ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 22
Effect and mechanism of mirror therapy on rehabilitation of lower limb motor function in patients with stroke hemiplegia
Haiyan Wang1*, Zhijun Zhao2, Ping Jiang1, Xiaoli Li1, Qiaomao Lin1 and Qingwen Wu3
1Department of Rehabilitation, First Hospital of Qinhuangdao, Qinhuangdao, PR China
2Department of Radiology, Qinhuangdao Traditional Chinese Medicine Hospital of Hebei, Qinhuangdao, PR China
3Department of Nursing and Rehabilitation Medicine, Hebei United University, Tangshan, PR China
- *Corresponding Author:
- Haiyan Wang
Department of Rehabilitation
First Hospital of Qinhuangdao
PR China
Accepted date: November 29, 2017
Objective: To investigate the effects of mirror therapy on rehabilitation of lower limb motor functions in patients with stroke hemiplegia and explore its neurophysiological mechanism by investigating the change rule of BOLD-fMRI imaging during treatment.
Method: From September 1, 2013 to December 26, 2013, 36 stroke hemiplegia patients were randomly and evenly divided into mirror therapy group and general rehabilitation group, 18 cases in each group. All patients in both groups received routine rehabilitation treatment. The patients of the mirror therapy group were additionally given mirror therapy while the patients of the general rehabilitation group were trained to do the same movements as the mirror therapy group without visual feedback and motor imagery. Before and after treatment, the patients in each group were assessed by the Brainstorm stage of lower limb motor function, the Berg balance scale, the Functional Ambulation Category scale (FAC) and the transferring and walking parts of Functional Independent Measurement (FIM).
Results: There was statistically significant difference in Brainstorm score, the Berg balance scale score, FAC score and FIM score between both groups before and after treatment. The improvement of the mirror therapy group was more obvious than that of the general rehabilitation group. In terms of the BOLD-fMRI scan, before the treatment the two groups of 8 patients showed extensive and scattered activation of bilateral cerebral cortex with the absence of activation of M1 area. After the treatment those from the mirror therapy group mainly showed the M1 activation of the opposite side while the general rehabilitation group showed no obvious change. The volume of M1 activation and LI both increased after the treatment compared with the values before the treatment.
Conclusion: The application of mirror therapy, which is based on routine rehabilitation treatment, can improve lower limb motor functions for patients with stroke hemiplegia, realize more activation in the M1 area and promote the reorganization of the brain.
Keywords
Stroke, Hemiplegia, Lower limb function, Mirror therapy, BOLD-fMRI
Introduction
According to the statistics data from the National Health Department, more than 80% of the patients who survived the stroke had sequelae in which lower extremity dyskinesia was most commonly seen, seriously affecting the patient's capability of standing, walking and activities of daily living. Therefore, it is necessary to explore more and more effective methods to improve the motor function of the lower extremity for hemiplegic patients with strokes. In this regard, mirror therapy has been widely accepted by related scholars and rehabilitation workers both at home and abroad for its advantages such as wide range of application, low cost, simple operation and obvious therapeutic effect [1]. In 1990s, it was applied to the rehabilitation treatment of phantom limb pain after amputation by Professor Ramachandran. More than ten years later some scholars managed to apply it for the treatment of such diseases as complex regional pain syndrome [2-4], stroke [5], and peripheral nerve injury [6,7] with good therapeutic effects. However, most researches on stroke mirror therapy have focused on hemiplegic upper limbs but few of them have been done to study the rehabilitation of motor dysfunction of hemiplegic lower limb. This research, through evaluation of the relevant function scale, demonstrated the effects of mirror therapy on the patients’ lower limbs motor function, balance function, walking ability and activities of daily living, thus providing basis for mirror therapy to make a better combination with other rehabilitation means to improve the effect of the recovery treatment of lower extremity dysfunction. In addition, the application of BOLD-fMRI technology in the study of change in the cerebral cortex activation before and after treatment by mirror therapy displays the influence of mirror therapy on brain functional reorganization in patients with cerebral apoplexy, serving as a neurophysiological support for its development, and providing imaging data for exploration of its mechanism.
Materials and Methods
From September 1, 2013 to December 26, 2013, 36 cases of stroke patients with hemiplegia treated in Department of rehabilitation of Qinhuangdao First Hospital of Hebei Province were selected as the objects based on the above criteria of inclusion and exclusion. They were randomly divided into mirror treatment group and routine rehabilitation group with the type of stroke (cerebral hemorrhage, cerebral infarction) and duration (<4 w, 4-8 w) as hierarchical factors and the order of all experimenters’ entrance into the group was determined by way of random number table. Each group included 18 cases in which there were 26 males and 10 females at the age of 28 to 64. There was no significant difference in general data (gender, age, paralysis side) between the two groups (Table 1).
| Group | Case | Gender | Age (y) | Paralysis side | ||
|---|---|---|---|---|---|---|
| Male | Female | Left | Right | |||
| Mirror therapy group | 18 | 14 | 4 | 52.45 ± 2.91 | 10 | 8 |
| Routine rehabilitation group | 18 | 12 | 6 | 53.00 ± 2.79 | 9 | 9 |
Table 1: General data of mirror therapy group and routine rehabilitation group.
Inclusion criteria
The patients diagnosed, by brain CT or MRI with the standard consistent with the diagnostic criteria for stroke developed by WHO in 1989 [8], to suffer the first occurrence of unilateral cortical or subcortical function impairment blood-supplying region of middle cerebral artery. The patients with the duration of less than 2 months and with no rehabilitation therapy. The patients aged younger than 70. The patients with hemilateral dyskinesia at the Brunnstrom staging of I-IV in motor function of hemiplegic lower limb; the patients with the stable vital signs and a GCS score of 15. The patients with more than 48 h of aggravated nervous system symptoms without any progression. The patients with the education level of junior or above as well as a MMSE score of 24 and with no cognitive dysfunction. The patients with the function of the sitting balance ranking the 3rd level, the patients with normal result of KVIQ test. Voluntary patients ready to accept the risks of treatment with signed informed consent.
Exclusion criteria
Stroke patients complicated with severe affective disorders, sensory aphasia, mixed aphasia, apraxia, unilateral neglect, unilateral sensory impairment or serious limb spasm (improved Ashworth grading>grade 1). The patients with history of cerebral stroke, brain trauma, brain tumors or other nervous system diseases. The patients with a history of mental illness. The patients with serious dysfunction of important organs like heart, lung, liver and kidney; the patients with the history of malignancy. The patients with serious injury or disease in the lower extremity bone, joint or peripheral nerve. The patients with deep venous thrombus of lower extremity. The patients with the failure of visual impairment correction. The patients with MRI contraindication such as fear of metal implanted material and phobia.
Treatment methods
The patients of both two groups received conventional rehabilitation treatment, including the therapy of normal limb position put and lower limb-facilitation technique, training of balance function, gait and activities of daily living, training of play instruments like power bicycle and other physical factors treatment, 2-3 h/d, 5 d/w.
Mirror therapy group was treated with assisted mirror therapy, 40 min/d, 5 d/w. Patients were guided to take the long seat or sitting position in front of whom a mirror with a size of 45 × 70 cm was perpendicularly placed along median sagittal plane, The patient symmetrically placed both lower limbs on both sides of the mirror where the lower extremity of the uninjured side can reflect the side of the reflecting surface of the limb; the upper part of the body lightly inclined toward the healthy side to observe imaging of the lower limb of the uninjured side on the mirror surface and the affected lower limb, blocked by the mirror, failed to enter the field of vision; The patients were told to try to make lower limbs do the same action and complete the action with the help of therapist if necessary. We observed the imaging of the lower extremities of the uninjured side on the mirror and imagined it as the movement of the lower limb of the affected side. Type of task: keeping the body posture of the lower limb at rest for a training time of 5 min; taking simple movement of the lower extremity joints including 5 groups of actions, each action lasting 5 min, with Range of Motion (ROM) of joints as large as possible including flexion and extension of hip joint, internal and external rotation of hip, flexion and extension of knee joint, dorsiflexion as well as plantar flexion and circumduction of ankle joint. The composite motion of lower extremity joint contained two types of training with each lasting 5 min: S-shaped map or ring map.
The routine rehabilitation group additionally included the passive or active supplementary training of the lower extremities of the affected side with the same training as the mirror therapy with the avoidance of visual feedback or motor imagery of the lower limbs in this course, 40 min/d, 5 d/w.
Function scale score
Patients in the two groups were evaluated before treatment and 6 w after treatment through function scale score by the same rehabilitation specialist who didn’t participate in the treatment. The score items included Brunnstrom staging of motor function of lower extremity, Berg balance scale, and Functional Ambulation Category (FAC) and transporting as well as walking part of Functional Independence Measure (FIM).
Functional magnetic resonance imaging
Eight patients were selected in accordance with the random number table followed by the performance of BOLD-fMRI scan before treatment and 6 w after treatment. The similarities and differences in the scan results of the two groups were compared and activation volume of the opposite M1 area as well as LI value of the 8 patients in mirror therapy group before and after treatment were respectively calculated as follows.
Inspection procedure
The inspection process and the matters needing attention were introduced to the patients before the examination followed by action demonstration and training. The patient lay flat on the scanning bed, shoulders close to coil, head centered, lower jaw adduction. The foam earplug was inserted into the patient's ears to reduce the effects of noise. Foam pads were used to secure the head to minimize motion artifacts produced by the head movement. The patients were told to have their eyes closed, take relaxing and calm breathing, stop any active thinking and maintain the head and the body still. On hearing the auditory tone cues set up by the machine, an inspector completed a passive ankle dorsiflexion with a motion frequency of 1 Hz in accordance with the countdown device and each ankle joint went back to the plantar flexion position of 45º every moment it reached dorsiflexion position of 20º. The above operation was finished by the same inspector.
Statistical analysis
The measurement data were expressed by mean ± standard deviation and the counting data was tested with Chi-square test. The comparison of value before and after treatment within each group and the comparison of the value before treatment as well as the difference value compared with that after treatment between the two groups were analysed respectively with independent-samples T-test and paired-samples T-test on SPSS 17.0 for statistical analysis. P<0.05 suggests that the difference is statistically significant.
Results
Comparison of score results of each functional scale between mirror therapy group and routine rehabilitation group
Before treatment there was no significant difference in Brunnstrom staging of lower extremity motor function, Berg balance scale, FAC and transporting and walking part of FIM between the two groups. Compared with the values before treatment, the score results of each function scale were significantly improved in both two groups after treatment with those in the mirror therapy group much more obvious than those in the routine rehabilitation group (Tables 2-4).
| Group | Before treatment | After treatment | t | P |
|---|---|---|---|---|
| Mirror therapy group | 2.50 ± 1.10 | 4.44 ± 1.34 | 4.17 | 0.002 |
| Routine rehabilitation group | 2.61 ± 1.14 | 3.67 ± 1.28 |
Table 2: Comparison of Brunnstrom staging score and difference between two groups.
| Group | Before treatment | After treatment | t | P |
|---|---|---|---|---|
| Mirror therapy group | 1.28 ± 0.96 | 2.56 ± 0.62 | 2.61 | 0.013 |
| Routine rehabilitation group | 1.39 ± 1.04 | 2.00 ± 0.84 |
Table 3: Comparison of FAC score and difference between two groups before and after treatment.
| Index | Before treatment | After treatment | t | P |
|---|---|---|---|---|
| Activation volume | 58.19 ± 41.23 | 728.23 ± 258.53 | -10.86 | <0.0001 |
| LI value | 0.24 ± 0.31 | 0.51 ± 0.27 | -2.79 | 0.008 |
Table 4: Comparison of FIM score and difference between two groups before and after treatment.
The similarities and differences of BOLD-fMRI scan results between the mirror therapy group and the routine rehabilitation group
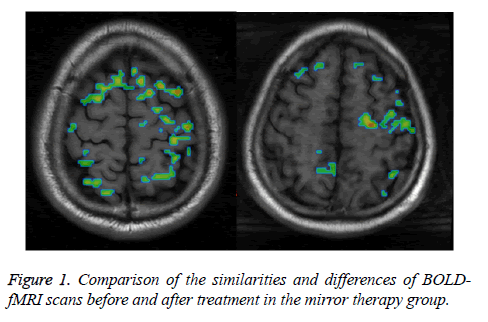
The result of BOLD-fMRI scan before treatment showed extensive and scattered activation of the bilateral cerebral cortex in both two groups of 8 patients with the absence of the activation in M1 area (Figure 1, left). After treatment, the BOLD-fMRI scanning showed dominated activation in contralateral M1 area in the case of passive ankle dorsiflexion at affected side in the mirror therapy group (Figure 1, right) and no obvious change of cortical activation compared with the result of previous scan in the routine rehabilitation group.
Comparison of activation volume of the opposite M1 area and LI value before and after treatment of 8 patients from mirror therapy group
In the mirror therapy group, the activation volume of the opposite M1 area and LI value of the 8 patients both significantly increased (Table 5).
| Index | Before treatment | After treatment | t | P |
|---|---|---|---|---|
| Activation volume | 58.19 ± 41.23 | 728.23 ± 258.53 | -10.86 | <0.0001 |
| LI value | 0.24 ± 0.31 | 0.51 ± 0.27 | -2.79 | 0.008 |
Table 5: Comparison of activation volume in M1 area and LI value before and after treatment in mirror therapy group.
Discussion
The mirror therapy was used for the treatment of stroke firstly in 1999, Altschuler [5] published in the lancet an article which showed that mirror therapy can increase the stroke joint activity and enhance the speed and accuracy of the action taken by the patients through its treatment 9 stroke patients, confirming positive effects of mirror therapy on motor function rehabilitation of the hemiplegic patients with stroke and giving rising to the necessity for further experiment and study of mirror therapy in treatment of stroke rehabilitation. In the following ten years, many scholars at home and abroad have made researches on it, making the rehabilitation of hemiplegia after stroke become one of the focuses of mirror therapy [9]. Earlier studies focused more on the study of hemiplegic upper limb rehabilitation with few researches done to improve post-stroke lower extremity dysfunction in mirror therapy. In 2007, Sutbeyaz [10] applied mirror therapy to rehabilitation of lower extremity motor function in hemiplegics after stroke for the first time through a randomized controlled trial and the results showed that the experimental group achieved more significant improvement in motor function, walking ability and activities of daily living compared with the control group.
Mirror therapy was performed by using a device called mirror box in early with a variety of designs carried out later according to different needs of the study in which the most simplified form turns out to perpendicularly put a mirror in front of the patient along the median sagittal plane. The mirror size is required to allow seeing all the movements of the uninjured side reflected in the mirror with the failure of seeing the affected side. In this study, we, based on the target body and task type, selected the mirror size of 45 cm × 70 cm, which can meet the requirement of both stowing on end in the training of sitting position and lying across in the training of long seat position.
Good preparation before can improve the effectiveness of training. Since mirror therapy is an active training of rehabilitation, thus the positive cooperation with patients becomes the key to successful training. Before the training, the therapist should explain in detail the essentials of treatment, treatment principle and the problems requiring attention. Particularly, the patient ought to be told to actively engage in visual participation and motor imagination, the most important part for the treatment, rather than the focus on how to complete the actual action of lower limb on the affected side. It is reasonable to figuratively tell patients that it is the brain that is involved in the training, not the body.
Because the results of current researches at home and abroad fail to make detailed description about specific actions during the treatment, we in this study designed specific types of action task targeting at the experimental population of hemiplegia patients with lower extremity motor dysfunction. The design conforms to the training principle of mirror therapy that the movement is trained from the easier to the more advanced and from proximal to distal extremities with the range ranging from 1 to 3 dimensions.
The evaluation results of function scale in this research showed that the combination with mirror therapy, compared with traditional rehabilitation therapy, enables to improve recovery of lower extremity motor function for the hemiplegic patients with stroke more effectively followed by the improvement in balance function, quality and speed of completion of actions like transporting, walking and other activities of daily living which are mainly dependent on the lower extremity. This research result provides a basis for the development of mirror therapy so that we can better combine it with other methods in future clinical work to improve the effect of comprehensive rehabilitation.
In this study, the neurophysiological mechanism of mirror therapy can be explored by analyzing the changes of cortical activation shown in the result of BOLD-fMRI scan before and after treatment. At present, neurophysiological mechanism of mirror therapy remains to be defined with such main ideas as: lower learned non-use: traditional theory holds that the stroke results from irreversible nervous centralis injury, however, some current researches have pointed out the possibility of reversible dysfunction in the case of nerve damage [11]. The reduction of body movement and loss of proprioceptive sensation in affected limbs lead to equilibrium shifting of brain function and regional reorganization, contributing to learned non-use. However, a large number of neurological and psychological researches show that the mirror therapy improves the consciousness of the affected limbs by providing appropriate visual input, which helps the recovery of the proprioception, reactivates the waste area and makes backmigration of brain function balance to produce functional reorganization of usage-dependency of brain structure and reduce the learned non-use followed by the recovery of motor function [5,12,13]. Mirror neurons mechanism: mirror neurons belong to a kind of special neuron of visual properties present in such sites of cerebral cortex as parallel fissure, inferior parietal lobule, inferior frontal gyrus, posterior parietal area, superior temporal regions and middle of the insula. The neuronal excitation would occur both when a mirror neuron individual performs a specific action and when an individual makes observation or imagines the same or similar actions [14]. All mirror neurons distributed in different brain regions form the mirror neuron system in which the mechanism of observation-execution enables to realize the unity and oneness between perception and execution of an action [15] and plays a key role in motor understanding, imitation, imagination and learning [16-19] exactly on which the mirror therapy is theoretically based [12,13,20-22]. Mirror therapy promotes brain plasticity and functional reorganization through the activation of the mirror neuron system and further improves the motor function [23]. Psychoneuromuscular (PM) theory: the central nervous system stores a pattern of motion patterns that act as a motor program; Despite the presence of physical disability, the "motor pattern" still remains intact or partially present in the stroke patients, having this pattern of motion originally used in practical activities equally strengthened and refined in the motor imagery of the hemiplegic limb [11], in other words, the visual imagination training of the mirror therapy would repeatedly strengthen the normal movement pattern from brain to muscle groups the same way as the case of actual activities so as to stimulate related muscles, improve movement control and coordination, enhance motor skills and speed up the process of motor learning; The "visual feedback mechanism: good motor visual stimulation provided by mirror therapy accelerates neural recruitment and function reorganization in cortex premotor area, primary motor cortex and sensorimotor cortex, which helps to establish the link between visual input and movement [24] and then facilitates the recovery of motor function [25]. In this study, the result of BOLD-fMRI scan before treatment showed extensive and scattered activation of the bilateral cerebral cortex in both two groups of 8 patients with the absence of the activation in M1 area. While after treatment, the BOLD-fMRI scanning showed dominated activation in contralateral M1 area in the case of passive ankle dorsiflexion at affected side in the mirror therapy group but with no obvious change of cortical activation compared with the result of previous scan in the routine rehabilitation group. The activation volume in contralateral M1 area and LI value turned out to obviously increase after treatment in the mirror therapy group of statistical significance. These results suggest that 6 w after treatment with mirror therapy, more active activation is possible in the contralateral M1 area of the affected limb, which normally occurs only during the exercise of the affected side. In the course of mirror therapy, through the visual illusion of seeing the injured limb moving but actually not moving, the motion information is constantly input from the nerve conduction pathway on the damaged side and through cortical response to sensorimotor input, it promotes cortical reorganization so as to induce voluntary movement in which the process allows to not only play the role of visual feedback mechanism, also increase proprioception by visual input and reduce the learned nonuse. Through the research we can also find that in the implementation of mirror therapy the excitability of the area in which mirror neurons are located (ventral region of the contralateral hemisphere SMA, premotor cortex, insula and hemisphere of premotor cortex, supramarginal gyrus and superior temporal gyrus) is on the rise. We can believe that the action of observation and imagination in the mirror therapy activates the mirror neuron system, which links some of the visual motor circuits in the brain, promotes brain reorganization and plays an important part in the development of motor learning, proving mirror neurons mechanism also plays a positive role during the treatment. So, the therapeutic effect of mirror therapy may be produced by the interaction of several mechanisms, which turns out to be consistent with the theory of brain plasticity-the basis of rehabilitation therapy. Although the routine rehabilitation group was given passive or active assisted training of the same movement with the mirror therapy group and in a certain extent inhibits the abnormal mode, the lack of key processes like visual input and motor imagery makes it fail to reach significant improvement of motor function and brain reorganization. In addition, with the participation in the active imagination training, the mirror therapy is more in line with the exciting conduction mode from the brain to the body compared with simple passive limb movement and facilitates the restoration of normal motor conduction pathway.
References
- Page SJ, Levine P, Leonard A. Mental practice in chronic stroke: results of a randomized, placebo-controlled trial. Stroke 2007; 38: 1293-1297.
- Sato K, Fukumori S, Matsusaki T. Non-immersive virtual reality mirror visual feedback therapy and its application for the treatment of complex regional pain syndrome: an open-label pilot study. Pain Med 2010; 11: 622-629.
- McCabe CS, Haigh RC. A controlled pilot study of the utility of mirror visual feedback in the treatment of complex regional pain syndrome. Rheumatology 2003; 42: 97-101.
- Moseley GL. Graded motor imagery is effective for long-standing complex regional pain syndrome: a randomised controlled trial. Pain 2004; 108: 192-198.
- Altschuler EL, Wisdom SB, Stone L, Foster C, Galasko D, Llewellyn DM, Ramachandran VS. Rehabilitation of hemiparesis after stroke with a mirror. Lancet 1999; 353: 2035-2036.
- Selles RW, Schreuders TA, Stare HJ. Mirror therapy in patients with causalgia (complex regional pain syndrome type II) following peripheral nerve injury: two cases. J Rehabil Med 2008; 40: 312-314.
- Rosen B, Lundborg G. Training with a mirror in rehabilitation of the hand. Scand J Plast Reconstr Surg Hand Surg 2005; 39: 104-108.
- WHO. Recommendations on stroke prevention, diagnosis and therapy. Report of the WHO task force on stroke and other cerebrovascular disorders. Stroke 1989; 20: 1407-1431.
- Cramer SC, Nelles G, Benson RR, Kaplan JD, Parker RA, Kwong KK, Kennedy DN, Finklestein SP, Rosen BR. A functional MRI study of subjects recovered from hemiparetic stroke. Stroke 1997; 28: 2518-2527.
- Sutbeyaz S, Yavuzer G, Sezer N. Mirror therapy enhances lower-extremity motor recovery and motor functioning after stroke:a randomized controlled trial. Arch Phys Med Rehabil 2007; 88: 555-559.
- Page SJ, Levine P, Sisto SA. A randomized efficacy and feasibility study of imagery in acute stroke. Clin Rehabil 2001; 15: 233-240.
- Ramachandran VS, Altschuler EL. The use of visual feedback, in particular mirror visual feedback, in restoring brain function. Brain 2009; 132: 1693-1710.
- Michielsen ME, Smits M, Ribbers GM. The neuronal correlates of mirror therapy:An fmri study on mirror induced visual illusions in patients with stroke. J Neurol Neurosurg Psychiatry 2009; 82: 393-398.
- Rizzolatti G, Craighero L. The mirror-neuron system. Annu Rev Neurosci 2004; 27: 169-192.
- Rizzolatti G, Fabbri-Destro M, Cattaneo L. Mirror neurons and their clinical relevance. Nat Clin Pract Neurol 2009; 5: 24-34.
- Kalra L, Ratan R. Recent advances in stroke rehabilitation 2006. Stroke 2007; 38: 235-237.
- Garrison KA, Winstein CJ, Aziz-Zadeh L. The mirror neuron system:a neural substrate for methods in stroke rehabilitation. Neurorehabil Neural Repair 2010; 24: 404-412.
- Small SL, Buccino G, Solodkin A. The mirror neuron system and treatment of stroke. Develop Psychobiol 2010; 1-10.
- Iacoboni M, Mazziotta JC. Mirror neuron system: basic findings and clinical applications. Ann Neurol 2007; 62: 213-218.
- Matthys K, Smits M, Van der Geest JN. Mirror-induced visual illusion of hand movements: A functional magnetic resonance imaging study. Arch Phys Med Rehabil 2009; 90: 675-681.
- Funase K, Tabira T, Higashi T. Increased corticospinal excitability during direct observation of self-movement and indirect observation with a mirror box. Neurosci Lett 2007; 419: 108-112.
- Yavuzer G, Selles R, Sezer N. Mirror therapy improves hand function in subacute stroke: a randomized controlled trial. Arch Phys Med Rehabil 2008; 89: 393-398.
- Cui Y, Cong F. Basic theory of mirror neuron system and its meanings in motor rehabilitation. J Rehab Theor Pract 2012; 18: 239-243.
- di Pellegrino G, Fadiga L, Fogassi L, Gallese V, Rizzolatti G. Understanding motor events: a neurophysiological study. Exp Brain Res 1992; 91: 176-180.
- Seitz RJ, Hoflich P, Binkofski F, Tellmann L, Herzog H, Freund HJ. Role of the premotor cortex in recovery from middle cerebral artery infarction. Arch Neurol 1998; 55: 1081-1088.