ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2017) Volume 28, Issue 1
Mixed germ cell testicular tumour complicated with inferior vena cava tumour thrombus: A case report and review of the literature
1Department of Critical Care Medicine, The Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, Zhejiang Province, PR China
2Department of Urology, The Sir Run Run Shaw Hospital, School of Medicine, Zhejiang University, Hangzhou, Zhejiang Province, PR China
- *Corresponding Author:
- Cunjie Sun
Department of Critical Care Medicine
The Sir Run Run Shaw Hospital
Zhejiang University
Zhejiang Province, China
Accepted date: June 29, 2016
Background: Testicular Mixed Germ Cell Tumour (MGCTS) is a rarely reported. En bloc vena caval resection of involved tumours or extensive thrombosis can be associated with short- and long-term morbidity but probably prolongs tumour-free survival and enhances a chance for cure.
Materials and methods: We reported a 32-year-old male patient presenting with left mixed germ cell testicular tumour complicated with inferior vena cava (IVC) tumour thrombus. Following ultrasound detection of the testis, the patient underwent left inguinal orchiectomy, retroperitoneal lymph node dissection (RPLND), left nephrectomy followed by inferior vena cava thrombectomy. Histological examination revealed that the cancer cells were distributed in a sold flake shape with large cell body and irregular nucleus located in the left testis and abdominal cavity.
Results: Laboratory test revealed that serum level of alpha-fetoprotein (AFP) was significantly enhanced. Postoperatively, the patient had smooth postoperative recovery and had disease-free survival for 6 months.
Conclusion: Clinical efficacy was poor for advanced non-seminomatous germ cell tumour when single treatment was delivered. Comprehensive treatment, especially surgical procedure, should be chosen according to the pathological and clinical characteristics.
Keywords
Testicular mixed germ cell tumour, Inferior vena cava, Tumour thrombus.
Introduction
Testicular Mixed Germ Cell Tumour (MGCTS) is a rarely reported, which mainly occurs in male aged between 20 and 35 years [1,2]. Although testicular neoplasm constantly combines with retroperitoneal lymph node metastasis, the complication of inferior vena cava (IVC) thrombus by the testicular tumour is largely unknown. En bloc vena caval resection of involved tumours or extensive thrombosis can be associated with shortand long-term morbidity but probably prolongs tumour-free survival and enhances a chance for cure [3].
We herein reported a male presenting with left testicular tumour complicated with IVC thrombus and was surgically treated by left inguinal orchiectomy, inferior vena cava thrombectomy, Retroperitoneal Lymph Node Dissection (RPLND), followed by left nephrectomy. The operative time was 420 min and intraoperative bleeding volume was 12 000 ml.
Liver mobilization with hepatic vascular occlusion and IVC thrombectomy were performed by urologists and vascular surgeons.
Case Report
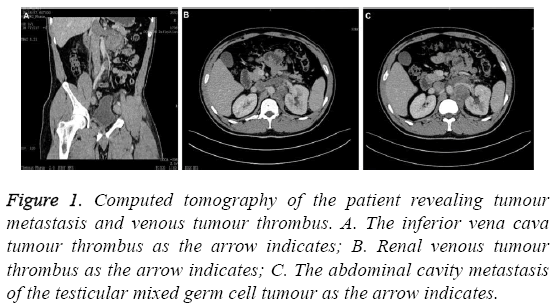
A 32-year-old male Chinese presented with chronic lower quadrant abdominal pain for 4 months and left-sided scrotal swelling for 2 days. Ultrasonography of the scrotum revealed the size of the left testis was measured 2.5 cm × 1.3 cm, which was characterized as scarce cystic elements and multiple calcifications. Colour Doppler ultrasound revealed that the left lower limb deep vein and left exterior iliac venous thrombus. Abdominal computed tomography (CT) scan demonstrated a lesion within the left testis and a metastasis mass at the left renal hilum as shown in Figure 1, surrounding the abdominal aorta and left renal artery. Multiple tumour thrombi were found in the inferior vena cava, left renal vein and bilateral iliac vein. The superior apex of the thrombus in the IVC was approximate 5 cm above the renal vein Figure 1. Physical examination revealed no symptoms related to inferior vena caval obstruction, such as leg oedema. Laboratory findings demonstrated that the concentration of serum beta-human chorionic gonadotropin (β-hCG) was 0.86 IU/L (normal range 0-3.8 IU/L) and lactic acid dehydrogenase (LDH) was 177 IU/L (normal range 60-213 IU/L). Serum level of alpha-fetoprotein (AFP) was significantly elevated up to 9867.42 ng/mL (normal range 0-13.4 ng/mL). During left inguinal orchiectomy, a mass approximately measured 1.0 cm × 1.5 cm and hoary colour was located at the lower pole of the left testicle. After one week, the patient further underwent inferior vena cava thrombectomy, RPLND, followed by left nephrectomy. Intraoperatively, tumour thrombus was detected in the inferior vena cava and left renal vein. A metastatic tumour, approximately 4.8 cm in size, was observed in the left retro peritoneum involved with the left kidney. The tumour adhered to the left kidney and abdominal aorta. Multiple swollen lymph nodes were found within the retro peritoneum.
Figure 1: Computed tomography of the patient revealing tumour metastasis and venous tumour thrombus. A. The inferior vena cava tumour thrombus as the arrow indicates; B. Renal venous tumour thrombus as the arrow indicates; C. The abdominal cavity metastasis of the testicular mixed germ cell tumour as the arrow indicates.
Laparotomy was performed using a median abdominal incision extending from the xiphoid to pubic symphysis. Splenocolic ligament was freed and the IVC and aorta were exposed. The inferior vena cava was separated straight up to the second porta. The liver was completely mobilized by the piggyback technique, dividing the falciform, triangular, and coronary ligaments, and the IVC was completely exposed to the hepatic veins. After complete hepatic mobilization and IVC crossclamping, hepatic vascular exclusion was performed to prevent bleeding from the hepatic vein and hepatic congestion. The suprahepatic IVC, infrarenal IVC, contralateral renal vein, and hepatic vein were occluded in sequence. Following administration of heparin, clamps were applied successively to the distal IVC, renal vein contralateral to the tumour, and upper IVC proximal to the thrombus. A lateral venotomy was performed from the ostium of the tumoural renal vein to the IVC beyond the proximal limit of the thrombus and the thrombus was removed under direct vision. The invasion was not detected in the inferior vena cava wall. Primary repair of the cavotomy was sutured by Prolene suture line, without prosthetic graft interposition or patch angioplasty. After closure of the IVC, radical nephrectomy and RPLND were performed. Following surgery, the patient was transferred to the intensive care unit. The surgery endured for 420 min and intraoperative bleeding loss was 12 000 ml.
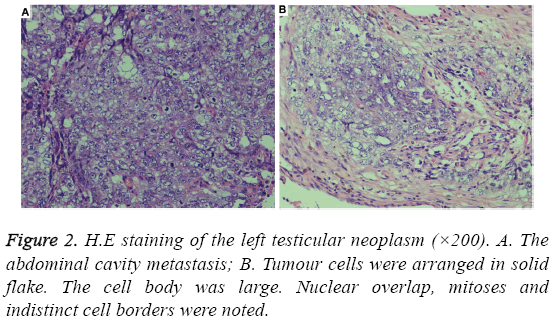
Postoperative pathological examination confirmed mixed germ cell tumours including teratoma, embryonal carcinoma and intratubular germ cell neoplasia. Hematoxylin and Eosin (H.E) staining revealed the signs of blurry cell borders, mitoses, nuclear overlap and the cells were arranged in solid flake. The abdominal mass was pathologically diagnosed with embryonal carcinoma as shown in Figure 2.
The AFP level decreased to 4530.0 ng/mL, 3 months after surgery. Chest and abdominal CT at postoperative 6 months revealed no signs of metastasis. Informed consent was obtained from this patient.
Discussion
Testicular cancer is a rare neoplasm, approximately accounting for 2% of all malignant cancers in male and a 10% of all malignant diseases affecting the male genitourinary system. Mixed germ cell tumours contain more than one germ cell component and more commonly occur than any of the pure histologic forms representing 32%-60% of all germ cell tumours. Testicular cancer complicated with IVC tumour thrombus has been extremely rarely reported. Only four cases of IVC invasion was found among 650 testicular cancer patients assessed by CT [3]. Herein we presented one male case of mixed germ cell tumour consisting of teratoma, embryonal carcinoma and intratubular germ cell neoplasia, accompanied with inferior vena cava, renal vein, iliac vein and femoral venous thrombus.
Pulmonary embolization is the most severe complication of IVC thrombus, which probably leads to sudden death. Approximately 9% of testicular cancer patients died of pulmonary embolization in autopsy cases [4]. Although complete removal of the tumour thrombus extending into the IVC exerts no effect upon clinical prognosis, the presence of the tumour thrombus is associated with poor survival rate [4]. Garcia-Fadrique G [5] assessed the clinical prognosis of venous thrombus in patients with kidney cancer. Survival analysis revealed that patients with venous thrombus and venous wall invasion had worse survival rate.
Common treatments of MGCTS include resection of the testis, epididymis and spermatic high ligation and retroperitoneal lymph node dissections. Comprehensive therapies, such as chemotherapy or radiotherapy, can be chosen according to clinical staging and pathological type. Few studies reported surgical treatment of the complication of MGCTS and IVC thrombus. However, IVC tumour thrombus in patients with renal cell carcinoma has been frequently reported [5,6]. The extent of tumour thrombus was graded at level I (i.e., extending ≤ 2 cm above the ostium of the renal vein into the IVC); level II (i.e., extending >2 cm above the ostium of the renal vein and below the intrahepatic vena cava); level III (i.e., extending into the intrahepatic portion of the vena cava, but below the diaphragm); or level IV (i.e., extending into the right atrium) [6]. According to different levels of the inferior vena cava involved by tumour thrombus and whether the venous wall was involved, different surgical methods could be properly employed accordingly. The inferior vena cava thrombectomy was performed in level I or II patients. Liver mobilization was individualized depending on thrombus extent. Liver mobilization with hepatic vascular exclusion was performed in level III patients and CPB in level IV.
CT and ultrasonography suggested that the tumour thrombus involving the inferior vena cava did not extend over the second porta. Thus, this patient was defined as level III tumour thrombus. Liver mobilization with hepatic vascular exclusion and IVC thrombectomy were chosen. Due to the multiple sites of tumour thrombus including the inferior vena cava, renal, iliac and femoral veins, it was challenging to remove all tumour thrombi. Satoru masui [7] reported one patient diagnosed with right testicular tumour complicated with IVC thrombus and was successfully treated by a temporary IVC filter besides anticoagulants during systemic chemotherapy and retroperitoneal lymph node and vena cava dissection. In our report, the male patient underwent the inferior vena cava thrombectomy, performed by urological and vascular surgeons. Postoperative recovery was satisfactory and no perioperative complications were induced. Chemotherapy has been widely accepted as an efficacious therapy of advanced testicular tumour, whereas the cure rate only achieved 50-60% for the advanced non-seminomatous germ cell tumour when operation, radiotherapy or single-agent chemotherapy is delivered, respectively. However, the cure rate was significantly increased up to 85% when combined chemotherapy of multiple agents was employed, especially after cisplatin-based combination chemotherapy became the preferred treatment [8]. According to the 7th edition of AJCC Cancer Staging Manual, the tumour of patient in our report was graded as IIb. Hence, adjuvant chemotherapy was recommended after retroperitoneal lymph node dissection [9,10]. However, the patient rejected the chemotherapy due to family member disagreement.
Clinical prognosis of MGCTS largely depends on clinical staging, histological type and treatment compliance. The survival time was reported as 20 to 132 months, with a median survival of 42 months [11]. In this report, the 32-year-old male was diagnosed with mixed germ cell tumours including teratoma, embryonal carcinoma and intratubular germ cell neoplasia. The prognosis of teratoma complicated with embryonal carcinoma was poor. According to the IGCCCGrisk classification criteria, the prognostic risk of the patient was intermediate. Additionally, he developed multiple venous thrombi and metastases in the retroperitoneal lymph nodes, and refused to receive chemotherapy. Therefore, clinical prognosis of this patient was estimated poor.
Conclusion
Testicular cancer complicated with IVC tumour thrombus is extremely rare. Clinical efficacy was poor for advanced nonseminomatous germ cell tumour when single treatment was delivered. Hence, comprehensive treatment, especially surgical procedure, should be chosen according to the pathological and clinical characteristics.
Conflict of Interest
The authors declare that there is no conflict interest.
References
- Spitz A, Wilson TG, Kawachi MH, Ahlering TE, Skinner DG. Vena caval resection for bulky metastatic germ cell tumours: an 18-year experience. J Urol 1997; 158: 1813-1818.
- Leow WQ, Loh HL, Lee LS, Goh CH. A rare case of combined placental site trophoblastic tumour with mature cystic teratoma and mixed germ cell tumour in the testis. Malays J Pathol 2015; 37: 145-147.
- Husband JE, Bellamy EA. Unusual thoracoabdominal sites of metastases in testicular tumours.Am J Roentgenol 1985; 145: 1165-1171.
- Moinzadeh A, Libertino JA. Prognostic significance of tumour thrombus level in patients with renal cell carcinoma and venous tumour thrombus extension. Is all T3b the same. J Urol 2004; 171: 598-601.
- Garcia-Fadrique G, Budía-Alba A, Ruiz-Cerda JL, Morales-Solchaga G, Pontones JL, Jimenez-Cruz JF. Prognostic value of venous tumour thrombus in renal cell carcinoma. Actas Urol Esp2012; 36: 29-34.
- Kwon TW, Kim H, Moon KM, Cho YP, Song C, Kim CS, Ahn H. Surgical treatment of inferior vena cava tumour thrombus in patients with renal cell carcinoma. J Korean Med Sci 2010; 25: 104-109.
- Masui S, Onishi T, Arima K, Sugimura Y. Successful management of inferior vena cava thrombus complicating advanced germ cell testicular tumour with temporary inferior vena cava filter. Int J of Urol 2005; 12: 513-515.
- Willams SD, Roth BJ. Chemotherapy of testis cancer: a review. Int Radiate Oncol Biol Phys 1992; 22: 213.
- Stephenson AJ, Bosl GJ, Bajorin DF, Stasi J, Motzer RJ, Sheinfeld J. Retroperitoneal lymph node dissection in patients with low stage testicular cancer with embryonal carcinoma predominance and/or lymphovascular invasion. J Urol 2005; 174: 557-560.
- Kondagunta GV, Sheinfeld J, Mazumdar M, Mariani TV, Bajorin D, Bacik J, Bosl GJ, Motzer RJ. Relapse-free and overall survival in patients with pathologic stage II nonseminomatous germ cell cancer treated with etoposide and cisplatin adjuvant chemotherapy. J Clin Oncol 2004; 22: 464-467.
- Kuo JY, Chin T, Hsieh YL, Lin AT, Chang YH, Wei C, Chen KK, Chang LS. Observations after orchiectomy in clinical stage I nonseminomatous germ cell tumours of the testis. Chung Hua I Hsueh Tsa Chih 1999; 62: 356-361.