ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 17
The alleviation of myocardial ischemia/reperfusion injury by lycopene
Zhenjun Liu*, Guangming He and Lili Zhao
Intensive Care Unit of the Sichuan Cancer Hospital, Chengdu, Sichuan, PR China
- *Corresponding Author:
- Zhenjun Liu
Intensive Care Unit of the Sichuan Cancer Hospital
Renming Road of Chengdu, PR China
Accepted on August 22, 2017
Myocardial Ischemia/Reperfusion (MI/R) injury is a clinical phenomenon including myocardial structural damage, dysfunction and disorders of metabolism and electrophysiology after re-perfusion of ischemic heart tissues. It mainly occurs after myocardial infarction and by-pass surgery, and is one major issue in clinic. Lycopene has been known to exert anti-oxidation effects. This study thus investigated the protective role and possible mechanism of lycopene on rat MI/R injury. 80 male SD rats were randomly and equally divided into sham, MI/R, lycopene treatment, and lycopene+EX527 group (N=20). MI/R model was established by the ligation of left descending coronary artery for 30 min followed by reperfusion for 6 h. Ultrasonic cardiogram was used to evaluate cardiac functions, while serum enzyme and myocardial apoptosis were detected by ELISA and TUNEL assays respectively. The area of infarction was determined by Evans blue-TTC double staining. Western blot was used to detect the levels of Sirt1, cIAP1, Bax and Bcl-xl. Lycopene significantly improved cardiac functions as shown by lower CK and LDH levels. It can also decrease the infarction area and reduce apoptotic cell numbers. Sir1 and Bcl-xl expressions were up-regulated while cIAP1 and Bax were down-regulated after lycopene treatment. However, EX527, an inhibitor of Sirt1, can reverse such effects of lycopene (p<0.05 in all cases). Lycopene can protect rat cardiomyocytes from MI/R injury, possibly via activation of Sirt1 signaling pathway to decrease reactive stress response after MI/R injury and subsequent amelioration of inflammatory injury.
Keywords
Lycopene, MI/R injury, Inflammation, Oxidative stress, Anti-apoptosis.
Introduction
Myocardial Ischemia/Reperfusion (MI/R) injury is the transition of myocardial cells with reversible injury due to ischemia into irreversible injury after blood reperfusion, and frequently occurs in those myocardial ischemia patients with regaining of blood flow [1]. MI/R injury is induced by multiple factors and involves complicated patho-physiological processes including oxidative stress, inflammatory response, cardiac dysfunction, myocardial necrosis and apoptosis [2,3]. Study has found the involvement of various risk factors including a large amount of oxygen free radicals, calcium ion over-load and inflammatory factors in the occurrence and development of MI/R injury, but still with unclear mechanism so far [4].
Lycopene mainly exists in fresh fruits such as tomatoes, and has potent anti-oxidation functions, thus can alleviate oxidative stress injury or inhibit hypersensitivity [5]. Another study also found reduced cancer incidence after lycopene treatment in breast cancer, prostate cancer and pancreatic carcinoma [6]. Moreover, other studies also suggested the protective effect of lycopene on post-cerebral ischemia [7]. Recently, lycopene has become the research hotspot in the prevention of endoplasmic reticulum induced cell apoptosis [8]. Some people believed that lycopene could alleviate cell apoptosis after myocardial infarction and inflammation, possibly via inhibiting NF-κB signal pathway [9].
Sir1 is a histone deacetylase that is dependent on NAD+. It is one of major transcriptional factors protecting myocardial cells from endogenous apoptosis. A previous study has indicated the critical role of Sirt1 in elongating cell life restricting by energy, as well as in cell differentiation, apoptosis and proliferation [10]. Recent study indicated the anti-MI/R injury function by activating Sirt1 was mainly via regulating its downstream molecule, cellular inhibitory for apoptotic protein 1 (cIAP1) [11-14]. However, the relationship between lycopene and MI/R injury, as well as its correlation with Sirt1 signaling pathway remains poorly understood. This study aimed to investigate the effect of lycopene on MI/R injury and functional mechanism in MI/R injury rat model.
Materials and Methods
Materials
80 adult male SD rats (body weight 230 g ± 20 g) were provided by Laboratory Animal Center, Sichuan University. Pentobarbital sodium and lycopene (Sigma, US); EX527 (Selleck Chemical, US); TUNEL assay kit, TTC test kit, CK test kit, and LDH test kit (Taiyang Biotech, China); Goat anti- Sirt1, goat anti-cIAP1, rabbit anti-Bcl-xl and rabbit anti-Bax (Boaosen Biotech, China).
Rats were used for all experiments, and all procedures were approved by the Animal Ethics Committee of Sichuan Cancer Hospital.
Animal grouping
80 adult male SD rats were randomly and equally divided into 4 groups (N=20 each): (1) Sham group; (2) MI/R group, which received equal volume of tetrahydrofuran via intraperitoneal injection before surgery; (3) Lycopene treatment group, which received intraperitoneal injection of lycopene (40 mg/(kg•d) for 5 d; and (4) MI/R+lycopene+EX527 group, which received EX527 (5 mg/(kg•d) for 3 times every other day via intraperitoneal injection along with lycopene as described in the previous group. All rats were anesthetized with 30 g/L pentobarbital sodium (50 mg/kg) via intraperitoneal injection, and intubated in trachea, which was connected to an animal respirator (tidal volume, 5~6 ml/100 g, respiratory rate, 10~80 per min). Sternum was opened between 4th and 5th rib, followed by incision of pericardium. The left atrial appendage was exposed for ligating the left descending branch of coronary artery at the upper 1/3 site using 5-0 silks followed by ligation using silicone tube. Sham group received only silk puncture but not ligation.
Blood indexes
After 6 h of MI/R model generation, 3 ml blood was collected from left ventricle. After incubation for 30 min, the blood was centrifuged for 10 min to collect the serum, in which CK-MB and LDH-1 levels were detected by commercial kit using manual instructions.
Cardiac function assay
6 h after MI/R surgery, Vevo2100 small animal ultrasound equipment was used to record the alternation of cardiac function indexes including Left Ventricular Ejection Fraction (LVEF) and Left Ventricle Fractional Shortening (LVFS).
Evans blue-TTC double staining
6 h after MI/R surgery, coronary artery of rats was ligated in situ, and were retrograde perfused with 1% Evans blue (3 ml) to completely stain myocardial cells at non-ischemia region. The heart was removed and frozen at -70°C for 30 min, followed by being sectioned for 5~6 slices below the ligation site (thickness 2 mm). Tissues slices were incubated with 20 g/L TTC in PBS (ph7.4) at 37°C for 20 min. White area represented ischemia infarction region while red and blue refer to ischemia (but not infarction) and non-ischemia regions, respectively. The risk area was defined as the sum of red and white zones. Image Pro Plus software was used to detect the areas of all regions. Myocardial infarction ratio=infarction area/ischemia area × 100%.
TUNEL assay
6 h after MI/R surgery, part of ischemia heart tissues were extracted and fixed in neutral buffered formalin. The tissue was then embedded in paraffin and sectioned. The apoptosis of myocardial cells was detected by TUNEL test kit. A total of 5 high magnification (X400) fields without over-lapping were randomly selected from MI/R regions for calculating myocardial cell apoptotic rate, which was defined as the total number of apoptotic myocardial cells divided by the total number of cardiomyocytes.
Western blotting
6 h after MI/R surgery, myocardial tissues were homogenized and lysed in lysis buffer to extract total proteins, which were quantified by BCA assay. Proteins were separated by gel electrophoresis, and transferred to PVDF membrane. The membrane was firstly blocked for 2 h at room temperature using TBST. Primary antibody (goat anti-Sir1, goat anti-cIAP1, rabbit anti-Bcl-xl and rabbit anti-Bax antibody) was then added and incubated overnight followed by TBST rinsing (3 times). Horseradish peroxidase-conjugated rabbit anti-goat IgG or goat anti-rabbit IgG secondary antibody was then added for 12 h room temperature incubation. After 3 times of TBST rinsing and ECL development, Bio-Rad imaging system was used to analyse the relative expression of target proteins using β-actin as the internal control to quantify the expression levels of Sirt1, cIAP1, Bcl-x and Bax.
Statistical analysis
SPSS19.0 software was used to process all collected data, which were presented as mean ± Standard Deviation (SD). One-way Analysis of Variance (ANOVA) with Newman-Keuls multiple comparison post-hoc analysis, was used in multiple group comparison. P<0.05 was considered as statistical significance.
Results
Rat cardiac functions after MI/R surgery
Ultrasound cardiograph analysis at 6h after surgery suggested that, compare with Sham group, both LVEF and LVFS were significantly depressed in MR/R group, suggesting successful establishment of the model. MI/R-lycopene can significantly improve LVEF and LVFS in myocardial tissues, while the application of EC527, a Sirt1 specific inhibitory, significantly decreased those indexes (Table 1).
| Index | Sham group | MI/R group | MI/R+lycopene group | EX572 group |
|---|---|---|---|---|
| EF (%) | 92.37 ± 1.85 | 79.74 ± 3.95* | 91.83 ± 0.85# | 78.54 ± 2.95* |
| FS (%) | 60.63 ± 4.12 | 41.24 ± 2.75* | 62.61 ± 2.21# | 40.455 ± 2.35* |
| Vmax (cm/s) | 142.83 ± 7.97 | 98.17 ± 1.92* | 139.72 ± 4.93# | 96.71 ± 2.92* |
| Note: Compared with Sham group, *P <0.05; Compared with MI/R group, #P<0.05. | ||||
Table 1. Cardiac functions.
Serum parameters of MI/R rats
6 h after MI/R surgery, serum samples were assayed and showed significantly elevated CK-MB and LDH-1 levels in MI/R model group compared with those in control group (p<0.05). While in MI/R+lycopene group, CK-MB and LDH-1 levels were significantly decreased (p<0.05). However, application of Sirt1 specific blocker EX527, significantly reduced CK and LDH levels (Table 2).
| Index | Sham group | MI/R group | MI/R+Lycopene group | EX527 group |
|---|---|---|---|---|
| CK | 92.37 ± 27.85 | 2755.01 ± 503.95* | 1530.24 ± 456.27# | 2897.24 ± 455.40* |
| LDH | 160.63 ± 45.12 | 1941.24 ± 225.75* | 1285.61 ± 243.21# | 2040.45 ± 279.35* |
| Note: Compared with Sham group, *P<0.05; Compared with MI/R group, #P<0.05. | ||||
Table 2. CK and LDH levels in all groups.
Myocardial infarction area and cell apoptotic rate
6 h after MI/R surgery, Evans blue-TTC double staining was employed to determine the infarction area. Compared with Sham group, MI/R rats displayed significantly larger infarction area and myocardial cell apoptotic rate, while in MI/R +lycopene group, those indexes were remarkably decreased (p<0.05). The application of Sirt1-specific inhibitor, EX527, significantly reduced those indexes (Table 3).
| Index | Sham group | MI/R group | MI/R+Lycopene group | EX572 group |
|---|---|---|---|---|
| Myocardial infarction (%) | 1.34 ± 0.94 | 72.45 ± 4.96* | 37.69 ± 3.86# | 70.51 ± 4.78* |
| Cell apoptosis (%) | 2.44 ± 0.74 | 62.94 ± 4.36* | 35.72 ± 3.54# | 68.45 ± 4.94* |
| Note: Compared with Sham group, *P<0.05; Compared with MI/R group, #P<0.05. | ||||
Table 3. Rat myocardial infarction area and cell apoptotic rates.
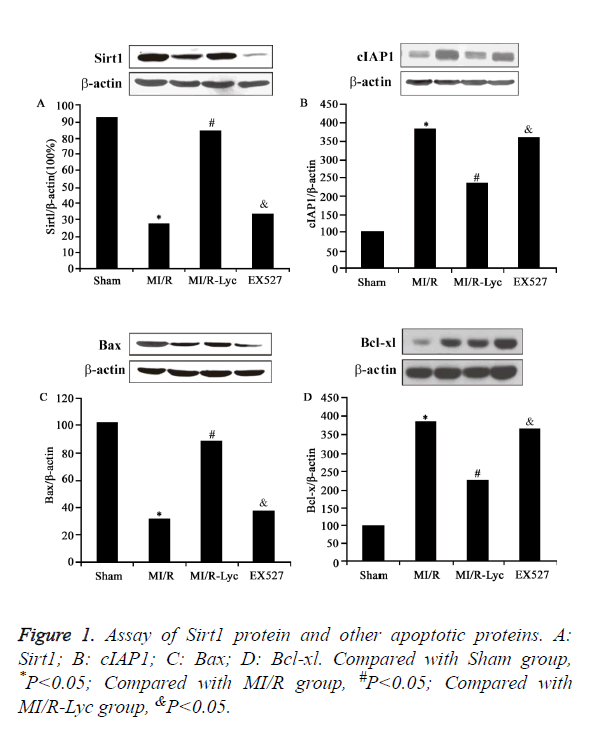
Sirt1 protein and other apoptotic proteins in MI/R rats
6 h after MI/R surgery, Western blot analysis revealed significantly decreased Sirt1 protein expression in MI/R group compared with that in Sham group (p<0.05). However, Sirt1 protein level was remarkably elevated after lycopene treatment (p<0.05). The application of Sirt1-specific inhibitor, EX527, significantly decreased Sirt1 protein expression (p<0.05, Figure 1A). Similar patterns were observed for cIAP1 expression, which was demonstrated by elevated cIAP1 level in MI/R group, decreased in MI/R+lycopene group, and depressed in EX527 group (p<0.05, Figure 1B). Another pair of studies targeting cell apoptotic proteins revealed elevated Bcl-xl expression and reduced Bax expression in MI/R +lycopene group compared with model group, with reverse of such protective effects by EX527 (Figures 1C and 1D).
Discussion
Ischemia heart disease is one of the major reasons causing death. The treatment focus is to regain normal blood supply of myocardial tissues. The secondary damage after reperfusion, however, leads to severe complications and causes unfavorable prognosis and even death [15]. Previous studies found that Lyc had pluripotent functions including anti-oxidation, clearing free radicals, modulating cell proliferation/differentiation and inducing cell-to-cell connection [16,17], as well as anti-tumor or cardiac protection [18,19]. Therefore this study mainly explored the protective function and related mechanism of lycopene on MI/R injury.
As one of the basic transcriptional factors, Sirt1 plays crucial role sin cell survival, aging and apoptosis [10,20]. It also exerts critical modulatory functions in the development of heart, cardiac failure, heart hypertrophy, coronary disease, and atherosclerosis [13,14]. Nadtochiy et al. found the participation of activated Sirt1 in ischemia-induced endogenous anti-MI/R injury [21]. Hsu et al found decreased Sirt1 expression after MI/R injury while activation of Sirt1 improved MI/R function [22]. The mechanism by how Sirt1 activation improves MI/R function might be through upregulation of the expression of anti-apoptotic molecule Bcl-xl while down-regulation of pro-apoptotic factor Bax expression, thus protecting myocardial tissues via suppressing cell apoptosis. In addition, overexpression of SIRT1 has been reported to be capable to reduce diabetes-exacerbated MI/R injury and oxidative stress via activating eNOS in diabetic rats [23]. Zhang et al. also showed elevation of Bcl-2 expression and depression of Bax after Sirt1 activation suppressed cell apoptosis [24]. Consistently, upregulation of Sirt1 expression was demonstrated to inhibit osteoarthritis chondrocyte apoptosis through upregulation of Bcl-2 and down-regulation of Bax expression [25].
Our results showed decreased Sirt1 expression in MI/R group compared with Sham group, accompanied with the increase of cIAP1 expression. Treatment of lycopene remarkably up-regulated Sirt1 expression and decreased cIAP1 level, suggesting an anti-apoptotic role of lycopene in the protection from MI/R injury. However, exogenous replenishment of Sirt1 specific inhibitor, EX527, significantly down-regulated Sirt1 expression, and inhibited the protective effect of lycopene against MI/R injury, further supporting the role of Sirt1 in lycopene-induced protection of MI/R injury.
Lycopene is a natural compound extracted from plants with lower cost and toxicity, and is suitable for long-term intake among different populations. This study showed the protective effect of lycopene on MI/R injury of rats, as shown by lowered apoptotic rate of myocardial tissues and infarction area, higher cell survival rates, which might facilitate the recovery of cardiac functions. This study provided new insights for preventing MI/R reperfusion injury, and novel target for cardiac protective drugs development.
Conclusion
Lycopene can protect rat cardiomyocytes from MI/R injury, possibly via activation of Sirt1 signaling pathway and subsequent decrease of reactive stress response after MI/R injury, leading to amelioration of inflammatory injury.
References
- Li CM. Myocardial ischemic post-conditioning attenuates ischemia reperfusion injury via PTEN/Akt signal pathway. Int J Clin Exp Med 2015; 8: 15801-15807.
- Wang G. Sildenafil protects against myocardial ischemia-reperfusion injury following cardiac arrest in a porcine model: possible role of the renin-angiotensin system. Int J Mol Sci 2015; 16: 27015-27031.
- Zhang J. Vagal modulation of high mobility group box-1 protein mediates electroacupuncture-induced cardioprotection in ischemia-reperfusion injury. Sci Rep 2015; 5: 15503.
- He Q. Lycopene attenuates inflammation and apoptosis in post-myocardial infarction remodeling by inhibiting the nuclear factor-kappaB signaling pathway. Mol Med Rep 2015; 11: 374-378.
- Riccioni G. Protective effect of lycopene in cardiovascular disease. Eur Rev Med Pharmacol Sci 2008; 12: 183-190.
- Jacques PF. Relationship of lycopene intake and consumption of tomato products to incident CVD. Br J Nutr 2013; 110: 545-551.
- Vilahur G. Intake of cooked tomato sauce preserves coronary endothelial function and improves apolipoprotein A-I and apolipoprotein J protein profile in high-density lipoproteins. Transl Res 2015; 166: 44-56.
- Furui Y. Cytomegalovirus (CMV) seroprevalence in Japanese blood donors and high detection frequency of CMV DNA in elderly donors. Transfusion 2013; 53: 2190-2197.
- Xu J. Lycopene protects against hypoxia/reoxygenation injury by alleviating ER stress induced apoptosis in neonatal mouse cardiomyocytes. PLoS One 2015; 10: e0136443.
- Ding M. SIRT1 protects against myocardial ischemia-reperfusion injury via activating eNOS in diabetic rats. Cardiovasc Diabetol 2015; 14: 143.
- Shalwala M. Sirtuin 1 (SIRT1) activation mediates sildenafil induced delayed cardioprotection against ischemia-reperfusion injury in mice. PLoS One 2014; 9: e86977.
- Gu C. Impaired cardiac SIRT1 activity by carbonyl stress contributes to aging-related ischemic intolerance. PLoS One 2013; 8: e74050.
- Yu L. Reduced silent information regulator 1 signaling exacerbates myocardial ischemia-reperfusion injury in type 2 diabetic rats and the protective effect of melatonin. J Pineal Res 2015; 59: 376-390.
- Yang Y. SIRT1 activation by curcumin pretreatment attenuates mitochondrial oxidative damage induced by myocardial ischemia reperfusion injury. Free Radic Biol Med 2013; 65: 667-679.
- Yan J. Total saponins from Aralia taibaiensis protect against myocardial ischemia/reperfusion injury through AMPK pathway. Int J Mol Med 2015; 36: 1538-1546.
- Kim JY. Pretreatment with lycopene attenuates oxidative stress-induced apoptosis in human mesenchymal stem cells. Biomol Ther (Seoul) 2015; 23: 517-524.
- Bhatia N. Lycopene enriched tomato extract inhibits hypoxia, angiogenesis, and metastatic markers in early stage N-nitrosodiethylamine induced hepatocellular carcinoma. Nutr Cancer 2015; 67: 1268-1275.
- Wang Y. Effect of carotene and lycopene on the risk of prostate cancer: a systematic review and dose-response meta-analysis of observational studies. PLoS One 2015; 10: e0137427.
- Chen P. Lycopene and risk of prostate cancer: a systematic review and meta-analysis. Medicine (Baltimore) 2015; 94: e1260.
- Satoh A. The brain, sirtuins, and ageing. Nat Rev Neurosci, 2017. 18(6): p.362-74.
- Nadtochiy, S.M. Lysine deacetylation in ischaemic preconditioning: the role of SIRT1. Cardiovasc Res 2011; 89: 643-649.
- Hsu CP. Silent information regulator 1 protects the heart from ischemia/reperfusion. Circulation, 2010; 122: 2170-2182.
- Ding M. SIRT1 protects against myocardial ischemia-reperfusion injury via activating eNOS in diabetic rats. Cardiovasc Diabetol 2015; 14: 143.
- Zhang C. Resveratrol attenuates doxorubicin-induced cardiomyocyte apoptosis in mice through SIRT1-mediated deacetylation of p53. Cardiovasc Res 2011; 90: 538-545.
- He DS. Underlying mechanism of Sirt1 on apoptosis and extracellular matrix degradation of osteoarthritis chondrocytes. Mol Med Rep 2017; 16: 845-850.