ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2016) Volume 27, Issue 4
Hyperacute destruction of the femoral head after corticosteroid injections in idiopathic osteonecrosis of the femoral head: a case report
Department of Orthopedic Surgery, Hallym University Medical Center, South Korea
- *Corresponding Author:
- Jihyo Hwang
Department of Orthopedic Surgery
Hallym University Medical Center
Korea
Accepted date: April 17, 2016
We report hyperacute resorption of the femoral head within six weeks after triple corticosteroid injections. A 65-year-old male patient had bilateral idiopathic osteonecrosis proven by magnetic resonance imaging, and the unilateral pain was controlled with three separate corticosteroid injections. The clinical progression deteriorated, so the patient was transferred to our hospital six weeks later. The imaging studies and blood tests showed a destructive femoral head as well as bone marrow changes in the ipsilateral distal femur. The patient reported severe pain in the hip joint, and a cementless total hip arthroplasty was conducted. The postoperative histopathological findings revealed osteonecrosis of the femoral head and the distal femur. The authors found the rapid destruction of the femoral head by corticosteroid injections in osteonecrosis. We report these very rare findings along with literature reviews.
Keywords
Hip, Osteonecrosis, Corticosteroid.
Introduction
Rapid destructive coxarthrosis can be defined according to its clinical, anatomical, and pathological criteria [1]. The etiology is not well known. Several case reports have been published since the first report by Forestier in 1957 [2]. Degenerative changes generally begin in a mostly healthy joint and progress to rapid destruction within 6–12 months [1]. Lequesne et al. [3] defined rapid destructive coxarthrosis as a greater than 2-mm/ year rate of joint space narrowing or more than 50% of joint space loss within one year. Underlying diseases include rheumatoid arthritis [4]; ischemic necrosis is also a potential cause. Steroid injections have been identified as a triggering factor [3,5]. The authors observed hyperacute destruction of the femoral head after three separate corticosteroid injections within six weeks in a man with bilateral idiopathic osteonecrosis. We suggest a strong correlation between the steroid injections and the rapid destruction of the femoral head.
Case Report
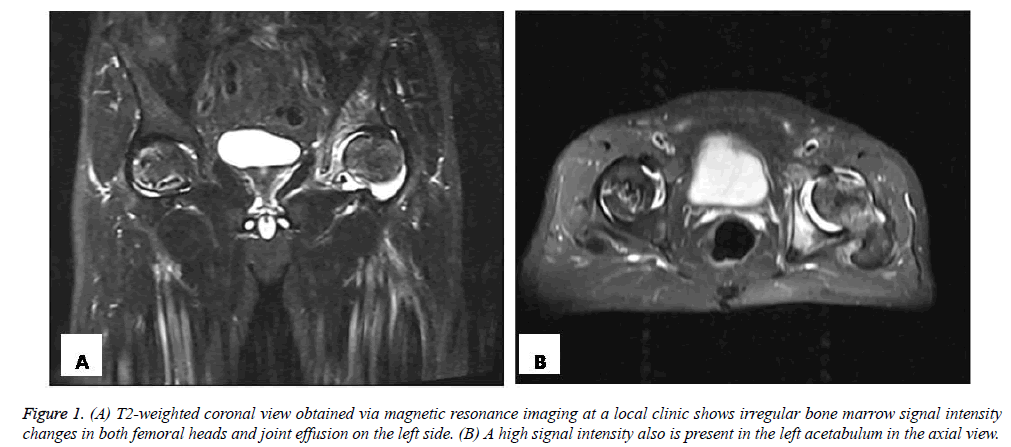
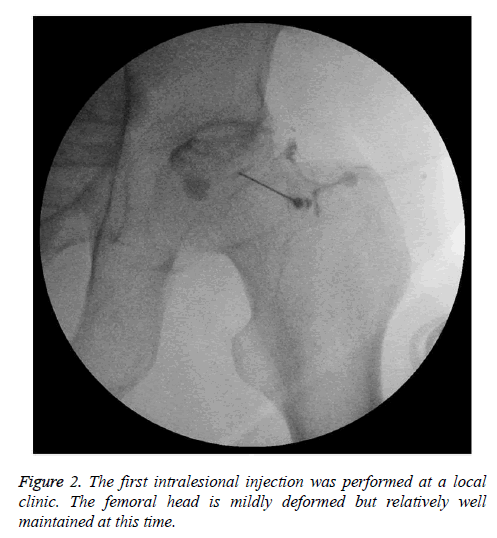
A 65-year-old male patient was checked using magnetic resonance imaging (MRI) at a private clinic for spontaneous pain in the left hip six weeks before being referred to our hospital. He had received treatment for early gastric cancer via a subtotal gastrectomy three years prior, and there was no history of corticosteroid intake or alcohol abuse. The change of bone marrow signal intensity was irregular in the first MRI (Figure 1), and the first intralesional injection was carried out in the left hip joint (Figure 2).
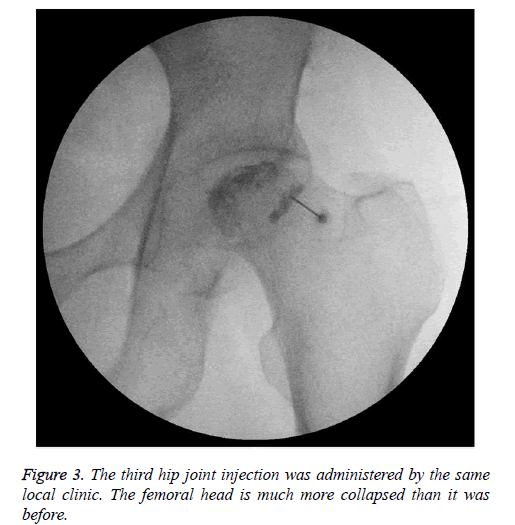
A limping gait and the left hip pain gradually worsened, and a steroid injection was administered once again 11 days later. However, the pain was still agonizing, so the third injection was done 7 days after the second one (Figure 3). The corticosteroid was a long-acting synthetic corticosteroid (Triamcinolone 20 cc) mixed with an anesthetic (Mepivacaine 2 cc). The pain was not controlled, and the patient was transferred to our hospital because the severe change in the femoral head was suspicious for acute infection or a metastatic lesion according to the local doctor, who was unfamiliar with rapid destructive coxarthropathy.
At our hospital, the patient’s body temperature was within the normal range. The passive range of motion of the left hip joint was also normal, and a Patrick test was positive. The Harris hip score was 43 points. A hematologic examination was conducted for the differential diagnosis of infection, rheumatologic disease, or metastasis in the hip joint. All the results were normal (ASO titer: 55.6 IU/ml, C-reactive protein: 7.7 mg/l, rheumatoid arthritis factor: <15 IU/ml) except for a slightly increased level of white blood cells (WBC: 10,010/μl). The tumor marker test did not show any abnormal findings.
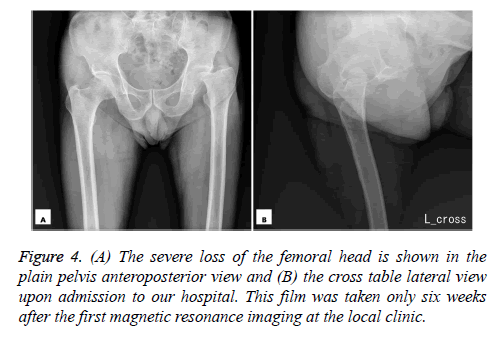
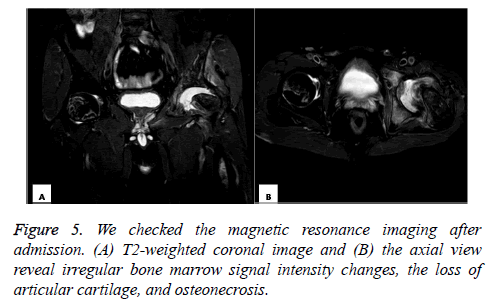
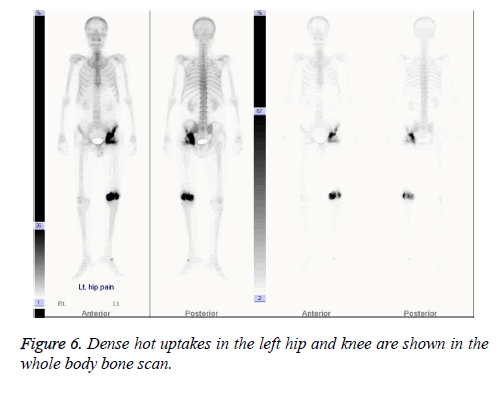
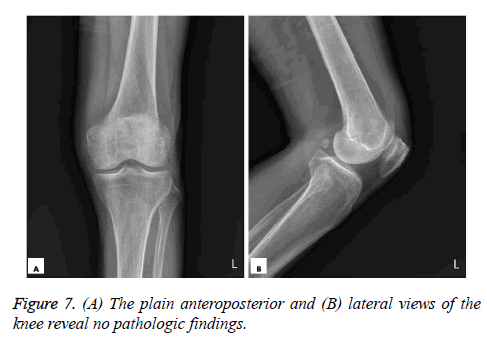
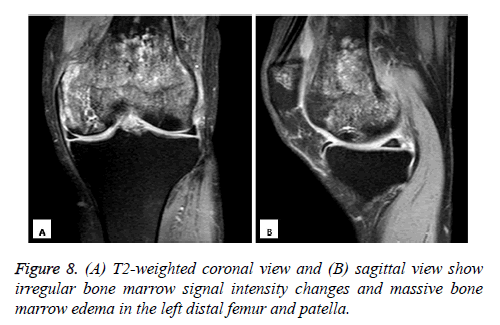
The patient was hospitalized, and a hip joint x-ray revealed destruction of the left femoral head, suggesting rapid destructive coxarthrosis (Figure 4). On hip joint MRI at our hospital, the change in the bone marrow signal intensity was irregular in the left femoral head, and a loss of articular cartilage and osteonecrosis were also observed (Figure 5). A whole-body bone scan of the patient showed dense hot uptakes only in the left hip joint and the distal femur (Figure 6). A knee joint x-ray was obtained to evaluate the hot uptake of the asymptomatic knee joint but revealed normal findings (Figure 7). Knee MRI showed an irregular and massive bone marrow signal intensity change that was consistent with massive bone infarct with bone marrow edema (Figure 8).
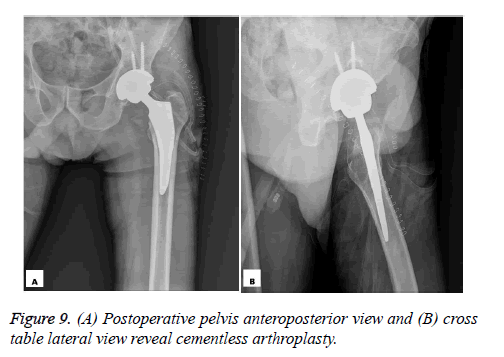
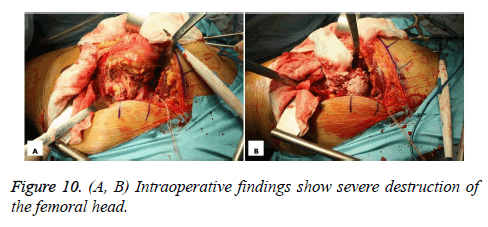
For a precise diagnosis, hip joint aspiration and bone biopsy of the proximal and distal femur was carried out under general anesthesia. The cytologic examination showed blood and necrotic materials (no cellular components), and the culture was negative. No evidence of malignancy or inflammation was found in the bone biopsy. The results of immunohistochemical staining for cytokeratin were negative. A cementless total hip arthroplasty was conducted on the left hip joint due to the patient’s severe symptom (Figure 9). The femoral head was significantly resorpted during the intraoperative evaluation (Figure 10). The postoperative histopathological findings revealed necrotic amorphous debris, fibrosis, blood clots in the marrow space, and fragmented bony trabeculae of both the hip and knee joint. These observations corresponded with osteonecrosis. After surgery, the patient was given a programmed rehabilitation schedule. We followed him up for 45 months in the outpatient department base, and the final Harris hip score was 92.
Discussion
Forestier described the first rapidly destructive arthrosis of the hip in 1957, and it was subsequently labeled atrophic osteoarthritis, rapidly progressive osteoarthritis, destructive osteoarthritis, and Postel’s osteoarthritis [2]. The causes of rapid joint destruction are still poorly defined, but etiologic factors include articular chondrocalcinosis, apatite crystal deposition, neuropathy, infection, drug-induced arthropathy, rheumatoid arthritis, and subchondral insufficiency fracture [5]. Rosenburg et al. argued that osteonecrosis associated with hematologic disorders, steroids, infections, and rheumatologic diseases should be excluded [6]. One of the clinical features that differentiate rapidly destructive arthropathy from other diseases is the progression rate of the arthropathy. Regarding the duration, Bock et al. reported acute destruction of the articular surface within an average of 14 months in 23 cases [7]. Most other studies have observed an occurrence of the destruction within an average of 12 months; severe cases showed destruction within 6 months. Our case was a very rare and hyperacute resorption where joint destruction was accelerated in just six weeks due to the underlying disease of osteonecrosis and following three sessions of prior steroid injections.
The etiology of acute bone destruction is related with osteonecrosis of the entire femoral head. Ischemic hip disease is a potential causative factor of rapidly destructive hip osteoarthritis [3,8,9]. Moreover, it occurs more often in patients with rheumatoid arthritis. High-risk groups amongst those with rheumatoid arthritis include postmenopausal women, drug resistant patients with highly active disease, and those taking steroids [4]. Yun et al. [10] reported rapidly destructive arthropathy of the hip joint in three elderly rheumatoid arthritis patients. Their patients also similarly met the aforementioned criteria: they had disorders in more than four major joints; steroid and disease-modifying antirheumatic drugs were administered for a prolonged period; and the patients’ body mass index was below 20 kg/m Yun et al. [10]. Yamamoto et al. [5] identified acute destruction of the femoral head after steroid injection in a healthy femoral head and suggested a cause-and-effect relationship between the steroid injection and acute destruction of the femoral head [5]. Caroline et al. reported no effect of intraarticular glucocorticoid injection for the treatment of rapid destructive hip osteoarthritis [5]. Caroline et al. [3] also found that the prior injection of a glucocorticoid did not decrease the need for total joint arthroplasty. Kawai et al. [1] reported satisfactory treatment results with the use of a Kerboull-type acetabular reinforcement device. Rapid destruction of the femoral head is usually common in patients with existing rheumatologic disease, female patients who take steroids, and those with secondary osteonecrosis, especially in steroid-induced cases.
In our case, the patient was a male who had no underlying diseases; the bilateral osteonecrosis was idiopathic, which indicates that this rapid destruction might be a very rare condition compared to previous reports. The corticosteroid injections’ role is still controversial in the rapid destruction of the femoral head. However, we suggest that these injections were a causative factor in the hyperacute destruction of the femoral head because the frequency of injection and the duration of destruction were too different compared to the usual cases. In addition, the possibility of destruction due to osteonecrosis that preceded the injections should be also considered. We can accept intralesional steroid injections in normal conditions, such as patients with simple osteoarthritis, but in osteonecrotic patients, we should consider this serious complication of rapid destructive coxarthropathy. A limitation of our case was that it was not clear whether the causative factor for the abrupt destruction of the femoral head was the steroids. We also have to consider that primary resorption of the femoral head is progressive, and the steroid injections may have only been coincidental.
Conclusion
We observed unilateral rapid resorption of the femoral head in a patient with bilateral idiopathic osteonecrosis. Three separate corticosteroid injections were strongly causative factors in the short period in which the destruction of the femoral head occurred. The osteonecrosis and the steroid injections were the probable etiology of the rapid destruction of the hip joint. Intralesional injection of steroid should be used with caution in patients with osteonecrosis.
No benefits in any form have been or will be received from a commercial party related directly or indirectly to the subject of this article.
References
- Kawai T, Tanaka C, Ikenaga M, Kanoe H, Okudaira S. Total hip arthroplasty using Kerboull-type acetabular reinforcement device for rapidly destructive coxarthrosis. Journal of Arthroplasty 2010; 25: 432-436.
- Batra S, Batra M, McMurtrie A, Sinha AK. Rapidly destructive osteoarthritis of the hip joint: A case series. Journal of Orthopedic Surgery and Research 2008; 3.
- Villoutreix C, Pham T, Tubach F, Dougados M, Ayral X. Intraarticular glucocorticoid injections in rapidly destructive hip osteoarthritis. Joint Bone Spine, 2006; 73: 66-71.
- Yoshino K, Momohara S, Ikari K, Kawamura K, Mochizuki T, Iwamoto T, Tomatsu T.. Acute destruction of the hip joints and rapid resorption of femoral head in patients with rheumatoid arthritis. Modern Rheumatology 2006; 16: 395-400.
- Yamamoto T, Schneider R, Iwamoto Y, Bullough PG. Rapid destruction of the femoral head after a single intraarticular injection of corticosteroid into the hip joint. Journal of Rheumatology, 2006; 33: 1701-1704.
- Khanna AJ, Domb BG, Moshirfar A, Wenz Sr JF. Rapidly destructive osteoarthropathy of the hip. American Journal of Orthopedics 2004; 33: 243-247.
- Bock GW, Garcia A, Weisman MH, Major PA, Lyttle D, Haghighi P, Resnick D. Rapidly destructive hip disease: Clinical and imaging abnormalities. Radiology 1993; 186: 461-466.
- Laroche M, Moineuse C, Durroux R, Mazières B, Puget J. Can ischemic hip disease cause rapidly destructive hip osteoarthritis? A case report. Joint Bone Spine 2002; 69: 76–80.
- Ryu KN, Kim EJ, Yoo MC, Park YK, Sartoris DJ, Resnick D. Ischemic necrosis of the entire femoral head and rapidly destructive hip disease: Potential causative relationship. Skeletal Radiology 1997; 26: 143-149.
- Yun HH, Song SY, Park SB, Lee JW. Rapidly destructive arthropathy of the hip joint in patients with rheumatoid arthritis. Orthopedics 2012; 35: e958-962.