ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 4
The efficacy of upper and lower airway-combined therapy in treating 103 cases of allergic rhinitis
Department of Otolaryngology, The First Affiliated Hospital of Xinjiang Medical University, Urumqi, China
- *Corresponding Author:
- Hua Zhang
Department of Otolaryngology
The First Affiliated Hospital of Xinjiang Medical University, China
Accepted date: September 27, 2016
This study aims to investigate the significance of Upper And Lower Airway-Combined Therapy (ULACT) by comparing the treatment protocols for pure Allergic Rhinitis (AR) and AR associated with lower airway inflammation. A total of 103 cases of AR that were diagnosed in a clinic service were divided according to their association with lower airway inflammation into three different groups: group A patients were diagnosed with pure AR, group B patients with AR associated with airway hyperreactivity, and group C patients with AR associated with asthma. Each patient group received a different treatment protocol. Group A patients received fluticasone propionate nasal spray, group B patients received fluticasone propionate nasal spray and 100 μg salmeterol fluticasone inhalant, and group C patients received fluticasone propionate nasal spray and 250 μg salmeterol fluticasone inhalant. The efficacy of each treatment protocol was then assessed. The administered treatment in these three groups achieved varying degrees of efficacy. The efficacy of the treatment in group A was significantly higher than that of the treatment provided to groups B and C (P<0.05). The combination of fluticasone propionate and salmeterol fluticasone showed significant effectiveness in controlling the short-term symptoms of group C patients. AR should, therefore, be diagnosed as early as possible or at least, its association with lower airway inflammation excluded. Correct standard treatment protocols could decrease the rate of improper medical treatment and effectively control topical steroid utilization.
Keywords
Allergic rhinitis, Fluticasone propionate, Airway hyperreactivity, Asthma
Introduction
Allergic Rhinitis (AR) is a disease that involves allergic inflammation of the nasal mucosa that is mediated by immunoglobulin E. Its prevalence has progressively and significantly increased over the past 30 years. Previous studies carried out in the western regions of China have shown a high prevalence of AR in Urumqi, NW China. A telephone survey on the prevalence of AR that was conducted in 11 cities showed that Urumqi had the highest prevalence of AR. Presently, there is no known effective way to inhibit AR’s continuous upward trend worldwide.
A study found that nasal inflammation increases the risk of male systolic pressure [1]. Furthermore, its inflammatory lesions are associated with many other diseases, among which, lower airway inflammation is the most common. According to the physiological characteristics of the upper and lower airways, certain scholars theorized that “diseases in the upper and lower airways should be treated integratedly” [2]. Recently, studies on the correlation between the upper and lower airways have increased to include basic studies on their clinical links, similar allergenic effects, lipoxin B4, as well as other biological studies. Increasing evidence suggests that AR is closely related to lower airway inflammation [3-6] and that more studies should be focused on the interaction between the upper and lower airways.
A previous observational study on the relationship between AR, non-AR, and asthma followed-up more than 6000 subjects, mostly from Western Europe, and found that AR and non-AR were both risk factors for asthma [7]. The combination of many domestic and foreign studies led to the conclusion that more than 50% of patients with bronchial asthma also suffered from AR [8,9] and that the risk of patients with AR developing asthma is eight times greater than normal [10]. It has also been reported that many patients with AR also exhibit characteristics of non-specific Bronchial Hyperreactivity (BHR) [2]. Currently, research on the relationship between the two is ongoing. Detailed information about the treatment is still inadequate. This might be because the upper and lower airways traditionally belong to the disciplines of otolaryngology and respiratory systems, respectively. The concept of combined therapy has already been developed, but its application still has certain limitations. To address this gap in the scientific knowledge, we designed Upper and Lower Airway-Combined Therapy (ULA-CT) protocols for our patients. The aims of the present study were to evaluate the performance of ULA-CT, add to the current scientific knowledge, and provide a reference for clinical practice.
Materials and Methods
Participant selection
A total of 103 patients with AR who visited the Department of Otolaryngology at the First Affiliated Hospital of Xinjiang Medical University, from May to August 2012, were enrolled in this study. AR was diagnosed according to the criteria of Allergic Rhinitis and Its Impact on Asthma (ARIA) and the Global Initiative for Asthma (GINA) guidelines. Patients were included if they fulfilled the following criteria: i) they were between 8-60 years of age, ii) they did not have nasal and lung space-occupying lesions or a surgical history, iii) they did not have any systemic immune-deficiency disease, and iv) they had a positive allergen skin prick test result. Skin prick, nasal resistance, pulmonary function, and bronchial provocation/ expansion tests were performed on all study participants. They were also checked for rhinitis and for asthma using a scoring system. This study was conducted in accordance with the declaration of Helsinki. This study was conducted with approval from the Ethics Committee of Xinjiang Medical University. Written informed consent was obtained from all participants.
Grouping and treatment
All patients underwent bronchial provocation/expansion tests, and nasal endoscopy. The signs-symptoms scoring were performed. A rhinitis evaluation form using the standard rhinitis signs and symptoms rating scale was used [11]. The Asthma Control Questionnaire (ACQ) designed by Juniper, the Canadian epidemiologist and biostatistics expert was used to determine the severity of asthma in the study participants. Five of the seven questions on the ACQ were used in the present study. The questions were selected based on 10 asthma-related symptoms chosen by 100 asthma experts.
Patients were grouped and received specific treatment protocols according to their test and scoring results. Group A (37 cases with pure AR,) received fluticasone propionate nasal spray and nasal irrigation, group B (35 cases with AR and BHR) received fluticasone propionate nasal spray, nasal irrigation, and salmeterol fluticasone inhalant (100 μg/5 μg), and group C (31 cases with AR and asthma) received fluticasone propionate nasal spray, nasal irrigation, and salmeterol fluticasone inhalant (250 μg/5 μg).
Data collection
After receiving treatment for 1-3 months, patients were followed up and their results compared. The clinical manifestations, signs, and auxiliary examination results of the three groups on the first clinic visit and at one and three months after treatment were compared in detail. For analysis purposes, the symptoms were classified as none, mild, moderate, and severe and assigned numerical scores of 0, 1, 2, and 3, respectively.
Statistical analysis
SPSS (19.0) statistical software was used for the analysis. The measurement data were analysed using the t-test, while the intergroup comparison of the count data was assessed using the paired t-test. P values less than 0.05 were considered to be statistically significant.
Results
Rhinitis symptoms’ scores
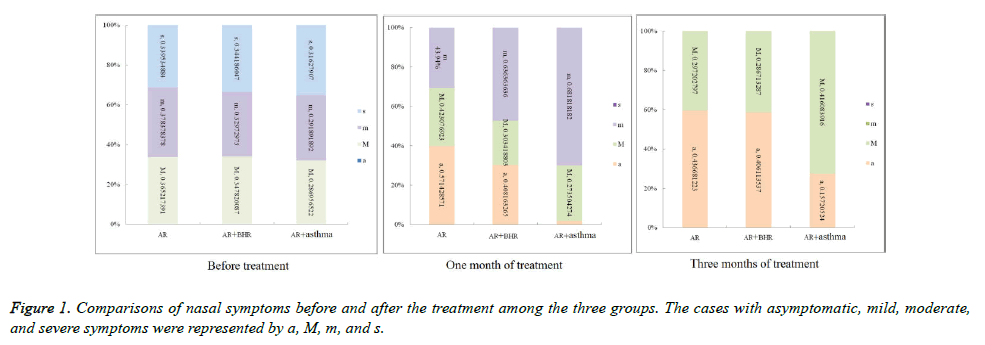
In group A, after one month of treatment, the severe symptoms (sneezing, nasal congestion, runny nose, and nasal itching) disappeared. The mild and moderate symptoms gradually decreased. After three months of treatment, the proportion of asymptomatic cases increased and the moderate symptoms disappeared. Compared with group A, the proportion of moderate symptom cases in group B after one month of treatment was higher, and that of the asymptomatic cases was lower. After three months of treatment, the proportion of moderate and asymptomatic cases in group B were similar to those of group A. Group C patients also experienced a curative effect; after one month of treatment, their severe symptoms disappeared, but the proportion of mild and moderate symptom cases were higher than those of groups A and B. After three months of treatment, the proportion of mild symptom cases in group C was the highest of the three groups, but that of the moderate symptom cases was the same as those of groups A and B (Figure 1).
Rhinitis sign scores
The changes in the sign scores of patients followed the same trend as those of the symptoms. The nasal signs significantly improved by the one-month (sign 1) and three-month (signs 3) follow-up visits, and the sign scoring differences before and after the treatment were statistically significant (P<0.05) (Table 1).
| Paired differentiating difference | |||||||
|---|---|---|---|---|---|---|---|
| Mean | SD | SD of mean | 95% CI (Lower limit) | 95% CI (Upper limit) | t | Sig. (bilateral) | |
| Sign-sign1 | 0.718 | 0.821 | 0.081 | 0.558 | 0.879 | 8.876 | 0 |
| Sign-sign3 | 1.524 | 0.938 | 0.092 | 1.341 | 1.708 | 16.497 | 0 |
| Sign1-sign3 | 0.806 | 0.715 | 0.07 | 0.666 | 0.946 | 11.441 | 0 |
Table 1. Changes of nasal sign scores with 3 months after the treatment.
Asthma control scores
Statistical analyses for the asthma scores were done for Group C only. Among the 31 Group C patients, 19 exhibited improved scores, while the remaining 12 patients showed little change before and after the treatment. This might be because the treatment course for asthma is usually longer than three months and under normal circumstances; it would be relatively rare to obtain a positive change after a three-month treatment only. Therefore, the follow-up for this group will be continued for 1-2 years for further analysis and reliable statistics.
Discussion
Correlations between the upper and lower airway diseases had been proposed as early as the second century, but they have only been getting attention in clinical practice in recent years. The present study was based on the factors that mutually influence the upper and lower airways. The combined therapy was designed with an aim to investigate the effects and significance of such treatment protocols. The statistical analyses showed that the treatment efficacy in patients with pure AR was significantly better than that in patients with AR associated with lower airway inflammation. This suggests that AR should be diagnosed as early as possible, or at least, that its association with lower airway inflammation be ruled out. After diagnosis, positive combined therapy should be performed to ensure more significant effects. The combined therapy of fluticasone propionate nasal spray and salmeterol fluticasone inhalant had obvious short-term effects in controlling the symptoms of AR associated with asthma. These conclusions support our desired therapeutic effects. The data obtained support our conclusion that ULA-CT could achieve better results in a shorter period of time. Continuous follow-up of patients in groups B and C is necessary for further data collection and analysis to determine whether ULA-CT could have intervention and prevention effects on lower airway inflammation.
Grossman clearly put forward the theory that "diseases in the upper and lower airways should be treated integratedly" [12]. Experts from many countries developed the guidelines on AR and its impacts on asthma (ARIA), which also became a part of the WHO’s initiatives. Many epidemiological studies have shown that asthma and rhinitis often occur in the same patient [13,14]. Most paediatric patients with AR often have asthma simultaneously or successively [15]. AR and asthma have considerable familial characteristics and risks [16-18]. Because of the structural similarity and continuity between the upper and lower airways, many BHR children also present with upper airway problems. This could easily result in the improper treatment of pure upper airway disease that presents with lower airway symptoms clinically [19]. As the prevalence of allergic diseases is increasing yearly and the age of onset is decreasing, an increasing number of children would be affected by airway diseases. Most of these children would be treated excessively. In light of this situation, treatment protocols for paediatric patients could be designed based on this study. The related data should be collected and analysed to expand the treatment applications of ULA-CT in paediatric patients [20].
The influencing mechanisms of nasal inflammation in the lower airway are mainly centered on the nasobronchial nervous reflex contact, primarily through the sphenopalatine and vagus nerves affecting the bronchi and lungs. Firstly, this reflex is executed through the afferent trigeminal nerve and the efferent vagus nerve reflex arc, that is, nasal mucosal stimulation could cause the contraction of bronchial mucosa. Secondly, because of its impact on the mode of breathing, nasal inflammation would lead to nasal congestion and thus, open-mouthed breathing. The latter has no warming, humidifying, and cleansing effects on inhaled air like the nose does; therefore, dry, cold, and dirty air could directly stimulate the airway. Thirdly, the immunological interactions and the dissemination of nasal inflammatory cells and mediators occur mainly through the backflow of nasal secretions, which are rich in inflammatory substances, into the lower respiratory tract and the absorption of inflammatory substances into the bloodstream, thus directly affecting the lungs [21,22]. In view of such physiological characteristics, the benefits of ULA-CT have some basis [23] that needs to be further investigated urgently. Studies need to be effectively designed and the relevant data collected for early diagnosis and scientific clinical intervention, as well as to stop the spread of local respiratory inflammation to the entire airway.
The relationship between AR and asthma is one of the key research areas in our department. By comparatively studying patients with AR and asthma, we obtained interrelated data on the severity of disease development, thus laying important foundations for the diagnosis and treatment of AR and asthma, and for providing data for the standard diagnosis and treatment. We found that the longer the upper airway symptoms persisted, the stronger the severity of the corresponding lower airway diseases, and the more sensitive the mucosal excitement level [23].
This study demonstrates the importance of standardized diagnosis and treatment. Clinically, misdiagnosis and improper treatment are prone to occur. Expecting asthma to exhibit more severe symptoms could lead to a misdiagnosis and a rhinitiscaused cough could be misdiagnosed as asthma. Improper treatment may include overtreatment and the abuse of hormones. The correct diagnosis and treatment of AR can result in better short-term effects, and it can effectively reduce the amount of hormonal treatment required, thus reducing the patient’s financial burden to some extent.
Acknowledgements
This study was supported by the "Eleventh Five-Year" National Technology Support Project, Ministry of Science and Technology (2007BAI18B15) and National Natural Science Foundation of China (81570896).
Conflict of Interest
All authors have no conflict of interest regarding this paper.
References
- Kony S, Zureik M, Neukirch C, Leynaert B, Vervloet D, Neukirch F. Rhinitis is associated with increased systolic blood pressure in men: a population-based study. Am J Respir Crit Care Med 2003; 167: 538-543.
- Ciprandi G, Cirillo I. The lower airway pathology of rhinitis. J Allergy Clin Immunol 2006; 118: 1105-1109.
- Oka A, Matsunaga K, Kamei T, Sakamoto Y, Hirano T, Hayata A, Akamatsu K, Kikuchi T, Hiramatsu M, Ichikawa T, Nakanishi M, Minakata Y, Yamamoto N. Ongoing allergic rhinitis impairs asthma control by enhancing the lower airway inflammation. J Allergy Clin Immunol Pract 2014; 2: 172-178.
- Yoo JY, Kim MJ, Hwang SG, Ahn KC, Ryu JC, Choi MK, Joo JH, Kim CH, Lee SN, Lee WJ, Kim J, Shin DM, Kweon MN, Bae YS, Yoon JH. Distinct TLR-mediated pathways regulate house dust mite-induced allergic disease in the upper and lower airways. J Allergy Clin Immunol 2013; 131: 549-561.
- Karra L, Haworth O, Priluck R, Levy BD, Levi-Schaffer F. Lipoxin B4 promotes the resolution of allergic inflammation in the upper and lower airways of mice. Nature 2015; 8: 852-862.
- Smolensky MH, Lemmer B, Reinberg AE. Chronobiology and chronotherapy of allergic rhinitis and bronchial asthma. Adv Drug Deliv Rev 2007; 59: 852-882.
- Shaaban R, Zureik M, Soussan D, Neukirch C, Heinrich J, Sunyer J, Wjst M, Cerveri I, Pin I, Bousquet J, Jarvis D, Burney PG, Neukirch F, Leynaert B. Rhinitis and onset of asthma: a longitudinal population-based study. Lancet 2008; 372: 1049-1057.
- Pawankar R. Allergic rhinitis and its impact on asthma: an evidence-based treatment strategy for allergic rhinitis. Asian Pac J Allergy Immunol 2002; 20: 43-52.
- Corren J. The connection between allergic rhinitis and bronchial asthma. Curr Opin Pulm Med 2007; 13: 13-18.
- Nayak AS. The asthma and allergic rhinitis link. Allergy Asthma Proc 2003; 24: 395-402.
- Bousquet J, Van Cauwenberge P, Khaltaev N. World Health Organization. Allergic rhinitis and its impact on asthma. J Allergy Clin Immunol 2001; 108: S147-334.
- Grossman RF. Guidelines for the treatment of acute exacerbations of chronic bronchitis. Chest 1997; 112: 310S-313S.
- Lughezzani G, Burger M, Margulis V, Matin SF, Novara G, Roupret M, Shariat SF, Wood CG, Zigeuner R. Prognostic factors in upper urinary tract urothelial carcinomas: A comprehensive review of the current literature. Eur Urol 2012; 62: 100-114.
- Togias A. Unique mechanistic features of allergic rhinitis. J Allergy Clin Immunol 2000; 105: S599-604.
- Nathan RA, Eccles R, Howarth PH, Steinsvag SK, Togias A. Objective monitoring of nasal patency and nasal physiology in rhinitis. J Allergy Clin Immunol 2005; 115: S442-459.
- Rochat MK, Illi S, Ege MJ, Lau S, Keil T, Wahn U, von Mutius E. Allergic rhinitis as a predictor for wheezing onset in school-aged children. J Allergy Clin Immunol 2010; 126: 1170-1175.
- Chawes BL, Kreiner-Møller E, Bisgaard H. Upper and lower airway patency are associated in young children. Chest 2010; 137: 1332-1337.
- Brinkman BM, Telliez JB, Schievella AR, Lin LL, Goldfeld AE. Engagement of tumor necrosis factor (TNF) receptor 1 leads to ATF-2- and p38 mitogen-activated protein kinase-dependent TNF-alpha gene expression. J Biol Chem 1999; 274: 30882-30886.
- Profita M, La Grutta S, Carpagnano E, Riccobono L, Di Giorgi R, Bonanno A, Pace E, Bonsignore G, Bousquet J, Vignola AM, Gjomarkaj M. Noninvasive methods for the detection of upper and lower airway inflammation in atopic children. J Allergy Clin Immunol 2006; 118: 1068-1074.
- Groot EP, Nijkamp A, Duiverman EJ, Brand PL. Allergic rhinitis is associated with poor asthma control in children with asthma. Thorax 2012; 67: 582-587.
- Joo JH, Ryu JH, Kim CH, Kim HJ, Suh MS, Kim JO, Chung SY, Lee SN, Kim HM, Bae YS, Yoon JH. Dual oxidase 2 is essential for the toll-like receptor 5-mediated inflammatory response in airway mucosa. Antioxid Redox Signal 2012; 16: 57-70.
- Shen JC, Cope E, Chen B, Leid JG, Cohen NA. Regulation of murine sinonasal cilia function by microbial secreted factors. Int Forum Allergy Rhinol 2012; 2: 104-110.
- Matsunaga K, Kawabata H, Hirano T, Sugiura H, Minakata Y, Ichinose M. Difference in time-course of improvement in asthma control measures between budesonide and budesonide/formoterol. Pulm Pharamcol Ther 2013; 26: 189-194.