ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2014) Volume 25, Issue 1
Case report: Atypical Presentation of Tropical Pulmonary Eosinophilia as a Lung Mass.
Department of TB & Chest, Rajan Babu Institute of Pulmunary Medicine and Tuberculosis, G.T.B Nagar, Kwingsway Camp, Delhi-110009, India
- *Corresponding Author:
- Suresh Kumar
Department of TB & Chest
Rajan Babu Institute of Pulmunary Medicine and
Tuberculosis, G.T.B. Nagar, Kwingsway Camp
Delhi-110009, India
Accepted date: October 19, 2013
Citation: Suresh Kumar, Praveen Gautam. Case report: Atypical Presentation of Tropical Pulmonary Eosinophilia as a Lung Mass. Biomedical Research 2013; 25 (1): 135-137.
Tropical pulmonary eosinophilia (TPE) most commonly affects people living in the tropics, especially those in Southeast- Asia, India and certain parts of China and Africa. TPE, which results from immunologic hyper-responsiveness to human filarial parasites. TPE is characterized by paroxysmal cough, dyspnea and wheezing, diffuse reticulonodular infiltrates in the chest radiographs and marked peripheral blood eosinophilia. Leucocytosis with an absolute increase in eosinophils in the peripheral blood is the hallmark of TPE. Other criteria for the diagnosis of TPE include high titres of antifilarial antibodies, raised serum total IgE >1000 ku/L and a favourable response to the antifilarial agent, diethyl-carbamazine. If left untreated or treated late, may be lead to long-term sequelae of pulmonary fibrosis or chronic bronchitis with chronic respiratory failure. The complications can be prevented by early diagnosis and treatment of patient.
Keywords
Tropical pulmonary eosinophilia, Diethyl-carbamazine
Introduction
Weingarten first described the condition of spasmodic bronchitis associated with leucocytosis, marked eosinophilia and a dramatic response to organic arsenicals in India as TPE [1]. Cases of tropical pulmonary eosinophilia were initially recorded in India but the disease is now known to occur throughout the world. Ill defined raticulonodular infiltrates with mottled appearance are the characteristic radiological findings seen in TPE. Various atypical presentations of Tropical Pulmonary Eosinophilia such as cavitation [2-4]. pleural effusion and pneumonitis [5] have been reported. In view of its rarity we present a case of tropical pulmonary eosinophilia which radiologically present as lung mass in the right lower zone.
Case Report
A 20 years old female, presented with symptoms of paroxysmal nocturnal cough with scanty mucoid sputum, fever and breathlessness on exertion of 6 month duration and pain in the chest of 2 week duration. Six month previously she had consulted a general practitioner, who diagnosed pulmonary tuberculosis on the basis of symptoms and radiological evidence of consolidation in the right lower zone with small patchy area of opacification in the left lower zone. She was given antibiotics for 2 week and antituberculous treatment. Patient took the drugs regularly until she was admitted to this institute. She showed neither symptomatic relief nor radiological improvement during this period.
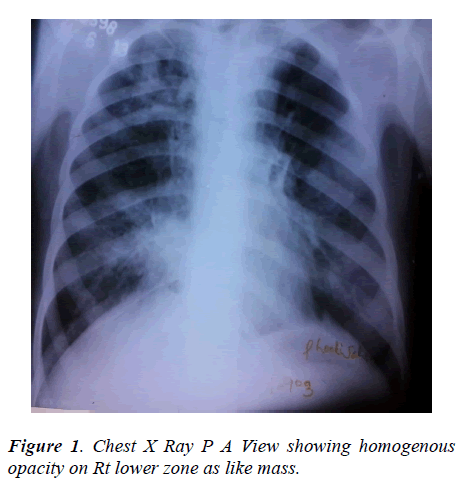
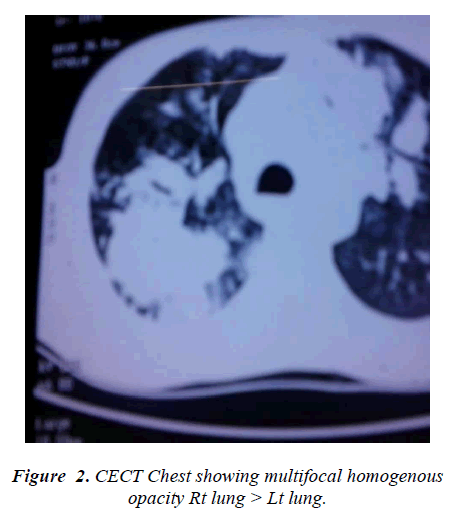
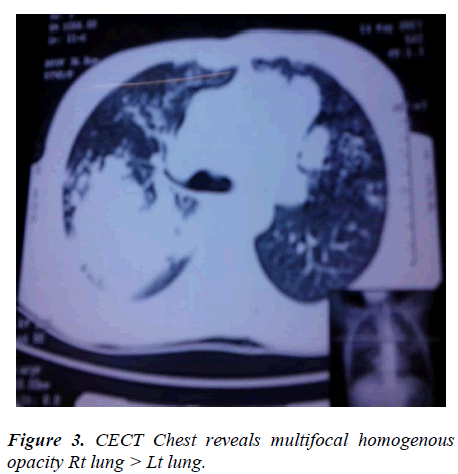
General examination revealed nothing important. Examination of respiratory system showed dullness on percussion on right lower chest and diminished breath sounds with fine crackles at right lower chest without evidence of mediastinal shift and bilateral ronchi were also heard, the total leucocytes count was 10 x10 9/L, DLC- polymorphs 57%, lymphocytes 10%, eosinophils 29%, monocytes 04% and absolute eosinophil counts was 3.22 x 109 /L. Urine and stool examination showed no abnormality. Her sputum culture was repeatedly negative for pyogenic, AFB and fungus and cytology was negative for malignant cells and total IgE was 16428 u kua/L.The chest x-ray showed a homogenous opacity on right lower zone (fig. 1) and patchy area of opacity on left lower zone. Her CECT chest revealed multifocal patchy area of consolidation involving bilateral lung upper lobes right>left and small 5 mm cavitation in the left upper lobe consolidation and bilateral hilar lymphnode were also noted (fig. 2-3). Indirect haemagglutination test for filaria was highly positive in a titre of 1:266 and fibreoptic bronchoscopy was non conibutory.
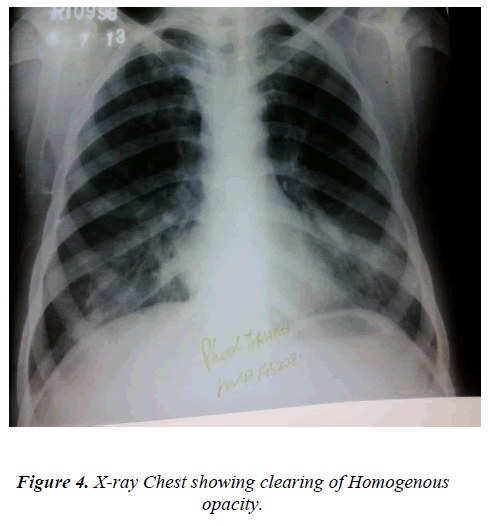
The patient was treated with 300mg of diethyl carbamazine orally in three divided doses daily for three week and bronchodilator also given. After three week of treatment her total leucocyte count was 9.3 x109/L, DLC- polymorphs 60, lymphocytes 27, eosinophils 08, monocytes 05 and absolute eosinophil count .74x109/L and chest xray showed appreciable clearing of the shadows (fig. 4). During this period no antibiotics or antituberculous drugs were prescribed.
Discussion
Radiologicaly presentation of TPE is may be normal or it may present as the typical appearance of bilateral indefinite mottling distributed in both lung fields and involving the middle and lower zones [6]. Radiological presentation of tropical pulmonary eosinophilia as a lung mass is rare. Chaudhary et al [7] also reported an unusual case of tropical pulmonary eosinophilia presenting with an area of pneumonic consolidation 3-4cm in diameter in the right mid zone with increased peripheral blood eosinophil count. This patient responded to three week of treatment with diethyl carbamazine. Our patient was initially misdiagnosed as having tuberculosis but showed no response to antituberculous treatment. Lesion producing a similar radiological picture like tuberculosis, pneumonia, lung abscess and malignancy were excluded in our patient with relevant investigations.
After scrutiny of blood investigation patient was diagnosed as suffering from tropical pulmonary eosinophilia and this diagnosis was supported by complete haematological, radiological investigations and symptomatic response and cure to diethyl carbamazine without the addition of any antibiotics and antitubercular drugs.
References
- Weingarten RJ. Tropical eosinophilia. Lancet 1943;1: 103-105.
- Menon NK Tropical eosinophilia-atypical manifestation. Indian J Chest Dis 1963; 5; 231-236.
- Viswanathan R. Pulmonary eosinophilosis. Q J Med 1948; 17; 257-270.
- Nath J, Jain VK. Atypical presentation of pulmonary eosinophilia. Indian J Chest Dis Allied Sci 1978; 20; 141-144.
- Mital OP, Someswar Rao M, Prasad, et al. Tropical pulmonary eosinophilia. Unusual presentation. Indian J Chest Dis 1975; 17: 135.
- Udwadia FE. Tropical eosinophilia :a review. Respir Med 1993; 87: 17.
- Chaudhary BS, Gupta PK, Gupta PR. Tropical pulmonary eosinophilia: an unusual presentation. Indian J Chest Dis Allied Sci 1978; 20; 139-140.