ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
- Biomedical Research (2009) Volume 20, Issue 1
Retroperitoneal sarcomas - A retrospective study
Department of Surgery, College of Medicine, King Khalid University, Abha, Saudi Arabia
- *Corresponding Author:
- Mohammed Al-Qahtani
College of Medicine
King Khalid University
PO.Box 641, Abha
Saudi Arabia
E-mail: msali11@hotmail.com
Accepted date: 25 September 2008
Outcomes of the management of retroperitoneal sarcoma in the Northern Alberta (NA), Canada was examined in this study. 75 patients (34 females and 41 males, age range 30-87 years) underwent operations at the CCI for PRS (sarcomas represented 61% of all the cases). A retrospective analysis of these patients was performed to determine the prognostic parameters associated with a favorable prognosis. Complete resection was possible in 33% of cases (n = 25), incomplete resection was performed in 35% (n = 26) and in 32% (n = 24) only biopsy was possible. Frequently resected adjacent organs were: kidney (15%), colon (10%) and pancreas (6%). Univariate analysis demonstrated that complete resection was an independent factor for survival as compared to partial resection or biopsy alone (p=0.001). Patients with complete resection had a 12 month survival of 100% (n = 25) compared to 84% (n = 22) for those undergoing partial resection and 25% (n = 5) for those with simple biopsy. A 24-month survival of the patients undergoing complete resection was 88% (n = 22). Median survival for type of surgical treatment was 91.2 (88.2-104.9) months for complete resection compared to 30.4 (24.2-41.5) months for partial resection and only 5.7 (2.6-8.1) months for biopsy. Complete resection is the cornerstone of the treatment and is important for long-term survival in patients with retroperitoneal soft tissue sarcomas.
Keywords
Retroperitoneal; Soft tissue sarcoma, Univariate analysis
Introduction
The incidence of Primary Retroperitoneal Sarcomas (PRS) that form a heterogeneous group of malignant neoplasm is very low and comprise only 1% of all malignant tumors and approximately 10 per cent of all sarcomas [1-3]. The histogenesis of retroperitoneal tum-our and its treatment underwent evolution since first described in 1829 by Lobstein. Initially it was linked to adult urogenital apparatus, later it was found that liposar-comas are the most common type of retroperitoneal sarcomas (61%); with majority of them being low grade tumors [4]. Leiomyosarcomas were the next most com-mon pathology (30%); with most of them being high grade. Low-grade sarcomas overall accounted for 62 per cent of the total group.
The surgical resection of tumour was advocated as the best options of treatment almost a century ago and effort was made to optimize the surgical treatment [5-18]. However, curative surgery is limited by several factors. First, retroperitoneal sarcomas present as large tumors probably because of late diagnosis. This is due to the minimal symptoms they produce and their "hidden" position in the body. Secondly, surgical resection is hindered by the close proximity with the vital structures of the retroperitoneum. Thirdly, these tumors often involve adjacent organs, necessitating concomitant resec-tion of these organs. Finally, clear surgical margins are often difficult to obtain despite radical surgery. These treatment-related problems may contribute to the poor outcome of surgery. Despite the enourmous effort to optimize the surgery, 5-year survival after surgery improved from 2% in 1954 to 39% in 2000, however local recurrence was often requiring multiple resections. It was shown that aggressive surgery with resection of adjacent structure is the single most important factor that improves survival [8,19,20]. Other factors found to be predictive of survival were stage at presentation and histological grade. Chiappa et al demonstrated that patie-nts with low grade sarcoma had 5-years survival of 90% compared with 26% only in patients with high grade sarcoma. Stage II A had 82% 5-years survival as compa-red to 22% in advanced stage [15].
To better understand the complex nature of this group of malignancies we undertook this study to review the biologic and clinical behavior of retroperitoneal sarco-mas. Special attention was directed to identifying any tumor- or treatment-related characteristics that had imp-act on clinical outcome including the treatment of local recurrence.
Patients and Methods
The clinical courses of all adult patients treated from 1989 to 2003 for soft-tissue sarcomas of the retroperito-neum at Cross Cancer Institute (CCI) Hospital, Northern, Alberta, Canada were retrospectively reviewed. All patie-nts underwent surgical resection. A retrospective analysis of these patients was performed to determine the progno-stic parameters associated with a favorable prognosis. The tumors were characterized by tumor size, histopatho-logic grade, lymph nodes involvement and presence of metastases. Surgery was considered complete if all gross tumors were removed and margins were negative for tumor.
Histopathologic grade was determined by the degree of hypercellularity, differentiation, pleomorphism, necrosis, and mitotic activity and categorized into low, interme-diate, or high grade. Tumor dimensions and weight were also determined. Patient- and treatment-related variables included age, sex, completeness of resection, and margin of resection (both gross and microscopic). Incomplete resection was defined as a resection where gross residual disease was obvious after resection. The patients were traced to their last clinical follow-up or death. Survival was calculated in months from the primary surgical treatment to last follow-up or death. Survival data were analyzed by the method of Kaplan and Meier as well as by the log-rank test for statistical significance.
Results
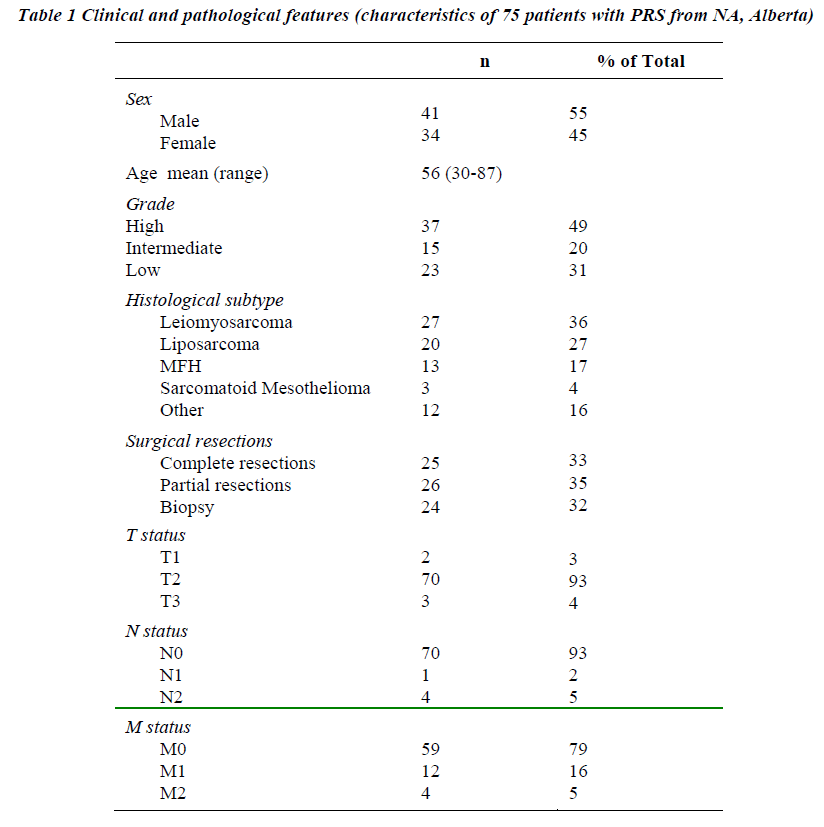
75 patients were included in the study. There were 34 females and 41 males. The mean age was 56, age range 30-87 years. All patients underwent operations and were followed until death or last follow-up date. Initial presen-ting symptoms were: severe abdominal pain (48%), palpable mass (25%), or weight loss (20%). Ninety six percent of pts had T1-2 (3%) and 93% had N0 at the time of presentation (Table 1).
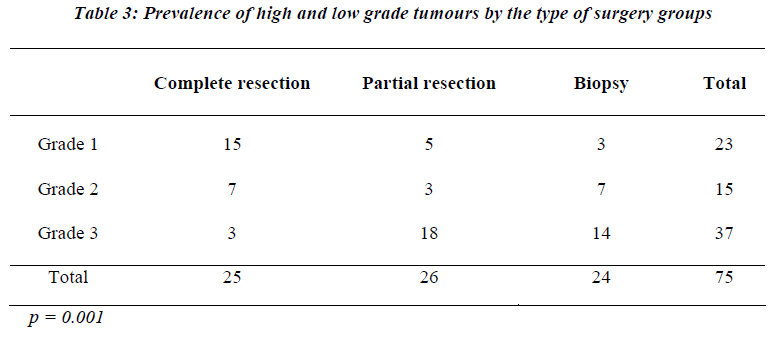
The most common histological type of retroperitoneal tumor encountered was leiomyosarcoma in 27 patients (34%). Liposarcoma was the second most common sarcoma and was encountered for 26% of tumors (20 patients). The majority of the sarcomas were high-grade tumors, which were seen in 37 out of 75 patients. In 15 cases (20%) sarcoma was intermediate grade (Table 3). The remainder 23 cases of sarcoma was of low grade (31%). Lastly there were 13 cases of malignant fibrous histiocytoma and 3 cases sarcomatoid mesothelioma.
Complete resection was possible in 33% of cases (n = 25), incomplete resection was performed in 35% (n = 26) and in 32% (n= 24) only biopsy was possible. Concomitant resection of adjacent organs was necessary to obtain clear margins in 31% of patients. Frequently resected adjacent organs were: kidney (15%), colon (10%) and pancreas (6%)
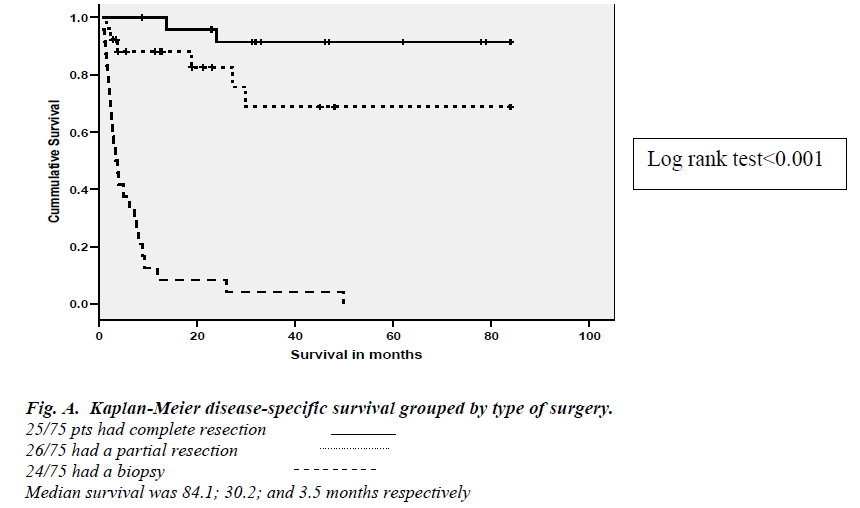
The clinical course of the 51 patients who underwent tumor resection was evaluated. All patients were availa-ble for long-term follow-up after initial surgical resec-tion. Overall survival was found to be 38 (24.2-57.1) months. Univariate analysis demonstrated that complete resection was an independent factor for survival as comp-ared to partial resection or biopsy alone (Log rank test < 0.001).
After complete resection with negative resection margins patients had a 12 months survival of 100% (n= 25) compared to 84% (n= 22) for those undergoing partial resection and 25% (n= 5) for those with simple biopsy. A 24-months survival of the patients undergoing complete resection was 88% (n= 22).
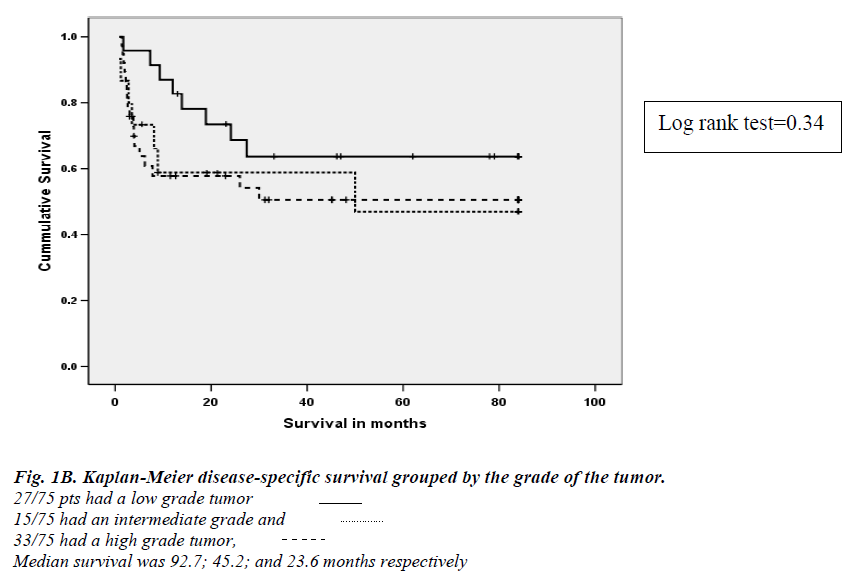
Median survival for the type of surgical treatment was 91.2 (88.2-104.9) months for complete resection compa-red to 30.4 (24.2-41.5) months for partial resection and only 5.7 (2.6-8.1) months for biopsy (Figure 1-A). Survival was not statistically different for different grade of the tumor (Figure 1-B)
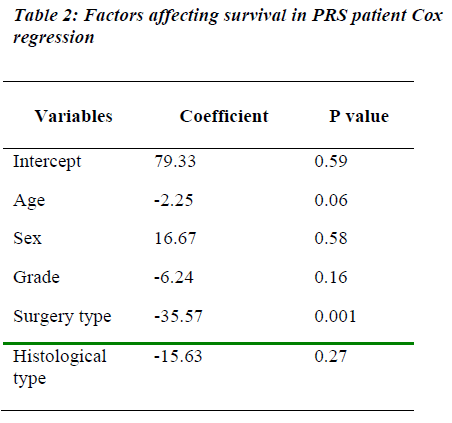
Unadjusted Cox regression model for survival with type of surgery as a single predictive variable have demonstra-ted that it predicts survival, HR= 2.6 (p<0.01). After adjusting for all known predictors of survival, the resection type was still the only significant predictor of survival (Table 2). The histological grades of the tumor had no significant impact on survival.
Discussion
Patients characteristics in our series were similar to those reported in other series; slightly male predominance with mean age of 56. Initial presentation of retroperitoneal sar-coma was also similar to one reported in the other series with most common sites of the secondary involvement being the structures such as kidney, colon and pancreas [17]. Although, the surgical resection of tumour was ad-vocated as the best options of treatment [9,15,19,21,22] our review showed that only 33% of the patients who underwent surgery for retroperitoneal sarcoma were com-pletely resected. The rate of complete resection inour study was lower as experienced in other series. In the se-ries of University of Florida, Makella et al reported 75% resectability rate of primary tumors [19]. Seventy-six per-cent of patients with PRS were completely resected in series of Samsung Medical Center, Korea [21]. Low per-centage of resection in our study may be attributed to the delay in surgery because our hospital is a referral hospital. The overall survival of 38 months in our series was simi-lar to that reported by the series of Royal Liverpool Uni-versity Hospital, UK, [1] but it was lower than survival reported by Memorial Sloan-Kettering Cancer Center, New York City7. The survival rates 1 and 2 years in our study was 100% and 88% after complete resection was rewarding. Patients in our series with partial resection were found to have a less favorable prognosis (median survival 30 months). Survival was even worse for those who did have exploratory surgery. These findings were similar to recent literature reports [11,15,17,23].
Although a positive prognostic power of low grade type tumor has been reported for survival of patients with retroperitoneal sarcoma by Van Dalen et al and Skubitz et al., [10,24] which was not confirmed in our study. Data from our observational analyses and from the literature indicate that complete resection of tumor improves sur-vival. Owing to the restricted numbers of patients the modeling of the prognostic factors could not be done at this point of the analysis.
Conclusion
This analysis showed that leiomyosarcoma were more frequent in Northern, Alberta, Canada. Complete resec-tion was the cornerstone of the treatment and was impor-tant for long-term survival in patients with retroperitoneal soft tissue sarcomas. Our resection rates were lower as compared to reported clinical series. This might partly be explained by difficulty in accessing data collection in a retrospective analysis; delay in surgery, but may reflect inadequate subspecialisation in Northern, Alberta, Canada centres.
References
- Pirayesh A, Chee Y, Helliwell TR, Hershman MJ, Leinster SJ, Fordham MV, et al: The management of retroperitoneal soft tissue sarcoma: a single institution experience with a review of the literature. Eur J Surg Oncol 2001; 27:491-297.
- Martin RG, JJ B, Albores-SaavedraJ: Soft tisue tumors, Annual clinical conference. Chicago, Year book medical publisher, 1965.
- Russell WO, Cohen J, Enzinger F: A clinical and pathological staging system for soft tisue sarcomas. Cancer 1977; 1562-1570.
- Binh MB, Guillou L, Hostein I, Chateau MC, Collin F, Aurias A, et al: Dedifferentiated Liposarcomas With Divergent Myosarcomatous Differentiation Developed in the Internal Trunk: A Study of 27 Cases and Comparison to Conventional Dedifferentiated Liposarcomas and Leiomyosarcomas. Am J Surg Pathol. 2007; 31:1557-1566.
- Lewis JJ, Benedetti F: Adjuvant therapy for soft tissue sarcomas. Surg Oncol Clin North Am 1997; 6:847-862.
- Gronchi A, Casali PG, Fiore M, Mariani L, Lo Vullo S, Bertulli R, et al: Retroperitoneal soft tissue sarcomas:patterns of recurrence in 167 patients treated at a single institution. Cancer 2004; 100:2448-2455.
- Lewis JJ, Leung D, Woodruff JM, Brennan MF: Retroperitoneal soft-tissue sarcoma: analysis of 500 patients treated and followed at a single institution. Ann Surg 1998; 228:355-365.
- Mischianu D, Bana M, Dinu M, Vlasin G: [Primary retroperitoneal tumors -- the experience in the Urological Clinic of the Central Military Hospital]. Chirurgia (Bucur) 2002; 97:139-150.
- Schwarzbach MH, Hormann Y, Hinz U, Leowardi C, Bockler D, Merhtercheimer G, et al: Clinical results of surgery for retroperitoneal sarcoma with major blood vessel involvement. J Vasc Surg 2006; 44:46-55.
- van Dalen T, Plooij JM, van Coevorden F, van Geel AN, Hoekstra HJ, Albus-Lutter Ch, et al: Long-term prognosis of primary retroperitoneal soft tissue sarcoma. Eur J Surg Oncol 2007; 33:234-238.
- Windham TC, Pisters PW: Retroperitoneal sarcomas. Cancer Control 2005; 12:36-43.
- Blanken R, Meijer S, Cuesta MA, Blomjous CE: Retroperitoneal sarcomas: pre-operative assessment and surgical therapy. Neth J Surg 1991; 43:245-248.
- Budzinski G, Kusmierski S, Oczkowicz G, Krol R: [Primary retroperitoneal tumors--course, diagnosis and treatment results]. Wiad Lek 50 Suppl 1 Pt 1997;1:155-158.
- Chiappa A, Zbar AP, Bertani E, Biffi R, Luca F, Crotti C, et al: Primary and recurrent retroperitoneal soft tissue sarcoma: prognostic factors affecting survival. J Surg Oncol 2006; 93:456-463.
- Chiappa A, Zbar AP, Biffi R, Bertani E, Biella F, Viale G, et al: Effect of resection and outcome in patients with retroperitoneal sarcoma. ANZ J Surg 2006; 76:462-466,.
- Eroglu A, Kocaoglu H, Demirci S, Akgul H: Retroperitoneal soft tissue sarcoma: effect of hyperthermic total abdominal perfusion. Tumori 1999; 85:259-264.
- Kilkenny JW, 3rd, Bland KI, Copeland EM, 3rd: Retroperitoneal sarcoma: the University of Florida experience. J Am Coll Surg 1996; 182:329-339.
- Lev-Chelouche D, Abu-Abeid S, Gutman M, Kluger Y, Michovitch M, Meller I, et al: [Retroperitoneal sarcoma. Treatment of 51 patients]. Harefuah 1999; 136:589-93, 660.
- Makela J, Kiviniemi H, Laitinen S: Prognostic factors predicting survival in the treatment of retroperitoneal sarcoma. Eur J Surg Oncol 2000; 26:552-555.
- Malerba M, Doglietto GB, Pacelli F, Carriero C, Caprino P, Piccioni E, et al: Primary retroperitoneal soft tissue sarcomas: results of aggressive surgical treatment. World J Surg 1999; 23:670-675.
- An JY, Heo JS, Noh JH, Sohn TS, Nam SJ, Choi SH, et al: Primary malignant retroperitoneal tumors: analysis of a single institutional experience. Eur J Surg Oncol 2007; 33:376-382.
- Jon B. Reitan OKIOBEMSAESKT: Prognostic factors in liposarcoma. Cancer 1985; 55:2482-2490.
- Bautista N, Su W, O'Connell TX: Retroperitoneal soft- tissue sarcomas: prognosis and treatment of primary and recurrent disease. Am Surg 2000; 66:832-836.
- Skubitz KM, D’Adamodr: Sarcoma. Mayo Clin Proc 2007; 82:1409-1432.