ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 4
Effectiveness of guided tooth brushing program for children with visual impairments-a randomized controlled trial
1Department of Community and Preventive Dentistry, Dow University of Health Sciences, Karachi, Pakistan
2Department of Haematology, Consultant, The Cancer Foundation, Karachi, Pakistan
- *Corresponding Author:
- Ambrina Qureshi
Department of Community and Preventive Dentistry
Dow University of Health Sciences, Pakistan
Accepted date: August 5, 2016
Aims: Apart from oral hygiene instructions continual motivation and manual dexterity may also be fundamentally required in case of disability. The objective of this study was to determine the effects of a guided manual tooth brushing program on oral hygiene status of visually impaired individuals after one month.
Methods: Parallel design single blind randomized controlled trial was conducted at Dr. Panjwani School Complex for the Blind, Karachi in collaboration with Ida Rieu Welfare Association. According to American Dental Association Guidelines 25 participants with visual impairments were required in each trial arm. Baseline data regarding oral hygiene practices and oral hygiene status using Oral Hygiene Index (OHI) was collected and participants were randomly assigned to test and control groups. Test group participants were intervened with guided tooth brushing program and controls with verbal oral hygiene message. Both were followed for 30 days. Data was managed using Stata version 11.0. Paired ttest was applied to compare between and within group mean differences in pre and post-trial oral hygiene index scores at p<0.05 with 95% confidence interval.
Results: Mean oral hygiene index score only within test group participants was reduced after 30 days trial with mean difference of -1.57 (95% CI, -2.087 to -1.071), t (24)=6.415, p<0.0001.
Conclusion: This study showed that guided manual brushing technique is effective in improving oral hygiene status of visually impaired individuals.
Keywords
Visual impairment, Effectiveness tooth brushing, Oral hygiene instruction
Abbreviations
ADA: American Dental Association; OHI: Oral Hygiene Index; CONSORT: Consolidated Standards of Reporting Trials; SNOSE: Sequentially Numbered, Opaque and Sealed Envelopes.
Introduction
Visually impaired children are solely reliant upon verbal instructions and simple information for their everyday routine abilities. One such routine task that they must fulfil is oral hygiene, which if jeopardized may have negative impact on their quality of life [1]. Very few studies have shown oral health problems occurring equally among visually impaired as well as those of their sighted peer [2,3]. This could be attributed to lack of dental knowledge and regular dental visits in general regardless of any disability [4]. On the other hand, there are noticeable studies which emphasize on much poorer oral health conditions of visually impaired children [5,6]; both in comparison to their sighted counter group [7] and peers with other disabilities [8]. Through these pertinent researches it is understandable that visual impairment must be causing some kind of obstacle in removing bacterial plaque from their tooth surfaces. Other difficulties may include toothpaste applications on brush and using brushing strokes that could be detrimental to oral structures. This may further cause damage to the periodontium and, as a consequence, may result in higher levels of gingival inflammation, calculus and debris than those who do not have any kind of major vision impairments. Therefore, in addition to verbal instructions, it is suggested that tactile aids may play a vital role in improving their potential and overcome their compromised abilities [4].
So far, the overall evidence retrieved on oral health of visually impaired has highlighted the need for raising pertinent knowledge and provision of oral health education to persons with visual impairment. It is understandable that these recommendations are based on the notion that knowledge of dental health is important to promote the maintenance of oral health [9]. However, very few researchers have promoted oral health without evaluating its effects [10,11] and further rare have recently studied the results of oral health promotion programs for disabled [12] and visually impaired individuals [13-15]. Thus there is a paucity of data and limited literature available on disseminating oral hygiene skills to individuals with visual impairments. In dentistry, key health promotion tool is oral hygiene instructions for prevention from poor oral conditions as it provides basis for good oral health throughout life. But in case of visually impaired children, apart from simple oral hygiene instructions for the prevention of poor oral conditions continual motivation and manual dexterity specifically for appropriate and adequate techniques may be fundamentally required [16]. Therefore, the objective of this study was to determine the effects of a guided manual tooth brushing intervention program on oral hygiene status of visually impaired individuals after one month.
Methods
A parallel design single blind randomized controlled trial was conducted at Ida Rieu Welfare Association, Dr. Panjwani School Complex for the Blind, Karachi over a span of four weeks (30 days). Ethical approval was taken by authors’ institution and pursued the ethical standards of World Medical Association for human experimentation 2008 version of Helsinki Declaration [17]. This study was in line with the CONSORT (Consolidated Standards of Reporting Trials) guidelines for reporting clinical trials [18] and sample size was acquired using the American Dental Association (ADA) Clinical Protocol Guidelines [19] and revealed that at least 25 participants were needed in each trial arm. Visually impaired and blind students who were registered and regularly attending the school were approached to be assessed for eligibility. Subjects with any other physical or mental disability and nonconsenting were excluded. A signed written and verbal consent informing about the aims and benefits of the study was taken from school administration/caregivers and each study participant respectively. Before dental examination all participants were interviewed using a structured questionnaire comprising of six questions regarding oral hygiene practices. Baseline oral hygiene status using Oral Hygiene Index of all participants was then examined by single trained and calibrated dental examiner (intra-examiner reliability=91%) who was blinded to the intervention allocation. Baseline dental examination was executed on a simple chair in day light with the help of sterilized dental examination instruments examining all buccal/ labial and lingual/palatal surfaces of all index teeth (16, 11, 21, 26, 36, 31, 41 and 46).
Participants were then randomly assigned to intervention (test and control) groups with equal division in both groups using simple random number table. Details of intervention to be administered to randomized participants were enclosed in Sequentially Numbered, Opaque and Sealed Envelopes (SNOSE). The randomization plan was determined by the principal investigator who was also the trial statistician.
The test group participants were intervened by 10 trained and calibrated dental students (mean kappa=95%) for BASS method of tooth brushing and applying full length amount of toothpaste via tactile stimuli first on demonstrative models in their hands and then their own teeth using manual tooth brushes provided to them. They were taught to count till 30 while brushing each quadrant using recommended technique. Their counting was sequenced with clock 30 seconds. They were also inculcated to brush twice daily, after breakfast in morning and before going to bed at night and were advised to rinse the oral cavity after every meal. Follow-up visit at their center was planned by dental students after two weeks of intervention where test group participants were advised to bring their tooth brushes and demonstrate tooth brushing. This was carried out to informally assess their performance.
Control group participants were intervened through verbal oral hygiene message to brush twice daily, after breakfast in morning and before going to bed at night and were advised to rinse the oral cavity after every meal. No particular skills to brush their teeth were taught to them.
Post-trial data was collected by dental examiners after 30 days and only OHI scores were examined and recorded of all study participants. Data entry and analysis was done using Stata version 11.0. Descriptive statistics was used to calculate frequency (in percentages) of baseline data and mean with standard deviation of OHI scores both before and after intervention were calculated. Chi-square test was applied to assess any difference between baseline responses and Paired ttest was applied to compare for both between group and within group difference in mean OHI scores at pre and post intervention levels. The p-value for statistically significant differences was considered as <0.05 at 95% confidence level.
Results
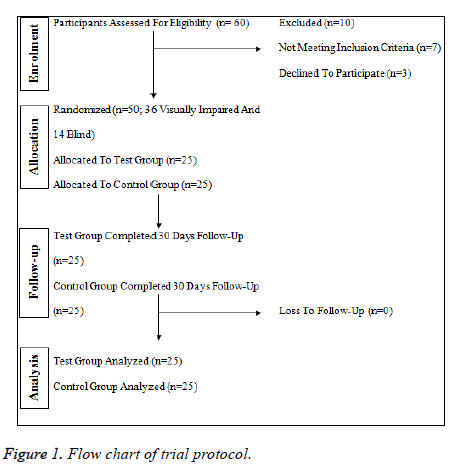
Sixty visually impaired and blind students were approached for this trial, of which 50 were finally recruited (n=25 in each group). Figure 1 presents the flow chart of trial protocol. Out of these 68% were males. Overall mean age was 12.42 ± 1.44 years with an age range of 10-15 years. With respect to participants’ visual condition 72% (n=36) of all were found with visual impairment and rest were completely blind. Overall mean OHI score was 3.06 ± 1.77. Group comparison with respect to age, gender and other baseline data is given in Table 1. All variables were matched among both groups (p>0.05).
| Baseline variables | Test group (n=25) | Control group (n=25) | p-value |
|---|---|---|---|
| Age (mean ± SD) | 12.35 ± 0.31 | 12.48 ± 0.27 | 0.755 |
| Gender | |||
| Male | 16 | 18 | 0.544 |
| Female | 9 | 7 | |
| Vision | |||
| Impaired | 16 | 20 | 0.208 |
| Blind | 9 | 5 | |
| What do you use for cleaning your teeth? | |||
| Brush and paste | 15 | 19 | 0.122 |
| Other (Only brush, Miswak, finger, powder) | 10 | 6 | |
| Who cleans your teeth? | |||
| Myself | 25 | 24 | 0.312 |
| Parent/Caretaker | 0 | 1 | |
| How often do you clean your teeth? | |||
| ≤ Once Daily | 19 | 16 | 0.735 |
| ≥ Twice Daily | 6 | 9 | |
| Mouth rinsing after every meal | |||
| Yes | 18 | 19 | 0.747 |
| No | 7 | 6 | |
| Mean OHI-score | 3.12 ± 1.40 | 3.00 ± 2.09 | 0.817 |
Table 1. Baseline comparison between test and control groups.
Table 2 presents between and within groups mean differences along with their statistical significances in OHI scores with reference to pre and post intervention. Mean OHI score within test group participants was reduced from 3.12 ± 1.40 to 1.54 ± 0.69 after 30 days of test trial with a statistically significant reduction of 1.57 (95% CI, -2.087 to -1.071) OHI score, t (24)=6.415, p<0.0001. Although after 30 days trial this reduction in mean OHI score was also observed among test group (1.54 ± 0.69) in comparison to the control group (2.35 ± 2.00) but this difference of -0.80 ± 2.10 (95% CI, -1.673 to 0.060) was not statistically significant (t (24)=-1.919, p=0.0669).
| Test group mean OHI | Control group mean OHI | Between groups mean difference | P-value (95% CI) | |
|---|---|---|---|---|
| Pre-intervention | 3.12 ± 1.40 | 3.00 ± 2.09 | 0.11 ± 2.52 | 0.817 (-0.924-1.160) |
| Post-intervention | 1.54 ± 0.69 | 2.35 ± 2.00 | -0.80 ± 2.10 | 0.066 (-1.167-0.060) |
| Within group mean difference | -1.57 ± 1.23 | -0.65 ± 2.15 | ||
| P-value (95% CI) | 0.000* (-2.087 to -1.071) | 0.141 (-1.543 to -0.233) | ||
| *Significance = p<0.05 | ||||
Table 2. Between and within group (test and control) differences in mean OHI score.
Discussion
Present study was planned to assess the effect of a guided tooth brushing intervention program on the oral hygiene status of visually impaired individuals and revealed a significant reduction in the mean OHI scores after one month of the intervened subjects. Sample size and trial conditions were appropriate according to using the ADA Guidelines, reasonable enough to evaluate short term results.
Considerable amount of oral debris and calculus was seen among visually impaired study participants at the baseline examination in this study. The reason could be an inability of these children to see and effectively utilize the oral hygiene aids. Test group participants showed a considerable positive change through this guided tooth brushing program leading to a substantial short-term improvement in their oral hygiene over a period of 30 days. However, further research is needed to assess long term effects. The result of this study is partially in line with other previous studies [13-15]. Previous studies observed plaque and gingival status unlike present study that considered OHI score as an outcome measure. Only one of these studies is found to be a randomized controlled trial and followed-up the participants for two months; [14] however, the sample size was not enough for the results to valid and reliable. Moreover, the statistical method used by the researchers for categorical data pertaining plaque (poor, fair, excellent) was analysed by using paired t-test is also unjustified leading to invalid and unreliable results.
Inter-group comparison in mean OHI scores was not found significant in our study. On the other hand previous study [15] found significant differences between gingival scores of “verbal+tactile group” and “verbal+tactile+braille group”, suggesting braille to be an effective tool to instil good oral hygiene practices for visually impaired individuals. However, study results must be cautiously considered due to non-random allocation of study participants.
It is admitted that present study did not consider the use of braille to teach the oral hygiene instructions to the visually impaired children due to lack of financial funding to initiate this trial which may be considered as a study limitation; but the study results will help pledge use of braille in future for this disadvantaged group of our society. Cautious inspection of the limits to services offered, the striking oral health negligence experienced by these disabled individuals can be effectively diminished. In addition it is also suggested that parents, caretakers and teachers must be trained with these methods to support tooth brushing so as to increase motivation and help sustain good oral hygiene among visually impaired.
Conclusion
Present study showed that guided manual brushing technique is effective in improving oral hygiene status of visually impaired individuals as compared to verbal oral hygiene message.
Acknowledgements
Special thanks to the management and teachers of Ida Rieu Welfare Association, Dr. Panjwani School Complex for the Blind.
Conflict of Interest
All authors declare that there is no conflict of interest.
References
- Tagelsir A, Khogli AE, Nurelhuda NM. Oral health of visually impaired schoolchildren in Khartoum State, Sudan. BMC Oral Health 2013; 13: 33.
- Azrina AN, Norzuliza G, Saub R. Oral hygiene practices among the visually impaired adolescents. Ann Dent Uni Malaya 2007; 14: 1-6.
- Herwis K, Ali A, Elturki H, Khamis H. Oral health status of visually impaired and sighted groups of children in Benghazi: A comparative study. Lib Dent J. 2013; 3: 1-5.
- Mahoney EK, Kumar N, Porter SR. Effect of visual impairment upon oral health care: a review. Br Dent J 2008; 204: 63-67.
- Bekiroglu N, Acar N, Kargul B. Caries experience and oral hygiene status of a group of visually impaired children in Istanbul, Turkey. Oral Health Prev Dent 2012; 10: 75-80.
- Ali S H, Hamad A M, Zardawi F M, Arif A N. Oral health knowledge, practice and oral hygiene status among visually impaired students in Sulaimani city, Iraq. J Dent Med Sc 2015; 14: 62-68.
- Solanki J, Gupta S, Chand S. Comparison of dental caries and oral hygiene status among blind school children and normal children, Jodhpur city Rajasthan, India. Univ Res J Dent 2014; 4: 22-25.
- Reddy VK, Chaurasia K, Bhambal A, Moon N, Reddy EK. A comparison of oral hygiene status and dental caries experience among institutionalized visually impaired and hearing impaired children of age between 7 and 17 years in central India. J Ind Soc Pedo Prev Dent 2013; 31: 141-145.
- Shih YH, Chang CHS. Knowledge of dental health and oral hygiene practices of Taiwanese visually impaired and sighted students. J Vis Impair Blind 2004; 98: 1-15.
- Nandini NS. New insights into improving the oral health of visually impaired children. J Indian Soc Pedod Prev Dent 2003; 21: 142-143.
- Dawn B. An observational study of oral hygiene care for visually impaired children. BDS Dental Elect Uni Glasgow 2008.
- Goyal S, Betsy ST, Bhat KM, Bhat GS. Manual tooth brushing reinforced with audio visual instruction versus powered tooth brushing among institutionalized mentally challenged subjects-A randomized cross-over clinical trial. Med Oral Pat Oral Y Ciru Bucal 2011; 16: e359-364.
- Apiwan S, Norawan R, Veeritta Y. A 6-month comparison of tooth brushing efficacy between the horizontal Scrub and modified Bass methods in visually impaired students. Int J Paed Dent 2011; 21: 278-283.
- Krishnakumar R, Silla SS, Durai SK, Govindarajan M, Ahamed SS, Mathivanan L. Comparative evaluation of audio and audio-tactile methods to improve oral hygiene status of visually impaired school children. Chrismed J Health Res 2016; 3: 55-59.
- Chowdary PB, Uloopi KS, Vinay C, Rao VV, Rayala C. Impact of verbal, Braille text, and tactile oral hygiene awareness instructions on oral health status of visually impaired children. J Indian Soc Pedod Prev Dent 2016; 34: 43-47.
- Bennadi D, Mythri H, Bharteesh JV. Dental negligence among visually impaired children-a call for attention. Res Rev J Dent Sc 2013; 1: 26-28.
- WMA Declaration of Helsinki-Ethical Principles of Medical Research Involving Human Subjects. W Med As 2016.
- Schulz KF, Altman DG, Moher D. Consort 2010 Statement: updated guidelines for reporting parallel group randomized trials. BMC Medicine 2010; 10: 18.
- Acceptance program guidelines. Am Dent As council sci affairs 2012: 1-10.