ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 19
Neutrophil/lymphocyte ratio is a valuable data to reduce negative laporotomy rates in emergency department
Eylem Kuday Kaykisiz1*, Pinar Yeşim Akyol2, Zeynep Karakaya2, Umut Payza2 and Fatih Esad Topal2
1Department of Emergency Medicine, Bitlis State Hospital, Bitlis, Turkey
2Department of Emergency Medicine, Izmir Katip Çelebi University, Ataturk Research and Training Hospital, Turkey
- *Corresponding Author:
- Eylem Kuday Kaykisiz
Department of Emergency Medicine
Bitlis State Hospital
Bitlis
Turkey
Accepted date: September 26, 2017
Introduction: Acute appendicitis (AA) may interfere many diseases and appendectomy is the most performed intra-abdominal operation in the world. Despite of the use of advanced technology diagnostic methods, it is not shown a decrease in perforation and negative appendectomy (NA) rates. The aim of this study is to identify the effect of neutrophil/lymphocyte ratio (NLR) in reducing the NA.
Methods: 341 patients who have operated with initial diagnosis of AA in a tertiary care hospital between 01.01-31.12.2014 were included in this study. The patients who had taking antibiotics before admission, trauma or cancer history, pregnancy and under age of 17 were excluded. Histopathologic reports of 318 patients who met criteria’s were evaluated and the patients divided into 3 groups in terms of histopathologic reports as non-AA (group 1), AA (group 2) and complicated appendicitis (group3). NLR values were compared between groups.
Results: 318 patients included in this study; 196 of these were male and 122 of these were female. The mean age of males were 33.29 ± 13 and of females 32.8 ± 13.25. There were no statistically significant differences between groups in terms of age. 15.7% (n=50) of the patients were in non-AA group however 79.2% (n=252) of the patients had the diagnosis of AA and 5% (n=16) of the patients had the diagnosis of complicated appendicitis. Cut-off value of NLR determined 4.659; sensitivity of 69% and specificity of 70% in predicting AA and NLR was statistically significant to differentiate non-AA from AA but there was no statistically significance to differentiate AA from complicated appendicitis.
Conclusion: AA is one of the most frequent emergency surgical problems of the patients with abdominal pain. Timely and accurate diagnosis is essential, on the other hand high NA rates are continuing an important problem so simple, fast and reliable tests are necessary to definitive diagnosis. As a result of our study, we found out that preoperative NLR is a valuable data for this purpose. We hope that our study may contribute to developing new protocols for definitive diagnosis in emergency department.
Keywords
Acute appendicitis, Neutrophil/lymphocyte ratio, Negative appendectomy
Introduction
Acute appendicitis (AA) is one of the most common causes of acute abdomen [1,2]. The lifetime occurrence of this disease is 7% [3] with perforation rates of 17-20% [4]. Mortality risk is less than 1% in the general population but this number can rise to 50% among the elderly population [5]. This entity has some well-known signs and symptoms like increased leukocyte count and right lower quadrant pain. However, these predictors are not constant and their accuracy is questionable. Many authors have reported that a raised leukocyte count is a sensitive test for AA but is not diagnostic because of its low sensitivity [6].
Further, atypical presentations are not infrequent, especially in the elderly. To overcome morbidity and mortality of perforation before surgery, a negative appendectomy is somewhat acceptable traditionally so the negative appendectomy rates can rise to 25-30% especially in children, pregnant and elderly [7].
However, in recent years, many have considered this unacceptable, and have studied means of improving the preoperative diagnosis since the operation itself is a cause of morbidity and mortality [8]. In recent years, some authors reported that the neutrophil/lymphocyte ratio (NLR) is a predictor of inflammation and useful in the preoperative diagnosis of AA [9-11].
At the present time, there is no diagnostic tool providing an accurate diagnosis in AA preoperatively. So that studies are continuing to find a diagnostic tool that is independent from practitioners, non-invasive, inexpensive and can be used in daily practice.
The current study was planned to examine whether calculation of NLR levels can be used preoperatively as an inflammatory marker in non-appendicitis, uncomplicated appendicitis and complicated appendicitis cases. We also suggest that this parameter may prevent negative appendectomies based on its predictive value.
Materials and Methods
This cross sectional study was conducted at Ataturk Research and Training Hospital Emergency Department (ED), Izmir, Turkey. This governmental tertiary care hospital has a capacity of 1100 beds and daily number of application to ED is about 700 patients. In this study, the patients having gone appendectomy included between January 2014 and December 2014 for a year. After approval from the ethics committee of Katip Çelebi University Faculty of Medicine, Turkey, data pertaining to patients aged at least 17 years who had presented to the ED with abdominal pain and had undergone appendectomy was studied. We retrospectively reviewed a database of 341 patients who had undergone open appendectomy for a preoperative diagnosis of AA. Exclusion criteria’s were under age of 17, pregnancy, trauma history, taking antibiotics before hospital admission, cancer history and no histopathology and laboratory results in medical record 23 of 341 patients were excluded.
The clinical diagnosis of AA was established preoperatively by means of clinical history, physical examination, traditional laboratory tests and in some patients by imaging studies like ultrasonography. Laboratory tests were performed on blood samples obtained on admission to the hospital. Based on the pathology results, data was divided into 3 groups: non-appendicitis (G1) (normal appendix, and reactive lymph node hyperplasia); uncomplicated AA (G2) (uncomplicated; AA without peritonitis or phlegmonous appendicitis) and complicated appendicitis (G3) (perforated, plastrone, necrotising appendicitis and appendicitis with peritonitis cases). Preoperative neutrophil levels were recorded. CBC analysis had been performed with calibrated Mindray BC6800 device. The reference intervals neutrophil and lymphocyte counts were set by the local hospital's laboratory (neutrophil: 2 7 K/Ul; lymphocyte: 0.8-4 K/Ul). Sensitivity, specificity, negative predictive value (NPV), positive predictive value (PPV) and cut-off value of neutrophil/ lymphocyte ratio levels were calculated. The likelihood ratios were calculated as positive (LR+) and negative (LR-).
The data analysis was performed using the Statistical Package for the Social Sciences for Windows, version 22.0 (SPSS Inc, Chicago, IL, USA). The differences between groups were compared by using Mann-Whitney U-test and Kruskall Wallis H test where appropriate. Data were shown as mean ± standard deviation or median (min-max), where applicable. The cut-off values of parameters for discrimination of the groups were determined using the receiver operating characteristic (ROC) analysis. At each value, the sensitivity and specificity for each outcome under study were plotted, thus generating an ROC curve. A p value less than 0.05 was considered statistically significant.
Results
The data of 341 patients were analysed. 61.6% (196) of analysed group were male. The mean ages of males were 33.29 ± 13 and ranges from 18 to 71. The mean ages of females 32.8 ± 13.25 and ranges from 17 to 74. There was no significant difference in mean age terms of gender (p>0.05).
There were 50 patients (15.7%) in G1, 252 patients (79.2%) in G2 and 16 patients (5%) in G3. There was no significant difference in mean age between G1, G2 and G3 (p>0.05).
The mean neutrophil value was 11.08 ± 4.2; the minimum value was 2.68 and the maximum value was 22.28. The mean of lymphocyte value was 1.98 ± 0.93; the minimum value was 0.15 and the maximum value was 6.19. The mean NLR value was 7.4 ± 5.87; the minimum value was 0.54 and the maximum value was 55.7. The mean NLR value were significantly higher in G2 and G3 (p<0.05).
The mean NLR value in G1 were statistically lower than in G2 and G3 (p<0.05) however there was no statistically significant differences between the mean NLR values of G2 and G3 (p>0.05).
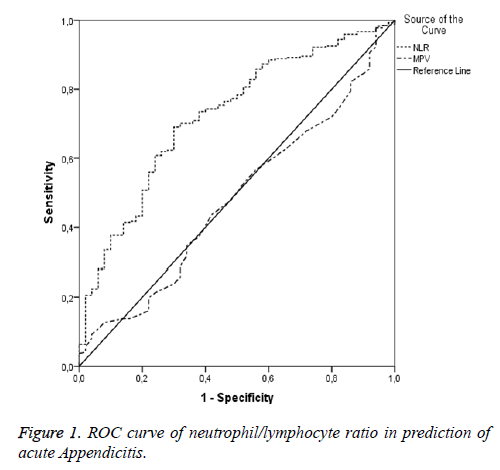
The AUC value of NLR calculated for the power in diagnosis of AA was statistically significant (AUC: 0.723 p<0.001) however the AUC value of NLR calculated for the power in diagnosis of complicated appendicitis was not statistically significant (p>0.05). The AUC value of NLR calculated for the power in diagnosis of AA was 0.723 (95% CI: 0.649-0.797), giving a sensitivity of 69.03% and specificity of 70%. Negative predictive value (NPV) was 29.7% and positive predictive value (PPV) was 92.5% (Figure 1).
Characteristics of patients are given in Table 1 and the mean NLR values of the patients in terms of the histopathologic diagnosis are given in Table 2.
| n | % | ||
|---|---|---|---|
| Gender | Male | 196 | 61.6 |
| Female | 122 | 38.4 | |
| Histopathologic diagnosis | Normal | 50 | 15.7 |
| Acute appendicitis | 252 | 9.2 | |
| Complicated appendicitis | 16 | 5 | |
Table 1: Characteristics of patients.
| NLR | P | ||
|---|---|---|---|
| Histopathologic diagnosis | Average ± SD | Min-Max | |
| Normal | 4.42 ± 3.2 | 1.14-17.73 | 0.001 |
| Acute appendicitis | 8.05 ± 6.21 | 0.54-55.7 | |
| Normal | 4.42 ± 3.2 | 1.14-17.73 | 0.024 |
| Complicated appendicitis | 6.37 ± 3.39 | 1.99-13.94 | |
| Acute appendicitis | 8.05 ± 6.21 | 0.54-55.7 | 0.431 |
| Complicated appendicitis | 6.37 ± 3.39 | 1.99-13.94 | |
Table 2: The mean NLR values of the patients in terms of the histopathologic diagnosis.
Discussion
AA is one of the most frequent emergency surgical problems of the patients with abdominal pain and still is the most operated group by surgeons. The incidence of AA ranges from 6.7% to 20% throughout the life. İt is determined that AA was seen in young adults (most likely 2. and 3. decades) and in males in many studies from literature [12-14]. In a prospective study performed by Anielski et al., the mean age was determined 36 ± 17 in patients interned with initial diagnosis of AA [15]. In our study, the mean ages of males were 33.59 ± 13 and females were 32.8 ± 13.25 and these results were compatible with literature. There were no statistically significant differences between genders in terms of age.
Grönroos et al. stated that the mean age of patients were 32.32 and 41 in patients with non-AA, AA and complicated appendicitis, respectively [16]. In our study, the mean ages of patients were 31.12 ± 12.19, 33.36 ± 12.91 and 38.88 ± 17.17 in patients with non-AA, AA and complicated appendicitis, respectively. Results of our study showed that the mean age of the patients with complicated appendicitis were higher than the patients with non-AA and AA but this superiority was not statistically significant and it is compatible with the results of Grönroos et al. (p>0.05).
AA is traditionally a clinical diagnosis however many patients may be operated unnecessary. Early diagnosis of AA may prevent perforation, abscess formation and complications of operation and reduce the treatment cost shortening the time of hospital stay. Despite of developing diagnostic technics, the diagnosis of AA is still difficult especially in children, young females, pregnant and elderly [17-19] and because of that negative appendectomy rates is still 20-30% [20-22]. In a study performed by Yıldırım et al., the negative appendectomy rate was found 11.4% [9]. Similarly in two different retrospective studies performed by Flum et al. negative laparotomy rates were found 15.5% and 23.2% and perforation rate was determine as 25.8% [15,20]. In our study we found that the negative appendectomy rates were 15.7% and the perforation rates were 5%. Negative appendectomy rates were compatible with literature although the perforation rates were lower than the other study results. We consider that this low rate caused to central location of our hospital so that the patients reached a surgeon in a short time whereat the lag of diagnosis had not been performed. Inadequate patients’ number may be another reason.
At the present time, there is no a diagnostic method for the diagnosis of AA preoperatively so that researchers bias to investigate radiological imaging techniques, inflammatory tests, scoring methods and invasive attempts like laparoscopy. NLR studied in our study seem to be practical because of it is non-invasive, easy applicable and obtained from blood samples. Many studies performed to rapid and accurate diagnosis of AA. It is sought that other parameters than total number of leukocytes because of not seem to be reliable sufficiently. Recently, it is emphasised that NLR is a better identifier than alone CRP, leukocyte and neutrophil [9,10]. NLR was studied firstly in 1995 by Goodman et al. to diagnosis of AA. NLR value determined above 3.5 in 324 patients diagnosed AA and this number was statistically significant also it is concluded that NLR was more sensitive that total leukocyte count [9]. Similar studies evaluated NLR are available and similar results have been found [11,23-26].
In our study, cut off value of 4.659 of NLR seems to be a reliable parameter to diagnose exactly on the other hand normal NLR values do not rule out the diagnosis of AA. Our cut off NLR value can differentiate normal appendix and inflamed appendix statistically significantly however this value is higher than some values determined in previous studies [9,11] on contrary lower than the cut off value determined by Ishizuka et al. [26]. There are many studies on this issue and determined different cut off values but all of them showed that NLR had diagnostic advantage than traditionally laboratory tests like alone WBC or alone CRP whereat it is reported that NLR value is an independent indicator to diagnose AA [10].
As a result, NLR seems to be a better parameter than total leukocyte count. NLR cut off value of 4.659 may be used as a diagnostic parameter for AA in this wise negative appendectomy rates can be reduced. Because of all these reasons we suggest that use of NLR as a reliable diagnostic test for diagnosis of AA in adults.
Conclusions
AA is one of the most frequent emergency surgical problems of the patients with abdominal pain. Timely and accurate diagnosis is essential, on the other hand high negative appendectomy rates are continuing an important problem so simple, fast and reliable tests are necessary to definitive diagnosis. As a result of our study, we found out that preoperative NLR with a cut-off value 4.659 is a valuable data for this purpose. We hope that our study may contribute to developing new protocols for definitive diagnosis in ED.
Funding/Support
This study was not needed to be supported financially.
Author’s Contribution
Eylem Kuday Kaykisiz: Study concept and designing, acquisition of data, critical revision of the manuscript for important intellectual content, statistical analysis; Pınar Yeşim Akyol: acquisition of data, critical revision of the manuscript for important intellectual content, technical and material support; Zeynep Karakaya: analysis and interpretation of data Umut Payza: analysis and interpretation of data: Fatih Esad Topal: study concept and designing, study supervision.
References
- Flum DR, Koepsell T. The clinical and economic correlates of misdiagnosed appendicitis: nationwide analysis. Arch Surg 2002; 137: 799-804.
- Bachman LM, Bischof DB, Bischofberger SA, Bonani MG, Osann FM, Steurer J. Systematic quantitative overviews of the literature to determine the value of diagnostic tests for predicting acute appendicitis: study protocol. BMC Surg 2002; 21: 2.
- Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol 1990; 132: 910-925.
- Basaklar C. Çocuklarda travma ve akut Karin I. Baski, Ankara: Palme Yayincilik 1994; 217-225.
- Franz MG, Norman J, Fabri PJ. Increased morbidity of appendicitis with advancing age. Am Surg 1995; 61: 40-44.
- Yang HR, Wang YC, Chung PK, Chen WK, Jeng LB, Chen RJ. Role of leukocyte count, neutrophil percentage, and C-reactive protein in the diagnosis of acute appendicitis in the elderly. Am Surg 2005; 71: 344-347.
- Blomqvist PG, Andersson RE, Granath F, Lambe MP, Ekbom AR. Mortality after appendectomy in Sweden, 1987-1996. Ann Surg 2001; 233: 455-460.
- Schellekens DH, Hulsewé KW, Van Acker BA, Van Bijnen AA, De Jaegere TM, Sastrowijoto SH, Buurman WA, Derikx JP. Evaluation of the diagnostic accuracy of plasma markers for early diagnosis in patients suspected for acute appendicitis. Acad Emerg Med 2013; 20: 703-710.
- Goodman DA, Goodman CB, Monk JS. Use of the neutrophil:lymphocyte ratio in the diagnosis of appendicitis. Am Surg 1995; 61: 257-259.
- Markar SR, Karthikesalingam A, Falzon A, Kan Y. The diagnostic value of neutrophil: lymphocyte ratio in adults with suspected acute appendicitis. Acta Chir Belg 2010; 110: 543-547.
- Yazici M, Ozkisacik S, Oztan MO, Gürsoy H. Neutrophil/lymphocyte ratio in the diagnosis of childhood appendicitis. Turk J Pediatr 2010; 52: 400-403.
- Jaffe BM, Berger DH. The Appendix. In: Schwartz’s. Principles of surgery 8nd ed 2005; 29: 1119-37.
- Hallan S, Asberg A. The accuracy of C-reactive protein in diagnosing acute appendicitis--a meta-analysis. Scand J Clin Lab Invest 1997; 57: 373-380.
- Chen SC, Wang SM. C-reactive protein in the diagnosis of acute appendicitis. Am J Emerg Med 1996; 14: 101-103.
- Anielski R, Cabala BK, Szafraniec K. An Evaluation Of The Utility Of Additional Tests Gn The Preoperative Diagnostics Of Acute Appendicitis. Langenbeck Arch Surg 2010; 395: 1061-1068.
- Grönroos JM, Grönroos. Leucocyte count and C-reaktive proteine in the diagnosis of acute appendicitis. Brit J Surg 1999; 86: 501-504.
- Cev M, Bozfakioglu Y. Apendiks hastaliklari. Degerli Ü (editör). Cerrahi gastroenteroloji. 2. baski. Istanbul: Nobel Tip Kitabevi 1989: 258-273.
- Burd RS, Whalen TV. Evaluation of the child with suspected appendicitis. Pediatr Ann 2001; 30: 720-725.
- Shaikh U, Rollins RC. Appendicitis in a child with paraplegia. Hospital Physcian 2001; 46-49.
- Keksek M, Tez M, Yoldas O, Acar A, Akgul O, Gocmen E, Koc M. Receiver operating characteristic analysis of leukocyte counts in operations for suspected appendicitis. Am J Emerg Med 2008; 26, 769-772.
- Wu HP, Lin CY, Chang CF, Chang YJ, Huang CY. Predictive value of C-reactive protein at different cut-off levels in acute appendicitis. Am J Emerg Med 2005; 23: 449-453.
- Yang HR, Wang YC, Chung PK, Chen WK, Jeng LB. Laboratory tests in patients with acute appendicitis. ANZ J Surg 2006; 76: 71-74.
- Sevim Y, Namdaroglu OB, Akpinar MY, Ertem AG. The Diagnostic Value of Neutrophil Lymphocyte Ratio in Acute Appendicitis. Sakarya Med J 2014; 4: 78-81.
- BiaÅas M, Taran K, Gryszkiewicz M, Modzelewski B. Evaluation of neutrophil-lymphocyte ratio usefulness in the diagnosis of appendicitis. Wiad Lek 2006; 59: 601-606.
- Terradas R, Grau S, Blanch J, Riu M, Saballs P, Castells X, Horcajada JP, Knobel H. Eosinophil count and neutrophil-lymphocyte count ratio as prognostic markers in patients with bacteremia: a retrospective cohort study. PLoS One 2012; 7: e42860.
- Ishizuka M, Shimizu T, Kubota K. Neutrophil-to-Lymphocyte Ratio Has a Close Association With Gangrenous Appendicitis in Patients Undergoing Appendectomy. Int Surg 2012; 97: 299-304.