28]. In countries where scorpions are a serious public health problem, mortality has decreased thanks to antivenom and supportive treatments [25]. Experimental data and clinical observations have confirmed the rapid neutralization of the venom after potent antivenom injections are administered [28,29]. The treatments received by our patients were examined according to Abroug’s classification and it was found that antivenom was administered to 16% and narcotic analgesics to 5.2% of grade I patients, and antivenom was administered to 20% of grade II patients and 50% of grade III patients. Our study revealed that the administration rate of antivenom increased as the grade of our patients increased. In addition, it was observed that scorpion antiserum was administered to 12 of 75 grade I patients. We conducted Abroug’s classification of our patients according to their first admission data; however, the grades of some patients changed in the following process, and even if antivenom was not necessary for the pretreatment, it may have been required in the following process. Eight of our patients who were grade I and were administered antivenom changed clinics during followup. Of the four cases that were grade I and had intense local pain that responded partially to narcotics, we treated three patients with two vials of antivenom and one patient with four vials. Consistent with the literature, we think symptomatic treatment could be adequate for grade I patients with local symptoms only, while antivenom therapy is required to treat grade II and grade III patients with progressive local symptoms accompanied by systemic symptoms. We also think low doses of antivenom treatment could be beneficial in patients who are resistant to symptomatic treatment and do not obtain relief with narcotic analgesics.
Conclusion
When we evaluated the results of our study, we determined that antivenom treatment had an important role in both stopping the progress of local symptoms and treating systemic symptoms in the management of scorpion sting cases. Furthermore, we observed that even though scorpion antiserum can have serious side effects, the administration of a low dose of antivenom relieved severe pain that was not relieved by symptomatic treatment or narcotic analgesics. However, further studies are required for this suggestion to be included in a treatment algorithm.
Another important result of our study is that the Abroug’s classification grades of the cases and not requiring antivenom treatment at the beginning can change or require antivenom in the following period. When considering this situation, it is appropriate for patients with local symptoms to be followed up for 6-12 hours or to be referred to centers performing this follow up.
Limitations
Our study is retrospective, and some of the patient data could not be obtained, which restricted the results of our study, such as the activity being undertaken at the time of the sting. In addition, we could not determine exactly the time elapsed between the time of the incident and the time of ED admission. Lastly, the number of our cases was limited because the study was conducted in a single center.
References
- Adiguzel S, Ozkan O, Inceoglu B. Epidemiological and clinical characteristics of scorpionism in children in Sanliurfa, Turkey. Toxicon 2007; 49: 875-880.
- Bahloul M, Chabchoub I, Chaari A. Scorpion envenomation among children: clinical manifestations and outcome (analysis of 685 cases). Am J Trop Med Hyg 2010; 83: 1084-1092.
- Chippaux JP, Goyffon M. Epidemiology of scorpionism: a global appraisal. Acta Trop 2008; 107: 71-79.
- Abourazzak S, Achour S, El Arqam L, Atmani S, Chaouki S, Semlali I. Epidemiologic and clinical characteristics of scorpion stings in children in Fez, Morocco. J Venom Anim Toxins Inci Trop Dis 2009; 15: 255-267.
- Karatas A. Mesobuthus caucasicus (Nordmann, 1840) (Scorpiones: Buthidae) in Turkey. Euscorpius, 2005; 25: 1-9.
- Ozkan O, Adiguzel S, Yakistiran S, Cesaretli Y, Orman M, Karaer KZ. Androctonus crassicauda (Olivier 1807) scorpionism in the Sanliurfa Provinces of Turkey. Acta Parasitol Turcica 2006; 30: 239-245.
- Cesaretli Y, Ozkan O. Scorpion stings in Turkey: epidemiological and clinical aspects between the years 1995 and 2004. Rev Inst Med Trop São Paulo 2010; 52: 215-220.
- Ismail M, Abd-Elsalam MA, al-Ahaidib MS. Androctonus crassicauda (Olivier), a dangerous and unduly neglected scorpion-I. Pharmacological and clinical studies. Toxicon 1994; 32: 1599-1618.
- Razi E, Malekanrad E. Asymmetric pulmonary edema after scorpion sting: a case report. Rev Inst Med Trop Sao Paulo 2008; 50: 347-350.
- Al B, Yarbil P, Zengin S, Ercan S, Davutoglu V, Yildirim C. Impact of scorpion stings on electrocardiographic changes and relationship with body oxidant and antioxidant status. J Pak Med Assoc 2014; 64: 423-427.
- Abroug F, ElAtrous S, Nouira S, Haguiga H, Touzi N, Bouchoucha S. Serotherapy in scorpion envenomation: a randomised controlled trial. Lancet 1999; 354: 906-909.
- Freire-Maia L, Campos JA, Amaral CF. Approaches to the treatment of scorpion envenoming. Toxicon 1994; 32: 1009-1014.
- Adiguzel S, Ozkan O, Inceoglu B. Epidemiological and clinical characteristics of scorpionism in children in Sanliurfa, Turkey. Toxicon 2007; 49: 875-880.
- Ozkan O, Uzun R, Adigüzel S, Cesaretli Y and Ertek M. Evaluation of Scorpion Sting Incidence in Turkey. J Venom Amin Toxins incl Trop Dis 2008; 14: 131.
- Altinkaynak S, Ertekin V, Alp H. Scorpion envenomation in children. Turk Arch Ped 2002; 37: 48-54.
- Jahan S, Mohammed Al Saigul A, Abdul Rahim Hamed S. Scorpion stings in Qassim, Saudi Arabia-a 5-year surveillance report. Toxicon 2007; 50: 302-305.
- Al-Asmari AK, Al-Saif AA. Scorpion sting syndrome in a general hospital in Saudi Arabia. Saudi Med J 2004; 25: 64-70.
- Pardal PP, Castro LC, Jennings E, Pardal JS, Monteiro MR. Epidemiological and clinical aspects of scorpion envenomation in the region of Santarém, Pará, Brazil. Rev Soc Bras Med Trop 2003; 36: 349-353.
- Bosnak M, Ece A, Yolbas I, Bosnak V, Kaplan M, Gurkan F. Scorpion sting envenomation in children in southeast Turkey. Wilderness Environ Med 2009; 20: 118-124.
- Pipelzadeh MH, Jalali A, Taraz M, Pourabbas R, Zaremirakabadi A. An epidemiological and a clinical study on scorpionism by the Iranian scorpion Hemiscorpius lepturus. Toxicon 2007; 50: 984-992.
- Forrester MB, Stanley SK. Epidemiology of scorpion envenomations in Texas. Vet Hum Toxicol 2004; 46: 219-221.
- de Roodt AR, García SI, Salomón OD, Segre L, Dolab JA, Funes RF, de Titto EH. Epidemiological and clinical aspects of scorpionism by Tityus trivittatus in Argentina. Toxicon 2003; 41: 971-977.
- Yilmaz F, Arslan ED, Demir A, Kavalci C, Durdu T, Yilmaz MS, Yel C, Akbulut S. Epidemiologic and clinical characteristics and outcomes of scorpion sting in the southeastern region of Turkey. Turkish J Trauma Emergency Surgery 2013; 19: 417-422.
- Duman A, Turkdogan AK, Akoz A, Avcil M, Dagli B, Canakci SE. A rare complication of scorpion venom: atrial fibrillation. Am J Emergency Med 2015.
- Chippaux JP, Goyffon M. Epidemiology of scorpionism: a global appraisal. Acta Trop 2008; 107: 71-79.
- Ghalim N, El-Hafny B, Sebti F, Heikel J, Lazar N, Moustanir R, Benslimane A. Scorpion envenomation and serotherapy in Morocco. Am J Trop Med Hyg 2000; 62: 277-283.
- Al B, Yilmaz D, Sogut O, Orak M, Ustundag M, Bokurt S. Epidemiological, clinical characteristics and outcome of scorpion envenomation in Batman, Turkey: An Analysis of 12O Cases. JAEM 2009; 8: 9-14.
- Touloun O, Slimani T, Boumezzough A. Epidemiological survey of scorpion envenomations in South Western Morocco. J Venom Anim Toxins 2001; 7: 199-218.
- Hammoudi-Triki D, Ferquel E, Robbe-Vincent A, Bon C, Choumet V, Laraba- Djebari F. Epidemiological data, clinical admission gradation and biological quanti?cation by ELISA of scorpion envenomations in Algeria: effect of immunotherapy. Trans R Soc Trop Med Hyg 2004; 98: 240-250.