ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2013) Volume 24, Issue 1
Clinical Analysis of Risk Factors and Lesion Characteristics of Coronary Artery in Patients with Coronary Heart Disease.
Shifang Ding*, Na Yang, Qing Lu, Zhigang Gong, Juquan Jiang, Zhinan Chen, Zhigang Li, Renxue Wang
Department of Cardiology, Wuhan General Hospital of Guangzhou Command, Wuhan Hubei 430070, China
- *Corresponding Author:
- Shifang Ding
Department of Cardiology
Wuhan General Hospital of Guangzhou Command
Wuhan Hubei 430070, China
Accepted date: November 01 2012
The objective of the present study is to investigate the relationship between the lesion characteristics of coronary artery and risk factors of coronary heart disease (CHD). A total of 430 patients underwent coronary angiography (CAG) were recruited from January 2008 to October 2009 and divided into CHD group (n=282) and non-CHD group (control group, n=148) according to the findings on CAG. The risk factors of CHD including smoking, hypertension, hyperlipemia and diabetes mellitus (DM) were recorded. Multivariable regression analysis was employed for the analysis of correlation between risk factors and lesion characteristics of coronary artery. The systolic pressure, pulse pressure, hypersensitive C reaction protein (hs-CRP), plasma fibrinogen and glycosylated hemoglobin (HbA1c) in the CHD group were markedly higher than those in the control group (P<0.01). Gender, age, hypertriglyceridemia, DM and elevated plasma fibrinogen are the independent risk factors of CHD (P<0.05) and also closely related to the extent and score of lesion in CHD patients. Subjects who are male or smokers, or have DM, hypertriglyceridemia or elevated hs-CRP / plasma fibrinogen have high risk for CHD.
Keywords
Coronary heart disease; risk factors; coronary angiography; Characteristics
Introduction
With the development of globalization and changes in lifestyle, coronary heart disease (CHD) has become the most common disease threatening human health. The risk factors of CHD are complex. Traditional risk factors include male sex, advanced age, smoking, family history, obesity, diabetes mellitus (DM), hyperlipemia and hypertension. Recent studies also reveal cytokines in adipose tissues, hyperhomocysteinemia and hyperuricemia as risk factors of cardiovascular diseases [1-3]. Thus, early and comprehensively interfering risk factors of CHD seems to be of great importance to reduce the incidence of cardiovascular events.
In the present study, coronary angiography (CAG) was employed to detect the characteristics of lesion coronary artery and percutaneous coronary intervention (PCI) was performed as a therapeutic strategy for CHD patients. The correlation between risk factors and lesion characteristics of coronary artery was further analyzed. Our findings may provide theoretical evidence for the early and comprehensive intervention of CHD.
Patients and Methods
Patients
A total of 430 patients who had clinical or suspected diagnosis of CHD were recruited from the Department of Cardiovascular Diseases of Wuhan General Hospital in Guangzhou Military Region. CAG was performed in all patients who were then divided into CHD group (n=282) and non-CHD group (n=148) according to findings on CAG. There were 197 males and 85 females with a mean age of 64.78±10.99 years in the CHD group and 85 males and 63 females with a mean age of 58.13±12.23 years in the non-CHD group. For patients with CHD, PCI was carried out on the basis of disease condition. Patients with incomplete medical record, concomitant severe infection, immune dysfunction or severe heart, liver, lung or kidney diseases were excluded from the present study.
Data collection
Inquiring medical history and physical examination were performed on admission. Patients were fasted for 12 h and then venous blood was collected in the morning of the second day for laboratory examinations: fasting glucose, serum cholesterol, triglycerides, high density lipoprotein cholesterol (HDLC), low-density lipoprotein cholesterol (LDLC), coagulation function and blood chemical parameters, which were determined by using an automatic biochemical analyzer.
Diagnostic criteria
1. CHD was diagnosed according to the criteria for CHD developed by WHO [4]: the diameter of at least one coronary artery or its branches is reduced by ≥50% when compared with adjacent normal vessels;
2. Hypertension was diagnosed based on the criteria for hypertension developed by WHO-ISH in 1999: systolic blood pressure (SBP) ≥140 mmHg and/or diastolic blood pressure (DBP) ≥ 90 mmHg at rest in at least two detections or presence of a history of hypertension;
3. Hyperlipemia was diagnosed according to the recommended criteria for hyperlipemia developed by the Group on Prevention and Preatment of Dyslipidemia: TC ≥ 5.72 mmol/L;TG ≥ 1.7 mmol/L; LDL ≥ 3.64 mmol/L; HDL ≤ 0.91 mmol/L;
4. DM was diagnosed based on the criteria developed by ADA [5]: Patients were previously treated with glucose lowering drugs or fasting serum glucose is ≥7.0 mmol/L in at least 2 detections;
5. Smoking: Patients have a history of smoking or the duration of smoking cessation of < 10 years is also regarded as a risk factor. The risk factors were recorded in each patient.
Calculation of pulse pressure
Blood pressure was measured on physical examination and pulse pressure was calculated as follow: pulse pressure = SBP – DBP.
Analysis of coronary artery lesion
CAG was performed with Judkins method according to the Guidelines of American College of Cardiology/ American Heart Association (ACC/AHA). CAG was done at several views (left anterior oblique, right anterior oblique and head-to-toe axial view) aiming to visualize each coronary artery. CAG was performed by an experienced cardiologist with same criteria. According to findings on CAG, patients with reduction of diameter of coronary artery by ≥50% were diagnosed as having CHD and the remaining patients served as controls (non-CHD patients).
Implantation of drug-eluting stents was done according to the standard protocol. Balloon dilatation or non-treatment surgery was performed and the stent was released. The stent was placed at the lesions and closely adherent to the vessel wall and completely covered the lesions. At the same time, anti-coagulation therapy was performed with combined aspirin, clopidogrel and heparin to minimize the thrombosis and intimal hyperplasia, which may reduce the post-operative re-stenosis and occurrence of cardiovascular events [6]. For patients with lesions at the bifurcation, stenting was done in the main artery but not in branches. Criteria for the successful treatment: the diameter of lesioned vessels was reduced by < 20% following PCI and the distal blood flow was classified as grade TIMI-3. Acute intra-operative complications were absent and no adverse cardiovascular events were observed during the hospitalization.
Determination and scoring
Main coronary arteries and their branches with reduction of diameter by ≥50% were regarded as lesioned arteries, including 1, 2 and 3 branch lesions. Lesions in both left anterior descending (LAD) artery and circumflex (LCX) artery accounted for lesions in left main coronary artery. Lesions in diagonal branch, obtuse marginal branch and acute marginal branch accounted for lesions in the main artery.
The coronary artery was classified as 4 branches: left main (LM), LAD, LCX and right coronary artery (RCA). Scoring of each branch was performed at the narrowest site: ≤49%, score 1; 50%-74%, score 2; 75%-89%, score 3, ≥90%, score 4. The final score was the sum of the score of each branch.
Statistical analysis
Statistical analysis was performed with SPSS version 13.0. Quantitative data were expressed as mean ± standard deviation (x_±s) and t test was applied for comparisons. Qualitative data were expressed as percentage. Comparisons of rates or numbers were done with chi square test. Analysis of variance was employed for comparisons among multiple groups. A value of P< 0.05 was considered statistically significant. Multivariate analysis was carried out with Logistic regression analysis and Pearson correlation analysis.
Results
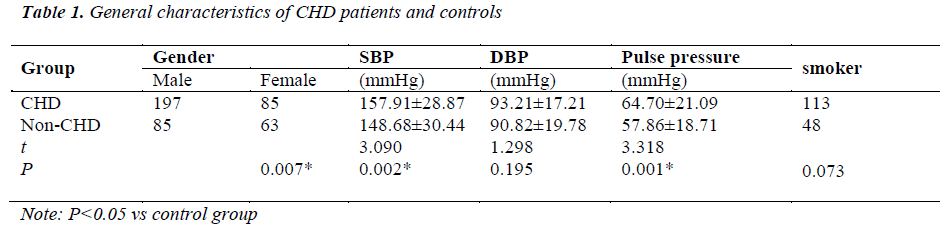
General characteristics of CHD patients and non-CHD patients
The proportion of males in CHD group was significantly higher than that in non-CHD group. The SBP and pulse pressure in CHD group were markedly increased when compared with non-CHD group (P< 0.05). (Table 1)
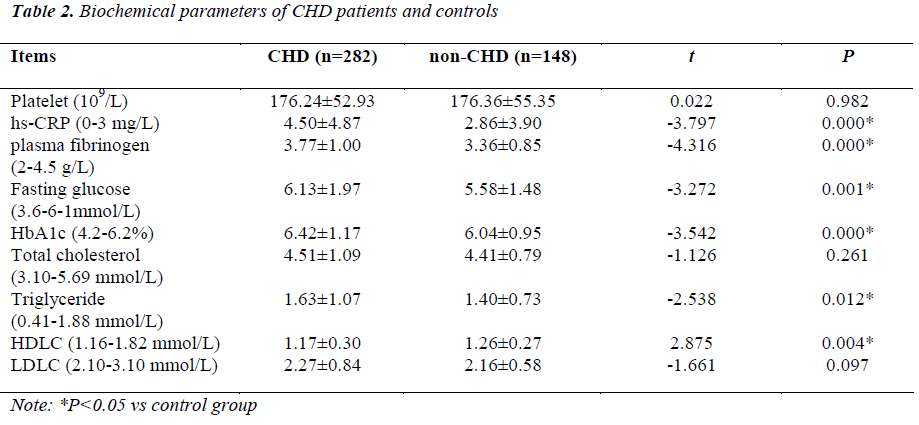
Biochemical parameters of CHD patients and non-CHD patients
In CHD group, the levels of hypersensitive C reaction protein (hs-CRP), plasma fibrinogen, fasting glucose, glycosylated hemoglobin (HbA1c) and triglyceride were dramatically different from those in non-CHD group (P< 0.05). Differences in hs-CRP, plasma fibrinogen and HbA1c between two groups were the most evident (Table 2).
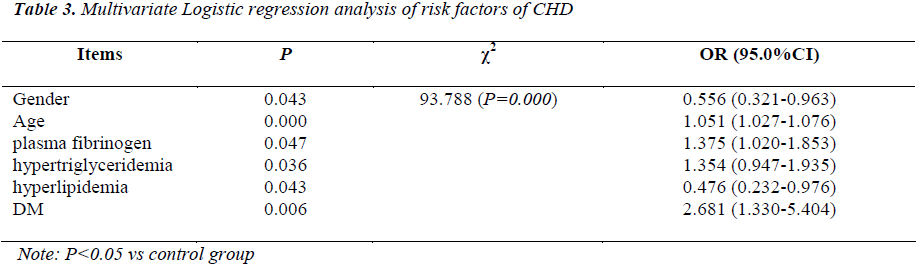
Multivariate Logistic regression analysis of risk factors of CHD
Gender, age, plasma fibrinogen, hypertriglyceridemia,hyperlipidemia and DM were the risk factors of CHD. Moreover, patients with a history of DM had a higher risk for CHD when compared with patients with other risk factors (Table 3).
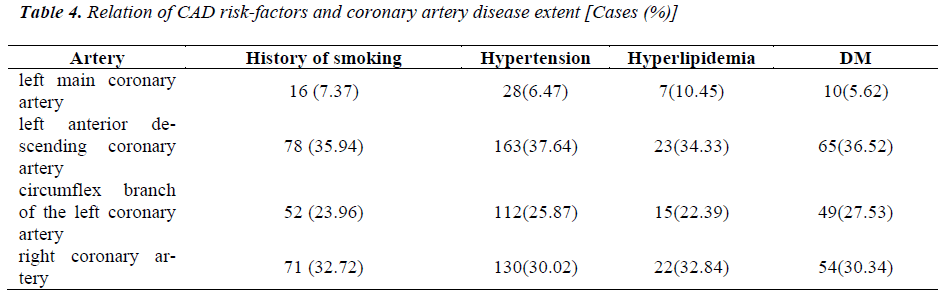
Correlation between risk factors of CHD and lesion extent of coronary artery
CHD patients with the following 4 risk factors predominantly had the involvement of left anterior descending coronary artery, followed by right coronary artery and circumflex branch of the left coronary artery (Table 4).
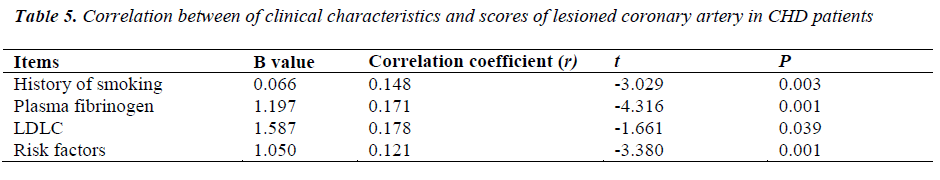
Correlation between clinical characteristics and scores of lesioned coronary in CHD patients
The history of smoking, elevated plasma fibrinogen, increase of LDLC and risk factors of CHD were related to the scores of lesioned coronary artery (Table 5)
Discussion
The etiology of CHD is complex. In recent years, epidemiology, molecular biology, animal experiments and clinical observations have demonstrated that the pathogenesis of atherosclerosis (AS) has involvement of damage to endothelial cells, oxidative stress, abnormal autoimmunity, chronic inflammation and lipid infiltration [7]. The cumulative effect of multiple risk factors promotes and aggregates the occurrence of cardiovascular events in CHD patients.
Apart from hyperlipidemia, smoking is another independent risk factor of CHD. The carbon monoxide (CO) in the smoke is inhaled and competes with hemoglobin to oxygen, which then reduces the oxygen supply to tissues, especially the myocardium. This may cause myocardial hypoxia and/or ischemia, lipid metabolism disorder and AS, and induce coronary spasm. High serum CO concentration may stimulate sympathetic nervous system leading to the massive production of transmitters including catecholamine and vasopressin, which may cause overexcitation induced damage to sympathetic nerves. In addition, a large amount of free radicals are produced during the smoking and may lead to oxidative stress of endothelial cells of coronary artery and compromise the activity of NO. The smoke can also stimulate the proliferation of vascular smooth muscle cells. Smoking may increase the oxidized low-density lipoprotein (ox-LDL) and induce the elevation of plasma fibrinogen (Fib), which then disrupts the coagulation function. The platelet aggregation is enhanced and embolus is susceptible to form. Our findings suggested that the history of smoking was related to the extent and score of lesioned coronary artery (P< 0.01).
Fib is one of important coagulation factors. In the presence of thrombin and coagulation factor VIII, Fib can transform from soluble molecule to insoluble fibrin polymer involving in the coagulation. However, sustained increase of plasma Fib may cause the imbalance between coagulation and fibrinolysis, which results in increase of blood viscosity, enhancement of coagulation of red blood cells and platelets and changes in hemodynamics and hypercoagulable state. These pathological changes may aggregate the damage to endothelial cells and promote the occurrence of clinical events related to instability of coronary atherosclerotic plaques. On the other hand, high levels pf plasma Fib and its degradation products may stimulate the proliferation and migration of vascular smooth muscle cells during the formation of AS [8]. These products can also bind to the lipoproteins in the inner membrane of macrophages, which facilitates the accumulation of lipid outside the atherosclerotic plaques. Increased plasma Fib level is also a marker of active inflammation during formation of AS. Our results revealed increase of Fib level was also an independent risk factor of CHD, which was consistent with previous studies. Thus, for patients with high risk for CHD, coagulation function should be monitored to guide the clinical anti-coagulation and thrombolytic therapy and to prevent the occurrence of CHD related events.
Hypertension, hyperlipidemia and DM are the traditional risk factors of CHD. Framingham heart study has demonstrated that increase of blood pressure is one of independent risk factors of CHD in both males and females of any age group, and the level of blood pressure is related to the continuous and gradual increased incidence of CHD[9]. In the present study, results showed the SBP and pulse pressure in the CHD group were markedly higher than those in control group (P< 0.01). This was also confirmed in Chinese epidemiological studies in which the SBP and pulse pressure were found to be positively related to the CHD. With the increase of age, the vascular intima is increasingly thickened and the elasticity of blood vessels is also compromised. The ability of vessel to dilate is reduced. Thus, the SBP increases, DBP reduces and pulse pressure elevates. Pulse pressure is an indicator reflecting the stiffness of major arteries, and has been found to be independent risk factor in the prediction of cardiac events. There is evidence showing that the increase of pulse pressure by 5 mmHg may increase the risk for CHD by 18%[10]. In the present study, multivariate analysis was employed to evaluate the role of hypertension in predicting risk for CHD, but hypertension was not included in the model. This may be attributed to that the diagnosis was specialized and the majority of patients had hypertension (P>0.05). However, patients with hypertension had severe and extensive damage to coronary artery, which further confirms the close correlation between hypertension and the extent of stenosis of coronary artery in CHD patients. Thus, to control blood pressure is still one of important ways in the treatment of CHD.
In clinical trials, statins have been applied in subjects with high risk for CHD as a measurement for primary and secondary prevention. Results have shown that the CHD related events reduced linearly, which suggests hyperlipidemia is a critical risk factor of CHD and both exhibit linear correlation. As a result of long-lasting multiple risk factors of CHD, lipid metabolism is disordered and lipid deposits in the blood vessel wall leading to AS. This process may cause damage to endothelial cells, infiltration of inflammatory cells and production of inflammatory cytokines, which further activate the activity and proliferation of inflammatory cells, and promote the production of cytokines and other inflammatory mediators. Under this condition, the synthesis of hs-CRP, a marker of inflammation, increases, leading to the increased level of serum hs-CRP. hs-CRP aggregates at the atheromatous plaques, activates complements, enhances the activity of phagocytes, induces the expression of Endothelial adhesion molecule mediating the LDL-C uptake and stimulates the expression of tissue factors on monocytes and immune regulation. These processes may initiate or promote the development of AS. Recent studies show [11- 12] the minor change in hs-CRP may predict the occurrence of life-threatening cardiovascular events even the hs-CRP is lower than the upper limit of normal. hs-CRP will reduce to the baseline level with the improvement of disease. Thus, hs-CRP not only has diagnostic value but can be used to monitor the therapeutic efficacy.
DM and impaired glucose tolerance have been identified as independent risk factors of cardiovascular diseases[13]. CHD is regarded as a complication of major vessels in DM patients. The AS in T2DM patients is more extensive and severe. There is evidence showing that the vascular complications have been present before the presence of symptoms of DM, and DM and AS share pathogenic mechanism (inflammation). DM has been considered as one of CHD risk equivalents [14]. In the present study, our findings also noted the incidence of DM in CHD patients was markedly higher than that in control group (P< 0.01). Multivariate regression analysis revealed the risk of DM patients for CHD was 2.681 folds higher than that of non-DM patients, which was consistent with previously reported. In China, a survey on heart diseases showed that about 75% of DM or pre-diabetes patients could not be diagnosed according to fasting glucose alone. In the present study, there was dramatic difference in the fasting glucose between CHD group and non-CHD group, but univariate and multivariate analyses did not present fasting glucose as a risk factor. This may be attributed to that fasting glucose may be affected by the diet and stress. For DM patients, high blood glucose level may cause damage to endothelial cells, increase the production of oxygen free radicals, promote the aggregation of platelets and thrombosis, stimulate the aggregation of multiple inflammatory cells, and increase the expression of growth factors and elevate the deposition of extracellular matrix, all of which involve in the re-stenosis after PCI.
Taken together, multiple risk factors are critical for the prediction and early intervention of CHD and thus, primary and secondary prevention is required for patients with high risk for CHD. However, the sample size is still small and studies with larger sample size are required to screen the risk factors of CHD. The limitation of the study is that the sample size is relatively small, and the study group and control group is not mathed well in age and gender, because they are divided according to the situation whether they underwent coronary angiography.
References
- Kilbourne AM, Brar JS, Drayer RA, Xu X, Post EP. Cardiovascular disease and metabolic risk factors in male patients with schizophrenia, schizoaffective disorder and bipolar disorder. Psychosomatics 2007;48(5): 412-417.
- Yang X, So WY, Kong AP, Ma RC, Ko GT, Ho CS, Lam CW, Cockram CS, Chan JC, Tong PC. Development and validation of a total coronary heart disease risk score in type-2 diabetes mellitus. Am J Cardiol 2008; 101(5): 596-601.
- Prugger C, Heidrich J, Wellmann J, Dittrich R, Brand SM, Telgmann R, Breithardt G, Reinecke H, Scheld H,Kleine-Katthöfer P, Heuschmann PU, Keil U. Trends in Cardiovascular Risk Factors Among Patients With Coronary Heart Disease: Results From the EUROASPIRE I, II, and III Surveys in the Münster Region.Dtsch Arztebl Int 2012; 109(17): 303-310
- International Society and Association of Cardiology, Joint Thematic Group of World Health Organization on Standardization of Clinical Nomination. Nomination and diagnostic criteria for ischemic heart diseases. Chin J Internal Med 1981; 20: 254-255
- American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care 2012; 35 Suppl 1: S64-71.
- Colombo A, Orlic D, Stankovic G, Corvaja N, Spanos V, Montorfano M, Liistro F, Carlino M, Airoldi F,Chieffo A, Di Mario C. Preliminary observations regarding angiographic pattern of restenosis after rapamycin-eluting stent implantation. Circulation 2003;107: 2178-2180.
- Tabas I, Williams KJ, Boren J. Subendothelial lipoprotein retention as the initiating process in atherosclerosis: update and therapeutic implications. Circulation 2007; 116: 1832-1844
- Renner W, Cichocki L, Forjanics A, Köppel H, Gasser R, Pilger E. G-455A polymorphism of the fibrinogen beta gene and deep vein thrombosis. Eur J Clin Invest 2002; 32: 721-722.
- O'Donnell CJ, Elosua R. Cardiovascular risk factors. Insights from Framingham Heart Study. Rev Esp Cardiol 2008; 61: 299-310..
- Yang ZK, Shen WF, Weng DB. Relationship between pulse pressure and incidence of coronary artery disease in hypertensive patients. Chin J Cardiol 2002; 30: 325-327.
- Bansal S, Ridker PM. Comparison of Characteristics of Future Myocardial Infarctions in Women With Baseline High Versus Baseline Low Levels of High-Sensitivity C-Reactive Protein. Am J Cardiol 2007; 99:1500-1503.
- Wang TJ, Gona P, Larson MG, Tofler GH, Levy D, Newton-Cheh C, Jacques PF, Rifai N, Selhub J, Robins SJ, Benjamin EJ, D'Agostino RB, Vasan RS. Multiple Biomarkers for the Prediction of First Major Cardiovascular Events and Death. N Engl J Med 2006; 355:1472-1473.
- Rodriguez BL, Curb JD, Burchfiel CM, Huang B, Sharp DS, Lu GY, Fujimoto W, Yano K. Impaired glucose tolerance, diabetes, and cardiovascular disease riskfactor profiles in the elderly. The Honolulu Heart Program.Diabetes Care 1996; 19: 587-590.
- National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). Third Report of the National CholesterolEducation Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) final report. Circulation 2002; 106: 3143-3421.