ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 1
Epicardial fat thickness is an important diagnostic marker for newly diagnosed essential hypertension
1Department of Cardiology, Konya, Turkey
2Department of İnternal Medicine, Konya, Turkey
3Department of Biochemistry, Konya, Turkey
- *Corresponding Author:
- Hüseyin Katlandur
Department of Cardiology
School of Medicine
Mevlana University
Turkey
Accepted date: April 10, 2016
Previous studies showed the association between epicardial fat thickness (EFT) and cardiovascular risk. Current study was to investigate relationship between newly diagnosed essential hypertensive (NDEH) patients with the EFT and left ventricle wall thickness. A 49 newly diagnosed hypertensive patients and 36 healthy controls according to the American Hypertension Guidelines (Joint National Committee 8) were enrolled in the study. EFT and left ventricle wall thickness were measured using 2D echocardiography. The hypertensive patient’s echocardiographic values included EFT (0.61 ± 0.15 vs. 0.38 ± 0.14 p:0.001), left ventricle septal thickness (1.3 ± 0.6 vs. 1.1 ± 0.08 p<0.001), left ventricle posterior wall thickness (1.2 ± 0.13 vs. 1.1 ± 0.05 p<0.001) were greater than normotensive patients. EFT (OR 468, 95% CI 0, 535-1, 955; p=0,001) was an independent predictor of the new diagnosis of hypertension according to the multivariate regression analysis. In this study, we provide the threshold value of echocardiographic EFT for newly diagnosed hypertensive patients.
Keywords
Epicardial fat tissue, Echocardiography, Hypertension.
Introduction
EFT is one of visceral fat stores in the body, located between the visceral pericardium and the myocardium. It produces cytokines with a standard comparable to abdominal visceral adipose tissue [1]. EFT is a highly active organ that has protective and harmful effects on the myocardium [2]. Recent studies have shown relation between epicardial fat accumulation and development of atherosclerosis, coronary heart disease and hypertension [3,4]. EFT has been suggested as a new cardio metabolic risk factor [5]. Evaluation of amount of the EFT various techniques such as echocardiography, computed tomography and magnetic resonance imaging are available [1]. Especially echocardiographic measurement is inexpensive, easy accessible and rapid to use and it also advantageous because other cardiac parameters can be achieved simultaneously [6]. New diagnosis of essential hypertension remains a clinical problem. Some clinical definitions related to hypertension such as white coat hypertension, pseudo-normal pattern makes difficulty for the determination of real hypertensive patients and increases the costs. An economic imaging technique using the determination of real hypertensive patients is needed. Therefore, this study assessed the possible relationship between new diagnosis of hypertension and some echocardiographic parameters in the prospective analysis.
Materials and Methods
Total 85 participants enrolled to study including 49 newly diagnosed hypertension patients were admitted to outpatient cardiology clinic for various reasons and 36 were normotensive healthy individuals accepted as a control group. Blood pressure measurements were obtained from each patient (using both arms) in the seated position, using a standard mercury sphygmomanometer. Korotkoff-I accepted systolic blood pressure (SBP) and Korotkoff-V accepted diastolic blood pressure (DBP). The same investigator measured blood pressure at each visit, in the morning after the patient had rested for at least 10 minutes in a quiet room. Three successive blood pressure readings were obtained at 1-minute intervals, and the mean of the three readings was calculated. Diagnosis of HT was based on the criteria in the Eighth Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC-8) [7]. HT diagnoses confirmed and exclude white-coat HT, with the 24-h ambulatory BP performed using a portable digital recorder (Mobilograph, Stolberg, Germany). The BPs were recorded at 30-min intervals during night-time (from 10 p.m. to 6 a.m.) and at 15-min intervals during daytime (from 6 a.m. to 10 p.m.). Mean Daytime systolic/diastolic BP of 135/85 mmHg or greater, or a mean night-time BP of 120/70 mmHg or greater was accepted as hypertension. Subjects taking any medication for the treatment of hypertension, previously diagnosed as secondary hypertension, known coronary artery disease, renal artery disease, liver insufficiency, hypothyroidism, hyperthyroidism excluded from the study. The ethics board approved the study, and written informed consent was obtained from all study participants. The control group was formed from otherwise healthy individuals. Body mass index (BMI) was calculated, dividing weight by height squared (kg/m2). Following a 12 hours’ night time fast, venous blood samples were obtained from the antecubital vein to measure serum glucose, total cholesterol, high density lipoprotein, low density lipoprotein, triglycerides. Blood samples were placed in biochemistry and haematological tubes. Biochemistry samples were centrifuged for 5 min at 3500 rpm and the samples studied at the same time.
Echocardiographic evaluation
Subjects were studied in the left lateral position. 2.5-3.5 MHz transducers were used in all echocardiographic studies. Echocardiography measurements were taken according to the American Society of Echocardiography with using a Vivid 5 Pro (GE Vingmed Ultrasound, Horten Norway) [8]. Measurements taken from the left atrium, left ventricle, anterior wall, posterior wall, and left ventricle ejection fraction.
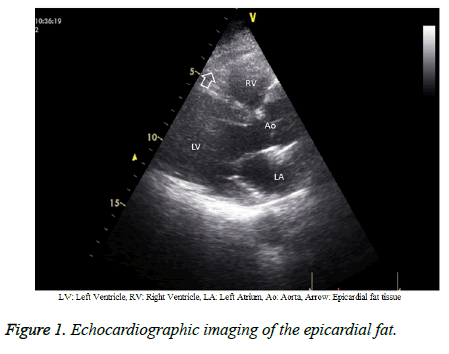
Epicardial adipose tissue thickness measurements
Parasternal long-axis and short axis views allows adequate assessment of EFT overlying the right ventricle (Figure 1). EFT is identified as the hypo echoic space anterior to the right ventricular wall and its thickness is measured between the epicardial surface and the parietal pericardium, seen between these two layers and is measured at the end-systole [6]. Two experienced cardiologist who unaware the patient’s clinical status was performed all patient’s transthoracic echocardiographic examinations. If measurements by the two investigators differed by >5% for any of the variables, the patient was not included; if the difference was <5%, the measurements were averaged.
Statistical analysis
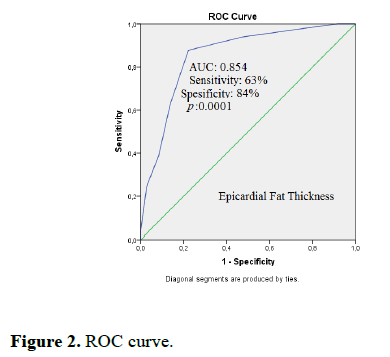
Data were analysed using the Statistical Package for the Social Sciences, ver. 22 for Windows (SPSS, Chicago, IL). The data are shown as the mean ± standard deviation for continuous variables, median (range) for ordinal variables, and frequency and percentage for categorical variables. A p-value of <0.05 was considered statistically significant. Continuous variables were analysed using unpaired t-tests and the Mann–Whitney U-test and dichotomous data using the Pearson’s χ2 test or Fisher’s exact test. Categorical variables were compared between groups by the χ2 test. Logistic regression analysis was used to identify independent predictors of NDEH. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated for independent parameters associated with hypertension. Receiver operator characteristic curve analysis was used to identify the optimal cut-off point of EFT diameter (i.e., the maximal sensitivity and specificity) for predicting new diagnosis hypertension.
Results
The study enrolled 49 patients admitted cardiology clinic due to various reason. The average patient age was 46.2 ± 11.2 (range 26-69) years; the average BMI was 29.7 ± 3 (range 23-37) kg/m2. The study population included 44 (51%) women. Baseline characteristics, laboratory and echocardiographic variables are summarized in Table 1. The patients with newly diagnosed hypertension had a significantly greater body mass index (30.5 ± 3.3 vs. 28.8 ± 2.4 kg/m2 p: 0.01) than those who remained in the norm tension. Demographic variables such as age, current smoking and laboratory variables such as fasting glucose, total cholesterol, HDL cholesterol, LDL cholesterol, triglycerides, haemoglobin, Blood Urine Nitrogen (BUN), creatinine were similar in both groups. The hypertensive patient’s echocardiographic values included EFT (0.61 ± 0.15 vs. 0.38 ± 0.14 p:0.001), left ventricle septal thickness (1.3 ± 0.6 vs. 1.1 ± 0.08 p:0.001), left ventricle posterior wall thickness (1.2 ± 0.13 vs. 1.1 ± 0.05 p: 0.001) were greater than normotensive patients. Receiver operator characteristic curve analysis revealed a cut off of 0.55 cm (95% Confidence Interval 0.768-0.940, area under the curve 0.854, p=0.0001) of the EFT for predicting newly diagnosis hypertension with 63% sensitivity and 84% specificity (Figure 2). A logistic regression analysis was performed on demographic, laboratory and echocardiographic variables. Only the EFT (Odds Ratio:0.468, 95% Confidence Interval 0.535-1.955; p=0.001) was an independent predictor of the diagnosis of hypertension. (Table 2).
| Variables | Hypertension | Normotension | p value |
| Baseline Characteristics | |||
| N | 49 | 36 | |
| Age (years) | 47.9 ± 11.6 | 43.9 ± 10.5 | 0.1 |
| Male/Female | 22/27 | 19/17 | 0.51 |
| Body Mass Index (kg/m2) | 30.5± 3.3 | 28.8 ± 2.4 | 0.01 |
| Current Smoker | 4 | 5 | 0.48 |
| Laboratory variables | |||
| Fasting glucose (mg/dl) | 106.2 ± 25.9 | 98.9 ± 11.7 | 0.12 |
| Total cholesterol (mg/dl) | 210.9 ± 41.6 | 200.2 ± 49.4 | 0.28 |
| HDL cholesterol (mg/dl) | 46.1 ± 10.9 | 46.8 ± 9.3 | 0.74 |
| LDL cholesterol (mg/dl) | 128.5 ± 35.1 | 121.5 ± 42.1 | 0.4 |
| Triglycerides (mg/dl) | 176.4 ± 95.3 | 143.6 ± 67.1 | 0.08 |
| Haemoglobin (g/l) | 14.1 ± 1.4 | 14.1 ± 1.6 | 0.94 |
| Blood Urine Nitrogen (BUN) (g/l) | 14.8 ± 6.4 | 14.7 ± 4.4 | 0.06 |
| Creatinine (mg/dl) | 0.75 ± 0.16 | 0.71 ± 0.15 | 0.28 |
| Echocardiographic Variables | |||
| Epicardial Fat Thickness (mm) | 0.61 ± 0.15 | 0.38 ± 0.14 | 0.001 |
| Left Ventricle Septal Thickness (cm) | 1.3 ± 0.6 | 1.1 ± 0.08 | 0.001 |
| Left Ventricle Posterior Wall Thickness (cm) | 1.2 ± 0.13 | 1.1 ± 0.05 | 0.001 |
| Bolded data are statistically significant | |||
Table 1: Baseline characteristics, laboratory and echocardiographic variables stratified by diagnosis of hypertension.
| Variables | OR | 95% CI | p value |
| Age | 0.093 | -0.005,0.014 | 0.397 |
| Body mass index | 0.116 | -0.013,0.050 | 0.238 |
| Fasting glucose (mg/dl) | -0.006 | -0.005, 0.005 | 0.952 |
| Total cholesterol (mg/dl) | -0.213 | -0.005, 0.000 | 0.097 |
| HDL cholesterol (mg/dl) | 0.006 | -0.009, 0.010 | 0.950 |
| LDL cholesterol (mg/dl) | 0.174 | -0.001, 0.005 | 0.151 |
| Triglycerides (mg/dl) | -0.063 | -0.002, 0.001 | 0.595 |
| Hemoglobin (g/l) | -0.072 | -0.090, 0.043 | 0.490 |
| Blood Urine Nitrogen (g/l) | -0.045 | -0.022, 0.014 | 0.670 |
| Creatinine (mg/dl) | -0.105 | -1.004, 0.353 | .342 |
| EFT (cm) | 0.468 | 0.535, 1.955 | 0.001 |
| Septum thickness (cm) | -0.048 | -1.36, 61.071 | 0.810 |
| Posterior wall thickness (cm) | 0.365 | -0.065, 2.800 | 0.061 |
| OR: Odds Ratio, CI: Confidence Interval, EFT: Epicardial fat thickness Bolded data are statistically significant |
|||
Table 2: Baseline, laboratory and echocardiographic variables examined in the univariate logistic regression analysis.
Discussion
In present study we demonstrated following results; first, there was an association between new diagnosis hypertension and echocardiographic parameters included EFT and left ventricular wall thickness. Second, EFT was an independent predictor of new diagnosis of hypertension. Finally, an EFT value >0.55 cm was an independent risk factor for new diagnosis of hypertension according to ROC curve analysis. Recent studies have shown that awareness rate of the hypertension in western countries are still low despite diagnostic and therapeutic advances [9]. Nowadays, development of the major public health problems due to uncontrolled hypertension threatened to the nations in terms of economic and psychosocial [10]. The patient with high blood pressure it is important that they are really hypertensive or not. In these patients who have an elevated blood pressure, the diagnosis of hypertension should be confirmed using out-ofoffice blood pressure measurement, ambulatory blood pressure monitoring or home blood pressure measurement. In patients with end organ damage secondary to hypertension it definitely supports the diagnosis of hypertension. Epicardial fat tissue is visceral fat deposit, located between pericardium and myocardium. It is not only simple fat deposit; it also shares many inflammatory and hormonal properties. Epicardial fat tissue and the myocardium do not have any fascia separates, thereby sharing the same microcirculation. Previous studies demonstrated that relation between EFT and metabolic syndrome, obesity, coronary artery disease, type-2 diabetes mellitus and hypertension [11-15]. Eroglu et al claimed that energy requirements of the myocardium increases due to hypertension with left ventricular hypertrophy. The increase in the epicardial adipose tissue via free fatty acids provide energy needs of the myocardium and epicardial adipose tissue growth the compensatory mechanism against left ventricular hypertrophy [15]. Similar to previous studies, we found that EFT correlates with systolic and diastolic BP [15,16]. In this present study, EFT over >0.55 cm predicts newly diagnosis hypertension with 63% sensitivity and 84% specificity. Eroglu et al. previously stated EFT over the 0.7 cm related the severity of hypertension [15]. In another study, Natale et al. reported positive correlation between EFT and duration of hypertension [17]. Main limitation of this study, patients with hypertension had a significantly higher body mass index. It is known that obesity component of the metabolic syndrome affects EFT and blood pressure. Another limitation of this study is that it has a relatively small number of patients.
Conclusion
As a result, EFT is not only related to the severity and duration of hypertension, but also it is an important diagnostic marker for newly diagnosed essential hypertension. We believe that these data may help for cardio-metabolic risk stratification through epicardial fat measurement for both clinical and research purposes.
References
- Bertaso AG, Bertol D, Duncan BB, Foppa M. Epicardial fat: definition, measurements and systematic review of main outcomes. Arq Bras Cardiol. 2013; 101: e18-28.
- Gastaldelli A, Basta G. Ectopic fat and cardiovascular disease: what is the link? Nutr Metab Cardiovasc Dis. 2010; 20: 481-490.
- Iacobellis G, Barbaro G. The double role of epicardial adipose tissue as pro- and anti-inflammatory organ. Horm Metab Res. 2008; 40: 442-445.
- Iacobellis G, Leonetti F. Epicardial adipose tissue and insulin resistance in obese subjects. J Clin Endocrinol Metab. 2005; 90: 6300-6302.
- Wu FZ, Wu CC, Kuo PL, Wu MT. Differential impacts of cardiac and abdominal ectopic fat deposits on cardio Metabolic risk stratification. BMC CardiovascDisord. 2016; 16: 20.
- Iacobellis G, Assael F, Ribaudo MC, Zappaterreno A, Alessi G, Di Mario U. Epicardial fat from echocardiography: a new method for visceral adipose tissue prediction. Obes Res. 2003; 11: 304-310.
- James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J. 2014 evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). Jama. 2014; 311: 507-520.
- Sahn DJ, DeMaria A, Kisslo J, Weyman A. Recommendations regarding quantitation in M-mode echocardiography: results of a survey of echocardiographic measurements. Circulation. 1978; 58: 1072-1083.
- Fernald FF, Van Den Born BJ, Snijder MB, Brewster LM, Peters RJ, Agyemang C. Hypertension awareness, treatment, and control among diabetic and nondiabetic individuals in a multi-ethnic population in the Netherlands: the HELIUS study. J Hypertens. 2016; 34: 539-547.
- Arredondo A, Cuadra SM, Duarte MB. Challenges of the epidemiological and economic burdens associated with hypertension in middle income countries: evidence from Mexico. BMC Public Health. 2015; 15: 1106.
- Rabkin SW. The relationship between epicardial fat and indices of obesity and the Metabolic syndrome: a systematic review and meta-analysis. Metab Syndr Relat Disord. 2014; 12: 31-42.
- Chun H, Suh E, Byun AR, Park HR, Shim KW. Epicardial fat thickness is associated to type 2 diabetes mellitus in Korean men: a cross-sectional study. CardiovascDiabetol. 2015; 14: 46.
- Faghihi S, Vasheghani-Farahani A, Parsaee M, Saedi S, Ghadrdoost B. Association Between Epicardial Fat Thickness and Premature Coronary Artery Disease: A Case Control Study. Res Cardiovasc Med. 2015; 4: e25679.
- Graeff DB, Foppa M, Pires JC, Vigo A, Schmidt MI, Lotufo PA, Mill JG, Duncan BB. Epicardial fat thickness: distribution and association with diabetes mellitus, hypertension and the Metabolic syndrome in the ELSA-Brasil study. Int J Cardiovasc Imaging. 2016; 32: 563-572.
- Eroglu S, Sade LE, Yildirir A, Demir O, Muderrisoglu H. Association of epicardial adipose tissue thickness by echocardiography and hypertension. Turk Kardiyol Dern Ars. 2013; 41: 115-122.
- Sengul C, Ozveren O, Duman D, Eroglu E, Oduncu V, Tanboga HI, Can MM, Akgun T, Dindar I. Echocardiographic epicardial fat thickness is related to altered blood pressure responses to exercise stress testing. Blood Press. 2011; 20: 303-308.
- Natale F, Tedesco MA, Mocerino R, de Simone V, Di Marco GM, Aronne L, Credendino M, Siniscalchi C, Calabrò P, Cotrufo M, Calabrò R. Visceral adiposity and arterial stiffness: echocardiographic epicardial fat thickness reflects, better than waist circumference, carotid arterial stiffness in a large population of hypertensives. Eur J Echocardiogr. 2009; 10: 549-555.