ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2016) Volume 27, Issue 4
Kikuchi disease associated with Group C Streptococcus: a case report
1Lucian Blaga University of Sibiu, Faculty of Medicine Sibiu, Academic Emergency Hospital Sibiu, Romaina
2Lucian Blaga University of Sibiu, Faculty of Medicine Sibiu, Foisor Clinical Hospital of Orthopedics, Romania
3Department of Pathology, Academic Emergency Hospital Sibiu, Romania
- *Corresponding Author:
- Rares-Mircea Bîrluţiu
Faculty of Medicine Sibiu, Lucian Blaga University of Sibiu, Romania
E-mail: raresmirce@gmail.com
Accepted on April 01, 2016
Kikuchi-Fujimoto disease is an idiopathic histiocytic necrotizing lymphadenitis with an autoimmune component triggered by the involvement of CD8 cytotoxic T lymphocyte due to a genetic predisposition. Cases are diagnosed more frequently in female patients, especially in young adults, in all races, more commonly in East Asia, and only isolated in Europe and America. We present the case of a 51-years-old Caucasian male, diagnosed with Kikuchi disease associated with the evolution of a Group C Streptococcus pharyngitis.
Keywords
Kikuchi disease, Group C Streptococcus pharyngitis, Male patient.
Introduction
Kikuchi-Fujimoto disease, or Kikuchi Disease (KD), is an idiopathic histiocytic necrotizing lymphadenitis, which most commonly has a laterocervical localization; it was independently described in 1972 in Japan by Kikuchi and Fujimoto, having a benign outcome in most cases, limited to a few weeks or months of evolution. The trigger of this syndrome is, most likely, admitted to be an infectious one, with an autoimmune component triggered by the involvement of CD8 cytotoxic T lymphocyte [1] due to a genetic predisposition, and the involvement of gamma interferon and interleukin-6. In the literature, there are described cases associated with streptococcal Group A, herpes simplex viruses type 1 and type 2, Cytomegalovirus, Epstein Barr Virus [2], human herpesvirus 6 and 8 [3], parvovirus B19 [4], varicellazoster virus, paramyxovirus, and parainfluenza virus infections. Cases were diagnosed in all races, more commonly described in East Asia, and only isolated in Europe and America and mainly involving the female gender. We present the case of a 51-years-old Caucasian male, diagnosed with Kikuchi disease associated in the evolution of a Group C Streptococcus pharyngitis.
Case Presentation
A 51-years-old Caucasian male, is hospitalized in the Infectious Diseases Department accusing: chills, fever 40°C, dysphagia, headache, myalgia, bilateral laterocervical lymphadenopathy in the anterior triangle. As family history, the mother is known with sarcoidosis; from the personal history of the patient nothing significant was reported. He comes from an outbreak of respiratory infection with betahemolytic Group C Streptococcus present in the throat swab culture of the patient and also in other two cases. The physical examination revealed no significant changes except for a hyperemic pharynx, laterocervical lymphadenopathies of about 2 cm, which were mobile within the overlaying and underlying surface plans, spontaneously sensitive and also sensitive at touching.
After 14 days of treatment with clarithromycin 1 g/day, the evolution is favorable and the therapy is ceased. One day after antibiotic therapy is ceased, fever reappears with a progressive increase in size of the left laterocervical lymphadenopathy up to around 4-5 cm, which becomes adherent to both superficial and deep surfaces, without any tendency of regress in the next 4 weeks, during which a scheme with antibiotics and Nonsteroidal Anti-Inflammatory Drugs (NSAIDs) is repeatedly recommended.
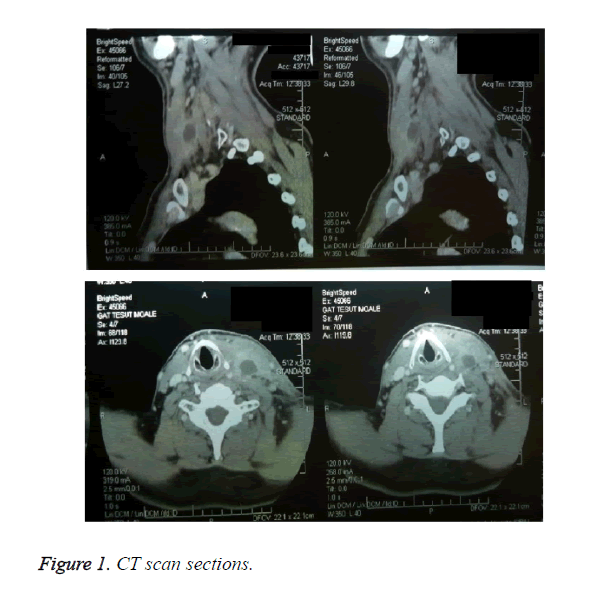
Laboratory examinations at 2 months after the streptococcal pharyngitis revealed the following alterations: C-Reactive Protein (CRP) 142.48 mg/L, fibrinogen 7.067 g/L, Erythrocyte Sedimentation Rate (ESR) 73 mm/h, white blood cells count 20.63 × 109/L, neutrophils count 14.01 × 109/L, Alanine Aminotransferase (ALT) 80 U/L (references values 20-43), and Lactate Dehydrogenase (LD) 265 U/L (references values 135-225). A Computerized Tomography (CT) scan was performed and confirmed the presence of multiple, bilateral, profound laterocervical lymphadenopathy with a maximum diameter of 1.2 cm and a left necrotic laterocervical lymphadenopathy block in the proximity of the cricoid cartilage of 4/2.7 cm (Figure 1). No mediastinal lymph nodes are present.
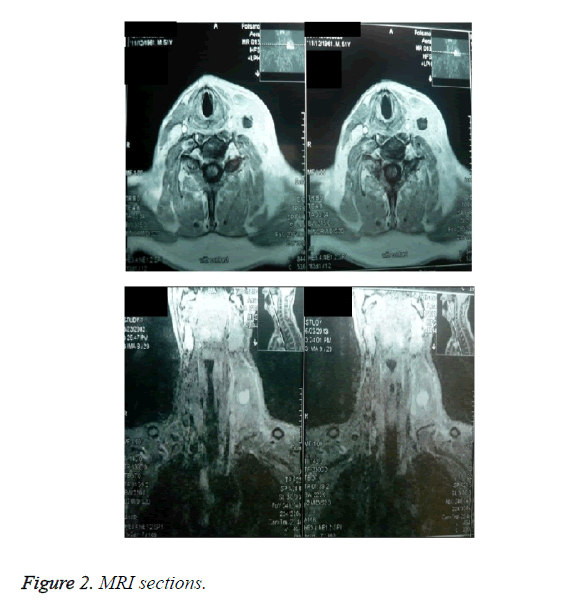
A cervical Magnetic Resonance Imaging (MRI) was performed and the findings were: cervical, bilateral, laterocervical lymph nodes varying in size from 9 to 12 mm, the largest being a jugulodigastric left lymphadenopathy, left necrotic laterocervical lymph nodes with left myositis of the sternocleidomastoid muscle (Figure 2).
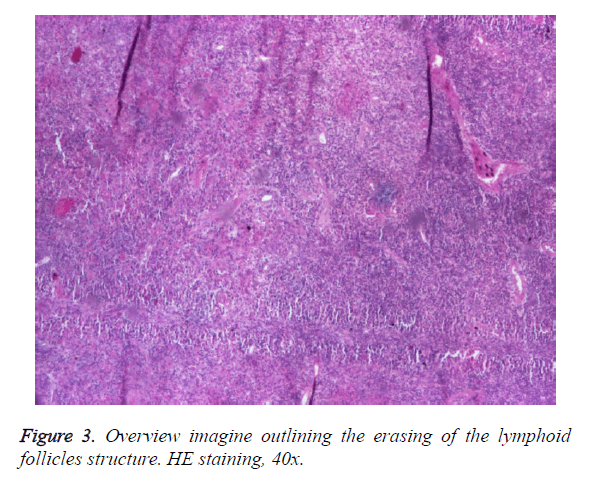
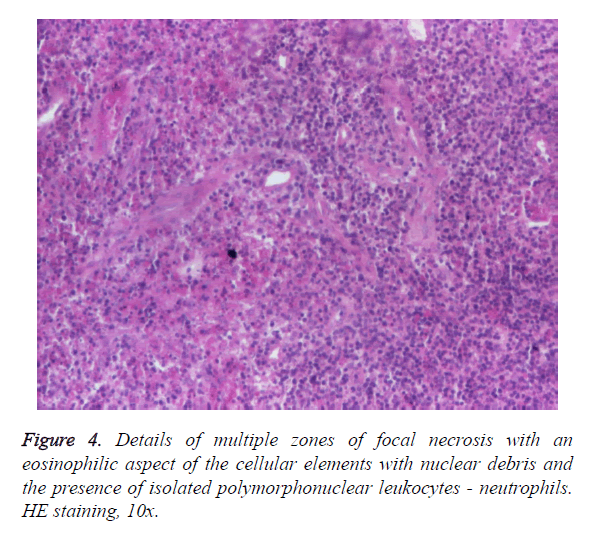
We excluded the with the evolution of infections like: Cytomegalovirus, Epstein Barr Virus, parvovirus B19, HIV, syphilis, tuberculosis, sarcoidosis, or collagen diseases, lymphoma, leukemia, tumors, toxoplasmosis, bartonellosis, and Still's disease. The evolution was slowly favorable within three weeks and surgical excision was required. The histopathological examination revealed the presence of eosinophils, rare lymphocytes and polymorphonuclear leukocytes, and the microbiological examination of the reveled sterile cultures. The histopathological examination report showed: microscopic examination: fragments of small lymph nodules with follicular structure mostly erased, with area of lymphocyte reaction. Constantly, in all lymph nodes fragments appear foci of necrosis of various sizes with ghost like aspect, eosinophilic cellular elements, with the presence of nuclear debris without around inflammatory reaction (polymorphonuclear leukocytes, eosinophils). Focal presence of mitosis. Without epithelioid reaction. Without the presence of atypical cells. Postcapillary venules hyperplasia. Histopathological diagnosis- reactive lymphoid changes within a necrotizing Kikuchi-Fujimoto lymphadenopathy, shown in Figures 3 and 4.
Also immunohistochemistry studies were performed on formalin-fixed, paraffin-embedded sections of small lymph nodes. Stains were performed using antibodies directed against the following antigens: CD3+ T cell population in the T cell reactive population, CD5+ in the lymphocytes population with overlaying CD3+ lymphocytes, CD10+ in the existing lymph node germinal centers and CD10- in the lymphocytes population, CD20+ in the lymphocytes population and CD20+ at the level of the dendritic cells of the germinal centers, CD30+ in rare activated immunoblasts, BCL2+ in the lymphocytes population, Ki67: ranging from 10 to 30% in the paracortical region and 60% in the remaining germinal centers and fail to stain with the other antibodies tested. These results support the diagnosis.
Discussion
KD is an entity encountered especially in the female gender, with a variable sex ratio (female to male) according to the literature from 3:1 to 1.25:1, especially in young adults; few studies revealed the presence in pediatric patients, predominantly in boys [5,6]. The clinical picture is dominated by fever, usually unilateral laterocervical lymphadenopathy, in 50% of the cases is preceded by a flu-like syndrome. Other less frequent manifestations are: headache, myalgia, arthralgia, dyspepsia, abdominal and thoracic pain; axillary, mesenteric, mediastinal, retrocrural, intraparotid, and celiac lymph nodes, hepatomegaly, splenomegaly, rash [7,8], exceptionally neurological manifestations like aseptic meningitis [9], encephalitis or cerebellar ataxia [10] and so on, sweating and weight loss. In terms of pathogenesis, is suggested the involvement of a genetic predisposition that is related to the Human Leukocyte Antigen (HLA) genes (from the major histocompatibility complex (MCH) - class II genes), genes that are responsible for a hyper-immune response through cytotoxic T lymphocytes, apoptotic cell and secondary lymphadenitis.
The histology appearance is similar regardless of the trigger of KD, with histiocytes, plasmocytoid monocyte (CD123+, CD68+, BCL2-), macrophages, immunoblasts-CD8 and CD4-T lymphocytes, paracortical/interfollicular necrosis and extracellular debris, usually without neutrophils, plasma cells, or granulomas. There is no specific diagnostic method, the histopathological examination being considered the gold standard - showing the presence of histiocytes, monocytes, plasma cells in the absence or with a reduced number of neutrophils [11]. In case of a type 1 or type 2 herpes simplex infection, at the anatomopathological examination of the involved lymph nodes, is distinguished the cytopathogenic effect caused by viral invasion, and the presence of viral inclusions. The histopathological features of the Epstein-Barr virus infection are focused on the expansion of the interfollicular areas by an important immunoblastic proliferation, areas of polymorphous infiltrate, plasma cells, and varying degrees of necrosis, resulting in a distortion of the normal tissue architecture. The lymphadenopathy associated with Toxoplasma gondii infection, is histopathological characterized by the presents of a histiocytic infiltrate and peripheral granulomas, the histopathological changes that appear in tuberculosis are characterized by a granulomatous, and necrotic appearance, changes that appear also in leprosy, syphilis and histoplasmosis.
The histopathological features in the presence of bacterial infections are dominated by the presence of neutrophils except for the infections caused by Yersinia where eosinophils are predominant. Usual, laboratory examinations, more frequently, highlight leukopenia, rarely leukocytosis [6], increased ESR, and CRP levels. The recommended treatment is with NSAIDs; for cases presenting fever for over two weeks, corticosteroids are recommended and sometimes in combination with immunosuppressant therapy. Pairing glucocorticoids and immunoglobulins seems to be beneficial in preventing fatal evolution [12,13]. The evolution is a self-limiting one, for about 1-6 months, so surgery is considered useful only for diagnostic purposes. There are 4 deaths of KD described in the literature, through a lupus-like manifestation, with liver and lung impairment or hemophagocytic syndrome [14]. KD requires several years of observation of the patients due to the risk of recurrence or development of systemic lupus erythematosus - SLE [15] 5 years after diagnosis [5]. What makes this case particular is the presence of KD in a male gender patient, aged over 40 years with an identified infectious trigger as a beta-hemolytic Group C Streptococcus and an unfavorable initial response to NSAIDs therapy. The problem of positive diagnosis was one that raised particular interest because of the exclusion of tumors, collagen diseases, and sarcoidosis in a patient with sarcoidosis in the family history. The laboratory examinations revealed an important inflammatory syndrome, with significant leukocytosis, which is unusual in the KD evolution. The evolution was favorable under glucocorticoids, the surgical intervention and the anatomic pathological examination being able to confirm the KD.
Conclusion
Although considered the preserve of the female gender and younger patients, KD can also occur in patients over 40, the cases in this group being most likely to be underdiagnosed. Diagnostic problems are rather due to the exclusion of different benign, malignant tumors, collagen diseases, viral infections, tuberculosis etc. and performing the histopathological examination remains the gold standard in the diagnosis. The evolution is generally favorable, self-limited for in 1-6 months, and rarely possible with a fatal development. Former patients require a subsequent observation due to the risk of association with SLE in the evolution. The therapy is a nonspecific one, nonsteroidal anti-inflammatory drugs being recommended; the cases with severe symptoms require corticosteroids associated with immunosuppressive medication.
Consents
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. The study was accepted by the Ethics Committee of the hospital and they encourage publishing the article. A copy of the written consent is available for review by the Editor-in- Chief of this journal.
References
- Ura H, Yamada N, Torii H, Imakado S, Iozumi K, Shimada S. Histiocytic necrotizing lymphadenitis (Kikuchi’s disease): the necrotic appearance of the lymph node cells is caused by apoptosis. J Dermatol 1999; 26: 385-389.
- Yen A, Fearneyhough P, Raimer SS, Hudnall SD. EBV-associated Kikuchi’s histiocytic necrotizing lymphadenitis with cutaneous manifestations. J Am Acad Dermatol 1997, 36: 342-346.
- Huh J, Kang GH, Gong G, Kim SS, Ro JY, Kim CW. Kaposi’s sarcoma-associated herpesvirus in Kikuchi’s disease. Hum Pathol 1998; 29: 1091-1096.
- Yufu Y, Matsumoto M, Miyamura T, Nishimura J, Nawata H, Ohshima K. Parvovirus B19-associated haemophagocytic syndrome with lymphadenopathy resembling histiocytic necrotizing lymphadenitis (Kikuchi’s disease). Br J Haematol 1997; 96: 868-871.
- Hsin-Ching Lin, FARS, Chih-Ying Su, Shun-Chen Huang. Kikuchi's Disease in Asian Children. Pediatrics 2005; 115: e92 -e96.
- Lin HC, Su CY, Huang CC, Hwang CF, Chien CY. Kikuchi's disease: a review and analysis of 61 cases. Otolaryngol Head Neck Surg 2003; 128: 650- 653.
- Atwater AR, Longley BJ, Aughenbaugh WD. Kikuchi's disease: case report and systematic review of cutaneous and histopathologic presentations. J Am Acad Dermatol 2008;59: 130-136.
- Yasukawa K, Matsumura T, Sato-Matsumura KC, Takahashi T, Fujioka Y, Kobayashi H, Shimizu H. Kikuchi's disease and the skin: case report and review of the literature. Br J Dermatol 2001; 144: 885-889.
- Sato Y, Kuno H, Oizumi K. Histiocytic necrotizing lymphadenitis (Kikuchi's disease) with aseptic meningitis. J Neurol Sci 1999; 163: 187-191.
- Moon JS, Il Kim G, Koo YH, Kim HS, Kim WC, Kim OJ, Oh SH. Kinetic tremor and cerebellar ataxia as initial manifestations of Kikuchi-Fujimoto’s disease. J Neurol Sci 2009; 277: 181-183.
- Tsang WYW, Chan JKC, Ng CS. Kikuchi's lymphadenitis. A morphologic analysis of 75 cases with special reference to unusual features. Am J Surg Pathol 1994; 18: 219- 231.
- Lin DY, Villegas MS, Tan PL, Wang S, Shek LP. Severe Kikuchi’s disease responsive to immune modulation. Singapore Med J 2010; 51: e18-e21.
- Quintas-Cardama A, Fraga M, Cozzi SN, Caparrini A, Maceiras F, Forteza J. Fatal Kikuchi-Fujimoto disease: the lupus connection. Ann Hematol 2003; 82: 186-188.
- Kampitak T. Fatal Kikuchi-Fujimoto disease associated with SLE and hemophagocytic syndrome: a case report. Clin Rheumatol 2008, 27: 1073-1075.
- Vivekanandarajah A, Krishnarasa B, Hurford M, Gupta S. Kikuchi’s Disease: A Rare Cause of Fever and Lymphadenopathy Clin Med Insights Pathol 2012; 5: 7-10.