ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Case Report - Biomedical Research (2017) Volume 28, Issue 11
L-shaped tibial condylar valgus osteotomy for advanced medial knee osteoarthritis: A case report
Hironobu Koseki1*, Akihiko Yonekura2, Hidehiko Horiuchi2, Chieko Noguchi2, Takashi Higuchi1 and Makoto Osaki2
1Department of Locomotive Rehabilitation Science, Nagasaki University Graduate School of Biomedical Sciences, 1-7-1, Sakamoto, Nagasaki 852-8520, Japan
2Department of Orthopedic Surgery, Nagasaki University Graduate School of Biomedical Sciences, 1-7-1, Sakamoto, Nagasaki 852-8501, Japan
- *Corresponding Author:
- Hironobu Koseki
Department of Locomotive Rehabilitation Science
Nagasaki University Graduate School of Biomedical Sciences
1-7-1, Sakamoto
Nagasaki, 852-8520, Japan
Accepted on March 27, 2017
Case: A 63 year-old woman with bilateral severe medial knee osteoarthritis, huge cartilaginous defects, and severe varus-valgus instability was treated by tibial condylar valgus (TCV) osteotomy. Her preoperative point of the weight-bearing (mechanical) axis was right -19% and left -20%. After surgery, the mechanical axis was right 60% and left 61% with a high degree of patient satisfaction.
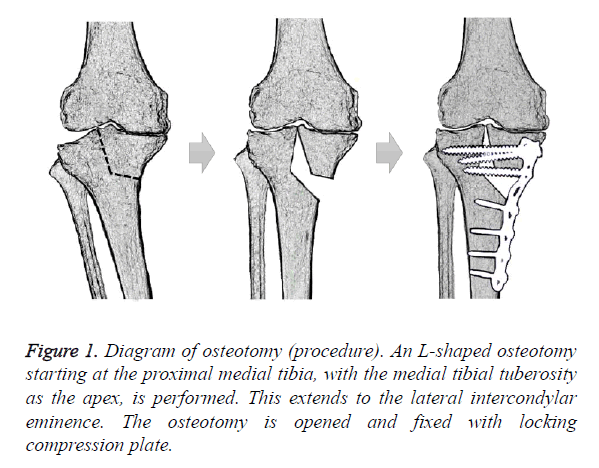
Conclusion: The TCV osteotomy technique consists of an L-shape osteotomy from the medial aspect of the proximal tibia to the intercondylar eminence. Corrected limb alignment and improved joint congruity can distribute the weight bearing force, stabilize the joint, and relieve pain of advanced medial knee osteoarthritis.
Keywords
Osteoarthritis, Knee, Osteotomy
Introduction
Surgery for advanced medial unicompartmental knee osteoarthritis (OA) is attracting considerable attention, and the value of osteotomy and of prosthetic arthroplasty has recently been discussed [1-3]. The longevity of total knee arthroplasty (TKA) is increasing with advances in materials and designs, and TKA is now indicated for patients over a wide age range [2]. However, with TKA, there is concern about complications such as implant-associated infections, the risk of metal allergies, and wear of the prosthesis. Moreover, problems with material durability and patient dissatisfaction with joint range of motion (ROM) can also occur, especially in young, active patients [4,5]. Therefore, in young and active patients maintaining wide ROM, or high-demand individuals who want to avoid prosthetic implant arthroplasty and preserve their native knee joints, a high tibial osteotomy (HTO), which is the most widely accepted osteotomy procedure, is indicated [1,6,7]. HTO is based on the concept of realignment to redistribute weight bearing and mechanical stress laterally to areas with less degeneration, thus relieving pain and improving function. The medial approach open-wedge HTO has gained popularity because it overcomes some of the complications associated with lateral closed-wedge HTO, such as tibiofubular joint disruption and peroneal nerve injury [6,8,9]. Even in open-wedge HTO, however, risks include loss of correction or over correction due to implant loosening and nonunion [1,10]. In addition, effects on the patellofemoral (PF) joint, limited knee extension, a see-saw phenomenon, and disease progression due to ligamentous joint laxity are also concerns [9,11-13]. Therefore, the indication for HTO is restricted only to patients with mild to moderate medial knee OA maintaining high stability [14,15].
Tibial condylar valgus (TCV) osteotomy, a novel L-shaped osteotomy, also corrects lower extremity alignment (shifts the weight-bearing (mechanical) axis laterally) at high in the tibia [16]. TCV osteotomy together with remodeling the shape of the tibial plateau can improve femorotibial joint congruity and stability. Therefore, the combined features of osteotomy and arthroplasty are promising for effective treatment of severe knee OA (gonarthrosis). To date, however, only a limited number of studies have examined clinical results of osteotomies in advanced OA cases [9,17,18] and there have not been identified TCV osteotomy case report in the international journal.
A defiant case of severe medial osteoarthritis (Kellgren– Lawrence classification grade 4) with TCV osteotomy is presented, along with some discussion of recently reported research. This study was approved by the ethics committee of the Nagasaki University Graduate School of Biomedical Sciences (number: 2015-15082031), and the patients provided their informed consent and agreed with having their data published.
Surgical Procedure
An oblique skin incision was made distomedially from the medial aspect of the tibial tuberosity, and the pes anserinus and superficial layer of the medial collateral ligament (MCL) were dissected subperiosteally. The osteotomy was started horizontally at a point 3.5 cm distally from the medial tibial plateau. In the next step, the direction of the chisel was changed at the medial margin of the tibial tuberosity toward the center of the lateral intercondylar eminence. A mild valgus force was applied to the leg, and completion of the osteotomy was confirmed by intraoperative radiographic imaging. A Kirschner wire was inserted to prevent separation of the tibial plateau, and stoppers were attached to both ends. The osteotomy was opened with a gradual valgus force until the lateral joint was repositioned (Figure 1). After the correction, the Tomofix™ plate (DePuy Synthes, West Chester, PA) was placed on the anteromedial aspect of the tibia, and locking screws were inserted sequentially. The opened gap space was filled with granular β-TCP. After irrigation, the surgical wound was closed.
Case Report
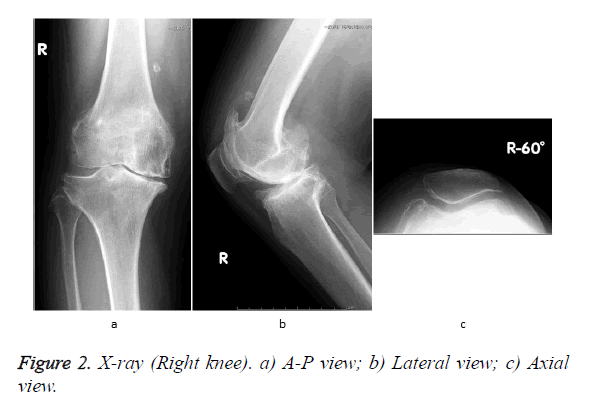
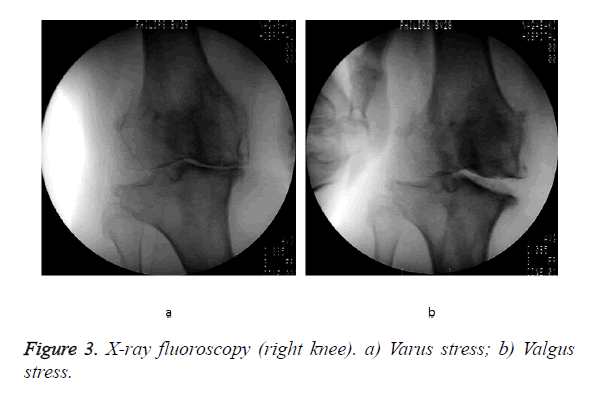
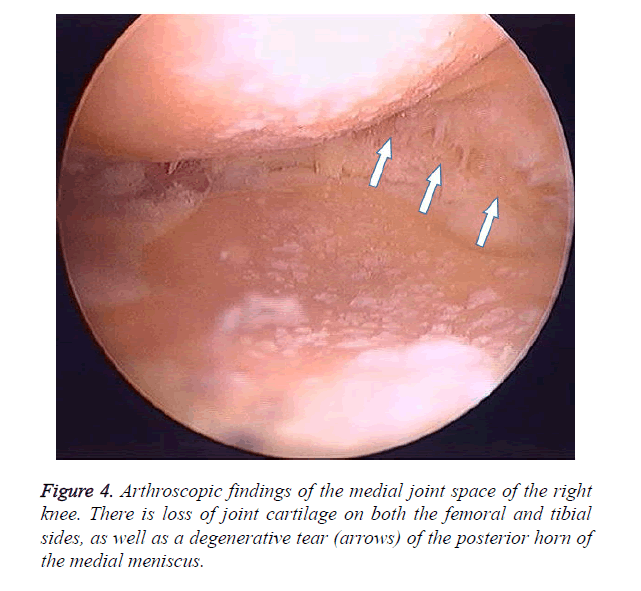
A 63-year-old working woman with bilateral knee OA for about 10 years was being treated conservatively, including joint injections. However, her symptoms gradually worsened, and walking ability decreased due to pain and limited joint mobility. She was able to walk continuously less than 100 meters and barely go up and down stairs one-by-one while holding a handrail. She felt severe right knee pain, especially when going downstairs. Right knee joint ROM was relatively maintained (-5° extension to 115° flexion), but plain radiographs showed Kellgren–Lawrence (K-L) grade 4 OA (Figures 2a-2c). On a standing A-P view, the point of the mechanical axis was -19% from the medial tibial articular margin [19,20]. After sufficient informed consent, the patient refused TKA and then we performed TCV osteotomy on her right knee. In operation, Imaging with varus-valgus stress under anesthesia showed severe joint instability from 6.1° varus to 5.9° valgus (magnitude 10°) (Figure 3). Right knee arthroscopy showed anterior cruciate ligament loss. The Outerbridge-Brittberg classification for cartilage damage was grade IV for the medial femoral condyle and tibial medial articular surface, and grade III for the femoral trochlea. The degenerative change and horizontal tear were observed in medial meniscus (Figure 4).
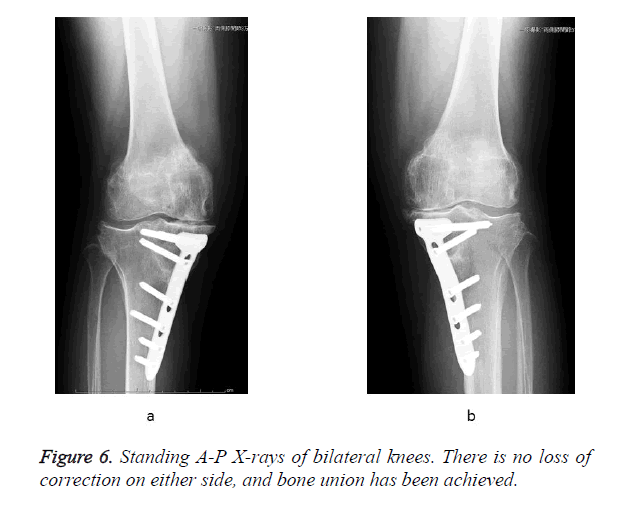
The TCV osteotomy site was opened to 17 mm (operative time, 2 h 39 min; blood loss, 50 g). A compression bandage and foot pump was used immediately after surgery. The patient began seated posture training and wheelchair transfer training the day after surgery. At 2 weeks postoperatively, 1/3 weight-bearing walking training was started and increased each week to 1/2 and 2/3 weight-bearing; full weight-bearing was allowed after 6 weeks. The patient had a satisfactory postoperative course with improved leg alignment, reduced knee pain, and knee joint stabilization. One year after surgery, she returned to previous work. ROM was: right knee, -10° extension to 105° flexion; left knee, -5° extension to 125° flexion and the mechanical axis was: right 60% and left -20%. There was disease progression on the left knee (Figure 5). The patient desired TCV osteotomy on her left side earnestly, therefore, we performed the same procedure with opening of the osteotomy site to 14 mm (operative time, 2 h 42 min; blood loss, 20 g). Thirty months after surgery of the right knee (18 months after surgery of the left knee), ROM was: right knee, 0° extension to 105° flexion; left knee, 0° extension to 120° flexion. Bone union was completed at the osteotomy site and the mechanical axis was: right 60% and left 61% (Figure 6). Arthroscopy findings of right knee at the time revealed white structures indicating articular cartilage was regenerated on the femoral medial condyle and tibial medial articular surface. The Knee Injury and Osteoarthritis Outcome Score (KOOS) [21], including a visual analogue scale (VAS) for pain, indicated a high degree of patient satisfaction (Table 1).
Discussion
Surgical treatment is now indicated in patients with knee OA refractory to conservative treatment. HTO is often indicated in relatively younger patients who are highly active, including patients with relatively wide knee ROM, and to avoid prosthetic implant arthroplasty [1,6,7]. With recent advances in internal fixation devices and bone substitutes, HTO has become less invasive, enabling earlier bone union and rehabilitation [10,22]. However, HTO outcomes are not always satisfactory in patients with severe degenerative or unstable OA knee with lateral thrust phenomenon [1,9,11-13]. In contrast, the cut line of TCV osteotomy is limited within the medial tibial condyle, so lateral weight-bearing is unlikely to cause a loss of correction. Moreover, congruity of the medial and lateral knee joint is improved, so weight bearing force is distributed. In addition, because the shape of the tibial plateau becomes more concave, the femoral condyle is wedged from both sides, and together, joint stability can be achieved [16].
The present patient’s knee had severe degeneration and joint instability, but she hope to avoid prosthetic implant arthroplasty. She was still relatively young and active patient, and her joint ROM was maintained. Because lateral joint structure was preserved, treatment outcome with TCV osteotomy was thought to be satisfied. If the anterior cruciate ligament had been preserved, stability may have improved even further. When the concept of TCV osteotomy is considered, a good outcome might be expected even if the mechanical axis is not necessarily placed as laterally as with HTO. The magnitude of varus/valgus stress under anesthesia can serve as a guide to the angle that can be corrected by TCV osteotomy. Leaving the mechanical axis in the medial half of the tibial plateau should be strictly avoided, because there is increased risk of promoting even further medial degeneration.
Therefore, when the mechanical axis does not shift laterally with TCV osteotomy alone, additional HTO can be performed as an option. Another issue with HTO include increased PF joint surface pressure (open wedge HTO) or reduced tension on the extensor mechanism (closed wedge HTO). The effect on the PF joint and extensor mechanism of TCV osteotomy is thought to be minimal compared to HTO, since the change in leg length with TCV osteotomy is less than with HTO. The present patient also had grade III cartilage damage of the PF joint, but she had no postoperative progression or complaints on both PF joints.
With this procedure to cut into the joint and modify joint shape, correction loss or overcorrection, non-union or mal-union due to implant loosening may occur to the same extent as HTO method. Therefore, weight bearing should be prohibited for 1 to 2 weeks. Currently, young generations are often obese and get little exercise, thus raising the concern of developing knee OA at younger ages. With increasing efforts to reduce medical costs, the demand for osteotomy, which is less expensive than prosthetic joint arthroplasty, may increase. Therefore, TCV osteotomy may be useful in patients with severe OA in whom HTO is not indicated. This can further increase the value of TCV osteotomy as a therapeutic surgical option for advanced knee OA.
References
- Amendola A, Bonasia DE. Results of high tibial osteotomy: review of the literature. Int Orthop 2010; 34: 155-160.
- Belmont PJ, Heida K, Keeney JA, Hamilton W, Burks R, Waterman BR. Return to Work and Functional Outcomes Following Primary Total Knee Arthroplasty in US Military Servicemembers. J Arthroplasty 2015; 30: 968-972.
- Hochberg MC, Altman RD, Brandt KD, Clark BM, Dieppe PA, Griffin MR, Moskowitz RW, Schnitzer TJ. Guidelines for the medical management of osteoarthritis. Part II. Osteoarthritis of the knee. American College of Rheumatology. Arthritis Rheum 1995; 38: 1541-1546.
- Papakostidou I, Dailiana ZH, Papapolychroniou T, Liaropoulos L, Zintzaras E, Karachalios TS, Malizos KN. Factors affecting the quality of life after total knee arthroplasties: a prospective study. BMC Musculoskelet Disord 2012; 13: 116.
- Werner BC, Evans CL, Carothers JT, Browne JA. Primary Total Knee Arthroplasty in Super-obese Patients: Dramatically Higher Postoperative Complication Rates Even Compared to Revision Surgery. J Arthroplasty 2015; 30: 849-853.
- Rossi R, Bonasia DE, Amendola A. The role of high tibial osteotomy in the varus knee. J Am Acad Orthop Surg 2011; 19: 590-599.
- Feeley BT, Gallo RA, Sherman S, Williams RJ. Management of osteoarthritis of the knee in the active patient. J Am Acad Orthop Surg 2010; 18: 406-416.
- Gardiner A, Gutiérrez Sevilla GR, Steiner ME, Richmond JC. Osteotomies about the knee for tibiofemoral malalignment in the athletic patient. Am J Sports Med 2010; 38: 1038-1047.
- Gstöttner M, Pedross F, Liebensteiner M, Bach C. Long-term outcome after high tibial osteotomy. Arch Orthop Trauma Surg 2008; 128: 111-115.
- Giuseffi SA, Replogle WH, Shelton WR. Opening-Wedge High Tibial Osteotomy: Review of 100 Consecutive Cases. Arthroscopy 2015; 31: 2128-2137.
- Rudan JF, Simurda MA. High tibial osteotomy. A prospective clinical and roentgenographic review. Clin Orthop Relat Res 1990; : 251-256.
- Naudie D, Bourne RB, Rorabeck CH, Bourne TJ. The Install Award. Survivorship of the high tibial valgus osteotomy. A 10- to -22-year followup study. Clin Orthop Relat Res 1999; 42: 18-27.
- Cantin O, Magnussen RA, Corbi F, Servien E, Neyret P, Lustig S. The role of high tibial osteotomy in the treatment of knee laxity: a comprehensive review. Knee Surg Sports Traumatol Arthrosc 2015; 23: 3026-3037.
- Bonasia DE, Dettoni F, Sito G, Blonna D, Marmotti A, Bruzzone M, Castoldi F, Rossi R. Medial Opening Wedge High Tibial Osteotomy for Medial Compartment Overload/Arthritis in the Varus Knee Prognostic Factors. Am J Sports Med 2014; 42: 690-698.
- Trieb K, Grohs J, Hanslik-Schnabel B, Stulnig T, Panotopoulos J, Wanivenhaus A. Age predicts outcome of high-tibial osteotomy. Knee Surg Sports Traumatol Arthrosc 2006; 14: 149-152.
- Chiba K, Yonekura A, Miyamoto T, Osaki M, Chiba G. Tibial condylar valgus osteotomy (TCVO) for osteoarthritis of the knee: 5-year clinical and radiological results. Arch Orthop Trauma Surg 2017; 137: 303-310.
- Harris JD, McNeilan R, Siston RA, Flanigan DC. Survival and clinical outcome of isolated high tibial osteotomy and combined biological knee reconstruction. Knee 2013; 20: 154-161.
- Schuster P, Schulz M, Mayer P, Schlumberger M, Immendoerfer M, Richter J. Open-Wedge High Tibial Osteotomy and Combined Abrasion/Microfracture in Severe Medial Osteoarthritis and Varus Malalignment: 5-Year Results and Arthroscopic Findings After 2 Years. Arthroscopy 2015; 31: 1279-1288.
- Staubli AE, De Simoni C, Babst R, Lobenhoffer P. TomoFix: a new LCP-concept for open wedge osteotomy of the medial proximal tibia--early results in 92 cases. Injury 2003; 34 Suppl 2: B55-62.
- Nakamura R, Komatsu N, Murao T, Okamoto Y, Nakamura S, Fujita K, Nishimura H, Katsuki Y. The validity of the classification for lateral hinge fractures in open wedge high tibial osteotomy. Bone Joint J 2015; 97-97B: 1226-31.
- Roos EM, Roos HP, Lohmander LS, Ekdahl C, Beynnon BD. Knee Injury and Osteoarthritis Outcome Score (KOOS)--development of a self-administered outcome measure. J Orthop Sports Phys Ther 1998; 28: 88-96.
- Kyung HS, Lee BJ, Kim JW, Yoon SD. Biplanar Open Wedge High Tibial Osteotomy in the Medial Compartment Osteoarthritis of the Knee Joint: Comparison between the Aescula and TomoFix Plate. Clin Orthop Surg 2015; 7: 185-190.