ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2011) Volume 22, Issue 1
Assessment of Autonomic Nervous Activity in Chronic Liver Disease
Study of autonomic nervous system activity in chronic liver disease has aroused great inter-ests due to its increasing prevalence due to various etiologies. The present study was under-taken to assess the autonomic nervous system activity in chronic liver disease patients by five standard autonomic function tests. Forty patients (20 with alcoholic liver disease and 20 with non- alcoholic liver disease) and 40 normal healthy age sex matched controls were re-cruited in the study. Statistical analysis comprised student’s “t” test. Thirty out of the 40 pa-tients (75%) were found to have autonomic dysfunction. Fourteen out of 30 patients (46.67%) had only parasympathetic damage and 16 out of 30 (53.53%) had combined sym-pathetic and parasympathetic damage. Eighty percent of the alcoholic liver disease patients and 70 % of the non- alcoholic liver disease patients showed autonomic dysfunction. In con-clusion, autonomic nervous dysfunction is present in significant number of patients with chronic liver disease. Overall; the parasympathetic impairment was more frequently pre-sent in chronic liver disease patients than sympathetic impairment . Autonomic dysfunction is found with comparable frequency in alcoholics and non-alcoholics suggesting that chronic liver disease, irrespective of etiology, contributes to autonomic dysfunction. The clinical im-plication of our study is that keeping in view the significant prevalence of autonomic dys-function caution should be exercised while managing chronic liver disease patients as cir-rhotic cardiomyopathy can be unmasked by surgical intervention.
Keywords
Autonomic dysfunction, chronic liver disease, autonomic function tests
Introduction
Autonomic nervous system (ANS) activity is influenced by various physiological and pathological conditions. Au-tonomic neuropathy is well described in Diabetes melli-tus, cerebrovascular disease, spinal cord lesions, Shy Drager syndrome and with use of certain drugs [1]. Currently, study of ANS activity in chronic liver disease (CLD) has aroused great interests due to reports on role of autonomic dysfunction in prognosis of CLD patients and increasing prevalence of CLD due to various etiologies.
The most common causes of chronic liver disease in gen-eral order of frequency are chronic hepatitis C, alcoholic liver disease (ALD), non-alcoholic steatohepatitis, chron-ic hepatitis B, autoimmune hepatitis, sclerosing cholangi-tis, primary biliary cirrhosis, hemchromatosis and Wil-son’s disease [2]. In India, the prevalence of CLD is in-creasing due to various etiologies. 2% of the total Indian population is HCV carrier. There are an estimated 43-45 million HBsAg carriers and, among them 10-12 million also have HBeAg [3,4]. Prevalence of ALD is also increasing due to increasing trend of alcohol consumption [5,6].
CLD is accompanied by a number of circulatory changes including impairment of cardiovascular autonomic re-flexes, related in part to an autonomic neuropathy. As in diabetes, autonomic dysfunction in CLD results in inade-quate response to stressful events like sepsis and hemor-rhage [7],[8]. So the possible role of autonomic nervous activity status in management of CLD patients is being recognized nowadays.
In India very few studies regarding autonomic dysfunc-tion in CLD have been conducted. Therefore this study was planned primarily to assess the extent of autonomic dysfunction in CLD and to study the relation between underlying etiology of CLD and the autonomic dysfunc-tion, if any.
Materials and Methods
The study was conducted on 40 patients with chronic liver disease (20 alcoholic liver disease and 20 non- alcoholic liver disease) and 40 age-sex matched controls in the De-partment of Physiology, Government Medical College and Guru Nanak Dev Hospital Amritsar, India.
The diagnosed cases of CLD, based on, clinical examina-tion, raised liver function tests for >6 months [2] and ultrasound findings were recruited in the study. All patients belonged to Child’s Grade B [9]. Subjects with a history of diabetes mellitus, heart disease or who were on medication likely to influence the interpretation of the autonomic tests such as diuretics or beta-blockers were excluded from the study. Forty normal, healthy, age sex matched controls were recruited from the local popula-tion. Both cases and controls gave informed consent and clearance from institutional ethics committee was obtained. A detailed history was taken from these subjects and a thorough physical examination including general physical and neurological, was carried out. All the sub-jects were subjected to the five standard autonomic function tests. Heart rate response to valsalva manoeuvre, heart rate ( R-R interval ) variation during deep breathing and immediate heart rate response to standing tests the parasympathetic system while blood pressure response to sustained hand grip and blood pressure response to standing tests the sympathetic system.
Heart rate response to Valsalva manoeuvre.
The test was performed by the subject, blowing into the mouth piece attached to a manometer and holding it to a pressure of 40 mmHg for 15 seconds while a continuous electrocardiogram was recorded. The manoeuvre was performed 3 times at one minute intervals. The result was expressed as: Valsalva ratio= Longest R-R interval after the manoeuvre / Shortest R-R interval during the manoeuvre The mean of the three valsalva ratios was taken as the final result.
Heart rate ( R-R interval ) variation during deep breathing. (Deep breathing test)
The subject was asked to breath deeply at 6 breaths/min (5 seconds ‘in’ and 5 seconds ‘out’) for one minute. ECG was recorded throughout the period of deep breathing and onset of each inspiration and expiration was marked on ECG paper. The maximum and minimum R-R intervals during each breathing cycle were measured with a ruler and converted to beats/min. The results of the test were expressed as the mean of the difference between maxi-mum and minimum heart rates for the six measured cy-cles in beats/min.
Blood Pressure response to sustained hand grip.
In this test the blood pressure of the subject was taken three times before the manoeuvre. The maximum voluntary contraction was first determined using a handgrip dynamometer. Handgrip was then maintained at 30% of their maximum for as long as possible upto 5 min. BP was measured at 1 min intervals during the handgrip. The result was expressed as the difference between the highest diastolic blood pressure during handgrip exercise and the mean of the three diastolic blood pressure readings before the test.
Immediate heart rate response to standing ( 30:15 Ratio)
The test was performed with the subject lying quietly on a bed while heart rate was being recorded continuously on an electrocardiogram (BPL Cardiart 108T/MK-VI ) The subject was then asked to stand unaided and the point at starting to stand was marked on ECG paper. The shortest R-R interval at or around 15th beat and the longest R-R interval at or around 30th beat after starting to stand were measured with a ruler. The characteristic HR response was expressed as 30:15 ratio.
Blood pressure response to standing
In this test the subject’s blood pressure was measured with a sphygmanometer while he was lying quietly and one minute after he was made to stand up. The postural fall in blood pressure was taken as the difference between the systolic pressure lying and systolic pressure standing. The test was repeated three times and the mean was calculated.
The subjects were briefed about these five standard auto-nomic function tests. Self demonstration of the tests was done to make them conversant with the procedure and to remove apprehension regarding the tests, if any.
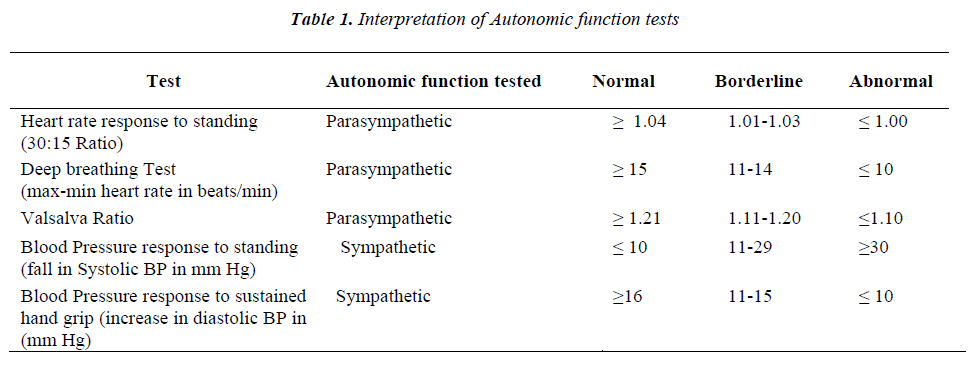
Interpretation of tests was based on guidelines of Ewing and Clarke [10]. (Table 1). Subject was labeled as normal, if none of the tests was abnormal; with early parasympa-thetic damage if results of one of the three tests of para-sympathetic function was abnormal; with definite para-sympathetic damage if two or more parasympathetic tests were abnormal; and with combined parasympathetic and sympathetic damage, if in addition to parasympathetic damage, at least one of the two sympathetic function tests was abnormal. The borderline tests were interpreted as normal [11]. The results of the five standard autonomic tests in patients and controls were compared using the student’s t-test.
'Results and Discussion
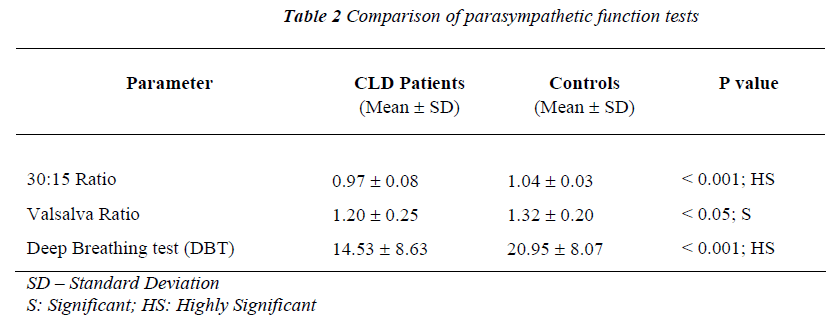
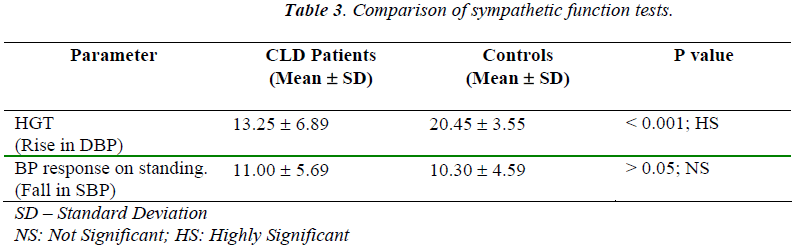
Autonomic dysfunction is an extrahepatic manifestation of CLD. Only a few Indian studies regarding this subject have been published [12,13]. In our study, the comparison of mean values of standard autonomic function tests in controls and patients (Table 2 and Table 3) shows that highly significant change in autonomic nervous system activity is seen in CLD patients. Amongst the parasympa-thetic function tests the difference between CLD patients and controls for the 30:15 ratio and deep breathing test was highly significant (p value < 0.001). Amongst the sympathetic function tests the difference between CLD patients and controls for the diastolic BP rise during hand grip test was highly significant (p value < 0.001). 30:15 ratio was the most frequently abnormal test in our study.
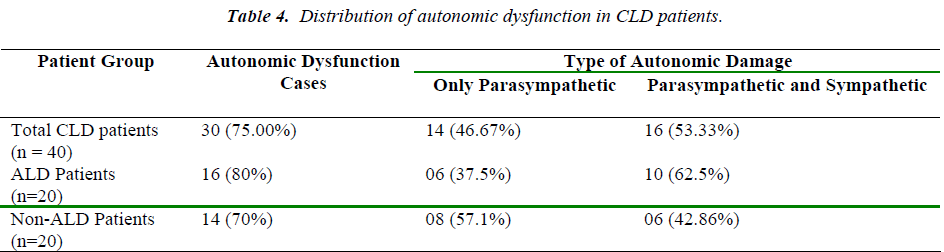
The distribution of autonomic dysfunction in various groups of CLD (Table 4) shows that overall in our study, 30 out of the 40 CLD patients (75%) were found to have autonomic dysfunction. Fourteen out of 30 CLD patients (46.67%) had only parasympathetic damage and 16 out of 30 (53.33%) had combined sympathetic and parasympa-thetic damage. None of the subjects had sympathetic dys-function alone. Overall parasympathetic impairment was more than sympathetic impairment in CLD patients.
Gentile et al found autonomic neuropathy in 60 % of the 113 cirrhotic. Seventy one percent of alcoholics and 57 % of non- alcoholics were affected. The parasympathetic impairment was significantly more than sympathetic im-pairment [14]. Dillon et al also detected abnormal cardio-vascular autonomic reflexes in 60% of the 70 CLD pa-tients [15]. Study by Bajaj et al on 20 CLD patients of Indian origin showed that 16 out of 20 (80%) of the CLD patients had evidence of autonomic dysfunction. Of these, 8 (40%) had combined parasympathetic and sympathetic damage and 8 (40%) had parasympathetic damage only [12]. Our results are in accordance with these studies.
In our study autonomic dysfunction is found with compa-rable frequency in alcoholics (80%) and non-alcoholics (70%) suggesting that liver damage, irrespective of etiol-ogy, can contribute to autonomic dysfunction. Similar findings were drawn by MacGilchrist and Reid in their study on 20 cirrhotics [16].
The present study differs from that of Barter and Tanner [10]. In their study on 30 CLD subjects parasympathetic damage was reported in 16% and combined parasympa-thetic and sympathetic damage in additional 20%.The lower frequency of autonomic dysfunction in their study could be due to the fact that they included only 14 sub-jects with alcoholic liver disease while the rest had an alcohol dependence problem only. Our study differs from that of Hendrickse et al also [17]. They reported vagal neuropathy in 45% of the 60 CLD patients. The lower frequency of autonomic neuropathy reported is due to the fact that 57 out of 60 CLD patients belonged to Child class A. In our study all patients belonged to Child class B.
The findings of our study have clinical implications. The systemic circulation in patients with CLD is hyperdy-namic with an increased cardiac output and heart rate and a reduced systemic vascular resistance caused by humoral and nervous dysregulation.[18,19]. It is suggested that autonomic neuropathy plays a role in development of this hyperdynamic circulation in CLD [20,21]. Nowadays there is easy availability of the transjuglar intrahepatic portal systemic shunt (TIPS), peritoneal venous shunt-ing, liver transplantation to the large number of CLD pa-tients, even in the developing countries like India. Keep- ing in view the significant prevalence of autonomic dys-function, as suggested in our study, caution should be exercised during these stressful procedures as the cirrhotic cardiomyopathy , an entity different from the heart mus-cle disease , can be unmasked by physical or pharmacol-ogical strain [22]. Autonomic function status may be eva-luated before going in for the above said procedures.
Finally, considering the possibility of adverse prognostic implications of the autonomic neuropathy in CLD and clinical significance of cirrhotic cardiomyopathy, caution may be exercised while managing CLD patients.
References
- Bannister R. Autonomic failure. Oxford University press, 1983: 4.
- Pratt DS, Kaplan MM: In: Harrison’s Principles of In- ternal Medicine. 16th ed. McGraw-Hill, New York 2005; pp 1813-1816.
- Medicine. 19th ed. M/S Banarsidas Bhanot, Jabalpur 2007; pp: 123-301
- Singh H, Aggarwal R, Singh RL et al. Frequency of infection by hepatitis B virus and its surface mutants in a northern Indian population. Indian J Gastroenterol 2003; 22(4): 132-137.
- Lal B, Singh G. Alcohol consumption in Punjab. Indian J Psychiatry 1978; 20(3): 212-216.
- Das SK, Balakrishnan V, Vasudevan DM. Alcohol: its health and social impact in India. Natl Med J India. 2006; 19(2):94-99.
- Lunzer MR, Manghani KK, Newman SP et al . Impaired cardiovascular responsiveness in liver disease. Lancet 1975; ii: 382-385.
- Thuluvath PJ, Triger DR. Autonomic neuropathy and chronic liver disease. Q J Med 1989; 72: 737-747.
- Pugh RNH, Murray-Lyon IM, Dawson JL et al. Tran- section of the oesophagus for bleeding oesophagial varices. Br J Surg 1983; 60: 646-649.
- Ewing DJ, Clarke BF. Diagnosis and management of diabetic autonomic neuropathy. Br Med J 1982; 285: 916-918.
- Barter F, Tanner AR. Autonomic neuropathy in an alcoholic population. Postgrad Med J 1987; 63: 1033-1036.
- Bajaj BK, Agarwal MP, Ram BK . Autonomic neu- ropathy in patients with hepatic cirrhosis. Postgrad Med J 2003; 79: 408-411.
- Khosla SN, Sanyal S, Nand N. Autonomic tests and clinical significance of dysautonomia in chronic liver disease. J Assoc Physicians India 1991 ; 39 : 924-926.
- Gentile S, Marmo R, Peduto A et al. Autonomic neu- ropathy in liver cirrhosis: relationship with alcoholic aetiology and severity of the disease. Ital J Gastroen- terol 1994; 26(2): 53-58.
- Dillon JF, Plevris JN, Nolan J et al. Autonomic func- tion in cirrhosis assessed by cardiovascular reflex tests and 24-hour heart rate variability. Am J Gastroenterol 1994; 89: 1544-1547.
- MacGilchrist AJ, Reid JL. Impairment of autonomic reflexes in cirrhosis. Am J Gastroenterol 1990; 85: 288-292.
- Hendrickse MT, Thuluvath Pj, Triger DR. Natural his- tory of autonomic neuropathy in chronic liver disease. Lancet 1992; 339:1462-1464.
- Moller S, Henriksen JH. Cirrhotic cardiomyopathy: a pathophysiological review of circulatory dysfunction in liver disease. Heart 2002; 87(1): 9-15.
- Moller S, Henriksen JH. Cardiovascular complications of cirrhosis. Gut 2008; 57(8): 1181-1182.
- Szalay F, Marton A, Keresztes K et al. Neuropathy as an extrahepatic manifestation of chronic liver diseases. Scand J Gastroenterol suppl 1998; 228: 130-132.
- Dumcke CW, Moller S. Autonomic dysfunction in cir- rhosis and portal hypertension. Scand J Clin Lab Invest 2008; 68(6): 437-447.
- Henriksen JH, Moller S. Cardiac and systemic haemodynamic complications of liver cirrhosis. Scand Car- diovasc J 2009; 14: 1-8.