ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2009) Volume 20, Issue 3
Holoprosencephaly: A Rare Complication of Maternal Hypothyroidism
1Department of Pathology, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India
2Department of TB and Chest, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India
- *Corresponding Author:
- S. M. Natu
Department of Pathology
Chhatrapati Shahuji Maharaj Medical University
(King George’s Medical University)
Lucknow-226 003
Uttar Pradesh, India
E-mail: shagufta.mufti@gmail.com
Accepted date: smnatu.natu@gmail.com
Maternal hypothyroidism is known to cause an array of complications, maternal and fetal. Some of them include infertility, abortion, still birth, pre-term labor, fetal distress, birth defects, low birth weight and low IQ. We present a case of 32-year-old multiparous woman with hypothyroidism whose pregnancy was terminated in mid-gestation because of development of holoprosencephaly. Holoprosencephaly is failure of the forebrain to divide into distinct lateral cerebral hemispheres. To the best of our knowledge this is the first case of holoprosencephaly associated with maternal hypothyroidism.
Keywords
Maternal hypothyroidism holoprosencephaly, pregnancy
Introduction
Maternal hypothyroidism causes various maternal and fetal complications like infertility, abortion, still birth, preterm labor, fetal distress, birth defects, low birth weight and low IQ. The fetus is able to produce thyroid hormones by 8-10 week gestation but prior to that time is totally dependent on maternal thyroid hormones [1]. The fetal gland becomes operational near mid-gestation [2]. We report here a singleton pregnancy with Alobar Holoprosencephaly in a 32-year-old multiparous hypothyroid woman during early pregnancy. Holoprosencephaly denotes an incomplete or absent division of embryonic forebrain into distinct lateral hemispheres. The prevalence of holoprosencephaly during embryogenesis is 1:250 and 1:16,000 in new born infants [3,4]. Holoprosencephaly has been classified into three grades of severity: Alobar Holoprosencephaly - complete absence of midline forebrain division resulting in a monoventricle and fused cerebral hemispheres. Semilobar Holoprosencephaly - incomplete forebrain division resulting in partial separation of cerebral hemispheres, typically, posteriorly and Lobar Holoprosencephaly - complete ventricular separation with focal areas of incomplete cortical division or anterior falcine hypoplasia [5].
Case Report
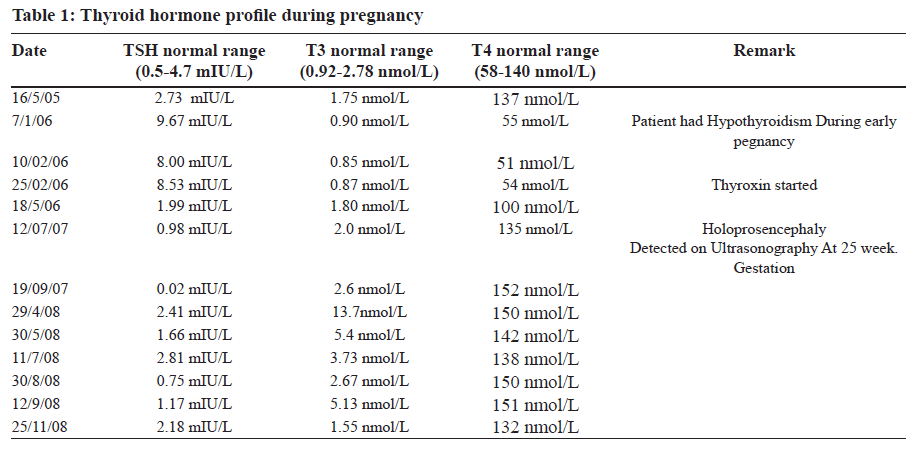
A 32-year-old multiparous woman P2+3 blood group O Rh negative presented to the Chemical Laboratory, Department of Pathology, Chhatrapati Shahuji Maharaj Medical University, Lucknow, Uttar Pradesh, India. Married for 17 years, non-consanguineous marriage, she tested negative for VDRL, HIV 1 and 2, Toxoplasma, Rubella, Cytomegalovirus and herpes simplex virus. Fasting blood glucose was normal (95 mg/dl). No history of smoking or alcohol intake. Her first pregnancy was after eight years of marriage. Result: spontaneous abortion at 15-16 week gestation. Second pregnancy in 2000: Uneventful pregnancy delivered a healthy male child. Third pregnancy 2006: Conceived six years after second pregnancy. During early pregnancy she presented with excessive weight gain (90 kg - before pregnancy 52 kg), myxoedema, hypercholesterolemia (270 mg/dl) and hypertension (144/90 mm Hg). Thyroid function test showed high Thyroid stimulating hormone (TSH), low tri-iodothyronine (T3) and low tetra- iodothyronine (T4) (Table 1). At 25-week gestation Alobar Holoprosencephaly was detected by ultrasonography. Parameters noted on ultrasound: Female fetus, head circumference 21 cm, total length 28 cm, foot length 5 cm corresponding to gestational age of 24 weeks. This pregnancy was terminated at 25- week gestation. Weight of fetus was 625 gm. Internal examination showed malformation in brain, thalami fused, no separation of cerebral hemispheres, mono-ventricle covered by thin cortex, olfactory tract not seen. These findings were suggestive of Alobar Holoprosencephaly. No malformation of any other organ was seen. Parents refused to get an autopsy done and karyotype was not done. Fourth pregnancy 2007: A year later, spontaneous abortion at six to eight-week gestation. Fifth pregnancy 2008: Uneventful, delivered a full term male child with club feet and patchy pneumonities at birth.
Discussion
Thyroid hormone is critical for normal fetal brain development, neuronal multiplication, migration and structural organization [2]. A lack of adequate maternal thyroid hormones can lead to disruption of normal brain growth and development in the fetus manifesting itself in a variety of ways such as poor cognitive development, mental retardation and cerebral palsy further in life [6,7]. In this case there are clinical features of hypothyroidism namely excessive weight gain, myxoedema, hypercholesterolemia and hypertension in early third pregnancy. Table 1 illustrates that the thyroid function tests done during this pregnancy. The results showed high TSH value and low level of thyroid hormones in early pregnancy when maternal thyroid hormones are critical for brain growth and development. Lack of thyroid hormones probably leads to development of alobar holoprosencephaly which is detected at 25-week gestation ultrasonographically. After starting thyroxin, thyroid hormone profile came to normal and remained in normal range in follow up. The causative factors of Holoprosencephaly are manifold of which chromosomal disorders account for not more than 40-50% mutationsmis- sense, non sense, deletion, insertion and frame shift [8]. Suggested non-genetic risk factors for HPE are maternal diabetes, infections during pregnancy-syphilis, toxoplasmosis, rubella, herpes, cytomegalovirus and various drugs taken during pregnancy-alcohol, aspirin, lithium, thorazine, anti-convulsants, hormones and retinoic acid [9]. These varied causes attest to the extreme heterogeneity of the disease. Since disturbance of brain development resulting in holoprosencephaly occurs before day 28 of embryonic life, basically, any factor that causes perturbation to forebrain development at the critical phase of mid to late gastrulation period of embryogenesis can result in holoprosencephaly [10]. All known causes of holoprosencephaly are ruled out in this case. The most probable factor instrumental in early pregnancy is low level of maternal thyroid hormones. Based on these findings we present an association between maternal hypothyroidism and holoprosencephaly.
To the best of our knowledge this is the first case of maternal hypothyroidism causing holoprosencephaly. Thyroid diseases are the commonest endocrinal disorders affecting woman of reproductive age group so expectant mothers should be screened for thyroid hormone status.
References
- Pop VJ, Vries DE, Baar VA, Waelkens JJ, Rooy DH, Horsten M. Maternal thyroid peroxidase antibodies during pregnancy: A marker of impaired child development. J Clin Endocrinol 1995;80:3561-6.
- Glinoer D. Thyroid regulation and dysfunction in pregnant patient: In thyroid disease. 2004.
- Golden, JA. Holoprosencephaly: A Defect in Brain Patterning. J Neuropathol Exp Neurol 1998;57:991-9.
- Ming JE and Muenke M. Holoprosencephaly: From Homer to Hedgehog. Clin Genet 1998;53:155-63.
- Myer WD, Zeman W, Palmer CG. The face predicts the brain: diagnostic significance of median facial anomalies for holoprosencephaly (arhinencephaly). Pediatrics 1964;34:256-63.
- Escobar DG, Obregon MJ, Escobar DR. Is neuropsychological development related to maternal or to maternal hypothyroxinemia. Clin Endocrinal 2000;85: 3975-87.
- Reuss ML, Paneth N, Martin PJA, Lorenz JM, Susser MB. The relation of transient hypothyroxinemia in preterm infants to neurological development at two years of age. N Engl J Med 1996;334:821-7.
- Wallis D, Muenke R. Mutation in Holoprosencephaly. Hum Mutan 2000;16:99-108.
- Kayode AO, Olamide A, Victor OU, David AO, Blessing J, Christina UO. Holoprosencephaly in a Nigerian cadáver: An original case report. J Neurosurg 2007;7:14-5.
- Alvin ST, Tse HL, Keyau SK, Patrick C, Subramaniam R, Elizabeth LP, Jessie YC, Sim LT. Holoprosencephaly: An antenatally diagnosed case series and subject review. Clin Pathol 2008;7:34-8.