ISSN: 0970-938X (Print) | 0976-1683 (Electronic)
Biomedical Research
An International Journal of Medical Sciences
Research Article - Biomedical Research (2017) Volume 28, Issue 6
Comparison of the curative effects of PFNA and DHS fixation in treating intertrochanteric fractures in elderly patients
Department of Orthopaedics, Bayi Hospital Affiliated Nanjing University of Chinese Medicine, Nanjing, PR China
- *Corresponding Author:
- Jianmin Chen
Department of Orthopaedics
Bayi Hospital Affiliated Nanjing University of Chinese Medicine
Nanjing 210000, PR China
Accepted date: November 09, 2016
The aim of this study is to compare the effects of proximal femoral nail antirotation (PFNA) and dynamic hip screw (DHS) in the treatment of intertrochanteric fractures in order to investigate the significance of internal fixation in the treatment of intertrochanteric fractures in the elderly. One hundred and eight patients admitted with intertrochanteric fractures and treated with PFNA and DHS were retrospectively analyzed. Among the 108 patients, 46 patients were treated with PFNA therapy alone and 62 patients were treated by DHS. The operation time, blood loss, postoperative weight, fracture healing time, incidence of postoperative complications, hip activity, and walking activity were compared, in order to analyze the advantages and disadvantages of the two internal fixation methods. In total, 108 patients were followed up for 9-18 months. There were statistically significant differences in the average operative time, blood loss, fracture healing time, incidence of postoperative complications, and hip function between the two groups (P<0.05); specifically, the outcomes in the PFNA group were better than that in the DHS group. The PFNA method for treating elderly patients with intertrochanteric fractures has the advantages of reasonable design, minimal invasiveness, and reliable fixation, and is an ideal operation method for treating intertrochanteric fractures in elderly patients.
Keywords
Proximal femoral nail antirotation, Dynamic hip screw, Intertrochanteric fracture, Elderly.
Introduction
Intertrochanteric fractures are very common in elderly patients, making up about 60-70% of hip fractures. There is an approximately 15%-20% mortality rate in elderly patients within a year of having this type of fracture [1]. Considering the life expectancy and increase of social activities among the elderly, as well as the prevalence of osteoporosis, the incidence rate of this fracture is gradually increasing [2,3]. Presently, intertrochanteric fractures are treated by surgery and internal fixation, which is approved by orthopedists; however, poor bone quality and neck screw instability can adversely affect the results using the currently available fixation devices [4]. The dynamic hip screw (DHS) in adults may be a better option [5], and because of the various kinds of implants, the selection of implant for intertrochanteric fractures remains controversial [6]. Currently, the two main types of implants are proximal femoral nail antirotation (PFNA) and DHS. Some studies showed that PFNA offers better recovery and functional outcomes than DHS [7], but both techniques possess the same risk of postoperative complications [8]. A meta-analysis showed that, for pertrochanteric fractures, PFNA involves less blood loss and fewer complications compared with DHS [9]. Another meta-analysis found that although PFNA was associated with less blood loss and a lower rate of fixation failure, PFNA led to more fluoroscopy time [10]. One prospective randomized study included elderly patients with unstable pertrochanteric fractures and compared the outcomes between PFNA and DHS; it found that PFNA allowed earlier mobilization and faster recovery than DHS [11]. Our study was a prospective study, and we chose the fixation according to the patient’s condition.
Data and Methods
This study was conducted in accordance with the declaration of Helsinki, and conducted with approval from the Ethics Committee of Jingdu Hospital. Written informed consent was obtained from all participants.
The inclusion criteria were: age of 60-92 years, good cognitive function. DHS or PFNA fixation device obtained from Shandong Weigao Orthopedic Device Company Limited, China. Fractures caused by falls when standing and were considered relatively low energy injuries, the operation performed on average 4 days (range, 1-10 days) after patients’ admission. Exclusion criteria were: pathological fractures or the presence of metastatic disease, poly-trauma, severe osteoarthritis, chemotherapy, fractures caused by crushing or car accidents, unable to work before injury, ipsilateral lowerlimb surgery, and/or contralateral hip fracture.
Pre-operative preparation
Tibial tuberosity to skin traction was performed in each patient’s injured leg, and x-ray films were obtained of the bilateral femurs in the anteroposterior and lateral positions. We then measured the collodiaphyseal angle and the thickness of the femur marrow cavity to prepare suitable DHS armor plates and PFNA nails. Low molecular weight heparin (0.2 mg/kg of patient weight) was administered and stopped 24 h before surgery; patients who developed other complications were given systemic therapy. The patients were evaluated for their ability to tolerate surgery and postoperative recovery.
Surgical process
In the PFNA group, patients underwent lumbar plexus-sciatic nerve blocking anesthesia, and antibiotics were administered half an hour before surgery to prevent infection. Then, patients were laid on a traction table and the injured limbs adducted about 15 degrees. Next, longitudinal traction reduction was applied to the limb under C-arm fluoroscopy. A 5 cm incision was cut on the great trochanter of the femur and a guide pin was inserted into the top point of the femur. When the pin was confirmed to be in the marrow cavity, a hollow drill was used to expand the hole; we then chose a proper size for the main nail for PFNA, inserted it into the marrow cavity, and removed the guide pin. The depth and the front inclination angle of the main nail were carefully regulated; then the screw guide pin was implanted. The C-arm confirmed the good position of the guide pin and was used to measure the length of the screw blade in order to choose a responding screw blade. Based on the fracture and sclerotin condition, static force or dynamic force was used. After confirming good fixation of PFNA by Carm, a tail cap was installed, the operative area was washed to stop bleeding, a drainage tube was placed, and the wound was sutured until closed.
In the DHS group, patients underwent lumbar plexus-sciatic nerve blocking anesthesia, and antibiotics were administered half an hour before surgery. Patients were laid on a traction table and the injured limbs adducted about 15 degrees; next, traction reduction was applied to the injured limb under C-arm fluoroscopy. A femoral lateral longitudinal incision was cut at 2-3 cm under the greater trochanter of the femur; then, gap separation was performed to expose an approximately 8 cm femur section. Next, a guide pin was inserted 2 cm from the subtrochanteric section. The collodiaphyseal angle was kept at 135 degrees and the front inclination angle at 15 degrees. The C-arm confirmed good position and was used to measure the length of the cervical part of the femur. A hole was drilled and tapped, and a guide pin was drawn to insert the proper longitudinal thick screw to keep the screw tail level with the outside of the femur. An adequate longitudinal armor plate was chosen and applied with screw fixation at the external position of haft of the femur. For unstable fractures, another screw was added in the trochanteric region, followed by installation of a screw cap, washing of the operative area to stop bleeding, placement of a drainage tube, and suturing until the wound was closed.
Postoperative treatment
Antibiotics were used for 2 or 3 days for all patients after surgery, and anti-osteoporosis therapy (combinate calcium and an agent that promoted calcium absorption were orally weekly) was initiated 3 days after surgery. Pneumatic pumps were used and low molecular weight heparin was administrated for the prevention of thrombosis; patients with additional complications were continuously treated for 24-48 h before drainage tubes were removed. The tip–apex distance (TAD) is an important factor in the failure rate of the fixation. The average of TAD was 22.4 mm and 21.1 mm in post-op x-ray and the x-ray during follow-up at outpatient department (OPD), respectively. The bone marrow density (BMD) was obtained by X-ray detection. The BMD was 0.641 ± 0.087 g/cm2 after one postoperative day, and was 0.638 ± 0.082 g/cm2 after three postoperative days. Patients from the PFNA group could sit down and perform activities 2 days after their operations; they exercised and after 2 weeks, they could turn over by themselves. They walked with a cane after 4 weeks. Patients from the DHS group exercised the quadriceps femoris from the first day, could sit after 3 or 4 days, and could subjectively go down on their knees and hip joint by the 6th-8th day. The average days of hospitalization in each group were 9.5 days. Patients with stable fractures could walk with canes after 4 or 5 weeks; patients with unstable fractures likely received x-ray films after 8-10 weeks, and if osteoporosis was seen, patients would thereafter walk with a cane. The average harris hip score of PFNA group was 88 point, and the average harris hip score of DHS group was 78 point. The Harris hip score was significantly higher in the PFNA group than in the DHS group 3 months after surgery.
Observing indicators and assessment of effective criteria
Follow up was done at 9-18 months in all patients who underwent bone union. Operative time, bleeding volume during surgery, postoperative holding time, complications, effect, and fracture healing time were recorded. Postoperative hip joint function was based on the Harris score criteria, where function comprised 47 points, pain comprised 44 points, joint activity comprised 5 points, and malformation comprised 4 points. The total score was 100; a score of 90-100 was defined as excellent, a score of 80-90 was defined as good, a score of 70-79 was defined as middle, and a score less than 70 was defined as poor.
Statistical analysis
Statistical analysis was performed by SPSS 13.0 software and all data were presented as mean ± SD. Student t test was used to compare two samples, and q test was used to compare multiple samples. Ratio comparison was compared by chisquare test. P value <0.05 denoted a significant statistical difference.
Results
Clinical data
A total of 108 patients were enrolled in this study, including 48 males and 60 females, with ages ranging from 63 to 92 years (mean age: 75.5 years). Fifty-seven cases had left-sided fractures and 51 cases had right-sided fractures; in 71 cases, fractures were caused by leg injuries and 27 cases were caused by traffic accidents. Fractures were graded by the Evans-Jensen classification; there were 10 cases of type Ia fractures, 16 cases of type Ib, 26 cases of type IIa, 32 cases of type IIb, 14 cases of type III, and 10 cases of type IV fractures. All were closed fractures. Ten patients also had other fractures; 20 patients had coronary heart disease; 12 patients had diabetes; and 8 patients had lung diseases. X-rays showed that all patients presented with different degrees of osteoporosis. There were no significant differences in age, sex, complications, or fracture types (P>0.05).
Short-term outcomes
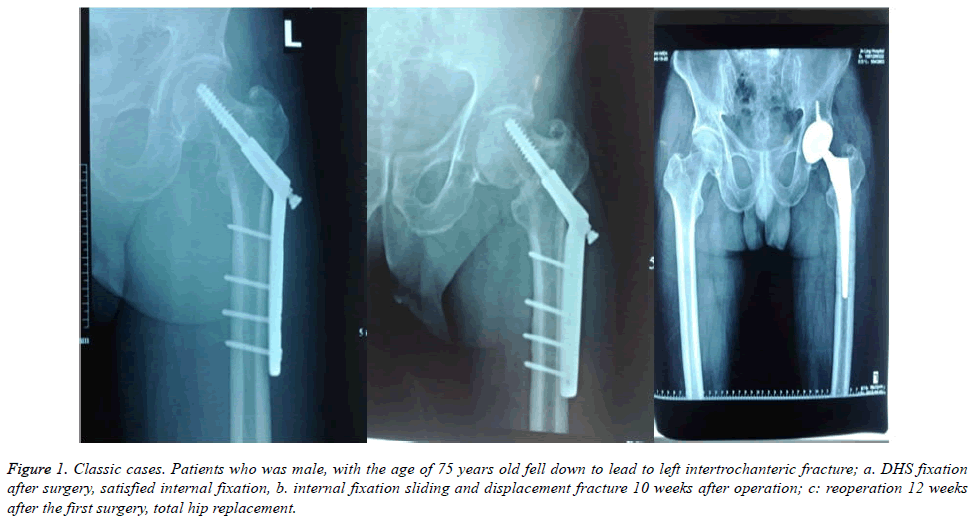
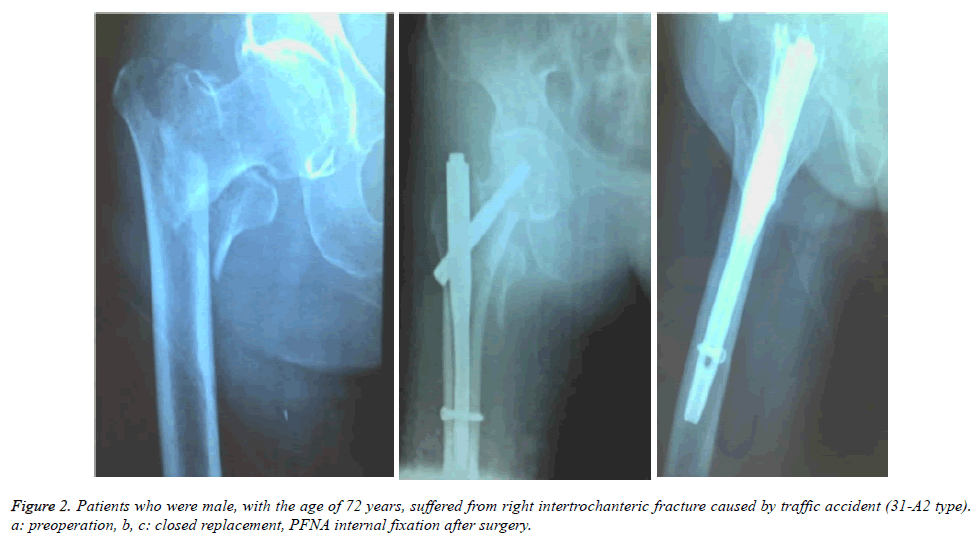
Surgical variables between the PFNA group and the DHS group were compared. The statistical difference was found between PFNA group and DHS group in terms of operative time (P=0.003). There were significant differences in intraoperative blood loss (P<0.01), loading time (P<0.01), and fracture healing time (P=0.001). Compared with the DHS group, the PFNA group had shorter operative times, less blood loss, earlier holding force in injured limbs after surgery, and shorter healing times (Table 1). More importantly, the intraoperative blood loss was significantly decreased in the PFNA group. One case of DHS was shown in Figure 1 and one case of PFNA was shown in Figure 2.
| Index | PFNA group | DHS group | P value |
|---|---|---|---|
| Operation time (min) | 45 ± 7.5 | 54 ± 16.9 | 0.003 |
| Intraoperative blood (ml) | 95 ± 25 | 160 ± 35 | <0.01 |
| Loading time (week) | 5.7 ± 1.4 | 7.1 ± 1.5 | <0.01 |
| Fracture healing time (week) | 11.6 ± 2.8 | 13.4 ± 4.2 | 0.001 |
Table 1. Comparisons of surgical effect between PFNA group and DHS group.
Figure 1. Classic cases. Patients who was male, with the age of 75 years old fell down to lead to left intertrochanteric fracture; a. DHS fixation after surgery, satisfied internal fixation, b. internal fixation sliding and displacement fracture 10 weeks after operation; c: reoperation 12 weeks after the first surgery, total hip replacement.
Post-surgical complications
Regarding the complications, there was no depinning phenomenon, necrosis of the femoral head, or deep venous thrombosis of the lower limbs in the PFNA group, but these did occur in the DHS group. Bone nonunion did not occur in either group. The incidences of coxa vara, internal fixation sliding, and delayed fracture healing were lower in the PFNA group than in the DHS group. In summary, the rate of complications was obviously lower in the PFNA group (6.52%) than in the DHS group (19.35%) (Table 2).
| Complications | PFNA group | DHS group |
|---|---|---|
| Coxa vara | 1 | 2 |
| Internal fixation sliding | 1 | 2 |
| Depinning phenomenon | 0 | 2 |
| Bone nonunion | 0 | 0 |
| Fracture delaying healing | 1 | 3 |
| Necrosis of the femoral head | 0 | 2 |
| Deep venous thrombosis of lower limb | 0 | 1 |
| total | 3 | 12 |
| Incidence rate of complications | 6.52% | 19.35% |
| Acceptance rate of functional recovery | 92% | 81% |
Table 2 Comparison of postoperative complications between PFNA group and DHS group.
Long-term outcomes of functional recovery
The postoperative functional recovery was better in the PFNA group (92%) than in the DHS group (81%) (Table 2). There were significant difference between PFNP group and DHS group (X2=5.943, P<0.05).
Discussion
Intertrochanteric fractures are prevalent in the elderly, mostly in those with osteoporosis. The elderly also suffer from severe medical diseases and many complications prior to surgery, thus the surgical risk is comparatively high. We used mostly nonoperative treatment for fractures in previous clinical practice, but long-term bed rest led to the occurrence of complications such as hypostatic pneumonia, bedsores, and venous thrombus, and the mortality rate was up to 15%-20%. In recent years, with the development of internal fixation technology and improvements in preoperative therapeutic level, surgical treatment of intertrochanteric fractures has become the consensus among a great number of medical physicians.
The key to intertrochanteric fracture therapy is to reduce the mortality rate and varus malunion. At present, the surgical methods have extramedullary and intramedullary internal fixation systems. DHS represents extramedullary internal fixation and PFNA represents intramedullary internal fixation [7,12-15].
DHS, also called the Richard nail, is a plate extramedullary fixation system and was first used in clinical practice in 1967; it was considered a major treatment for intertrochanteric fractures [16-19]. The proximal end of the armor plate and binding position of the armor plate have strong bending resistance to create strong fixation and better sliding and pressurizing function. DHS also has static and dynamic characteristics of pressurizing action, and exerts internal fixation to shrink and apply pressure on the fracture end. A sliding screw can connect an armor plate flexibly, and there is some adjustable range in the coronal and sagittal sections so as to allow convenient operation. A large operative incision, broad exposure, and large bleeding volume are the disadvantages of DHS, and DHS comprises half of all closed replacement operations. The biggest shortcoming is that DHS lacks effective internal support and poor anti-torsional strength, especially for unstable intertrochanteric fractures; the calcar femorale loses holding power and the armor plate must take on more power, which causes many complications [18,20-22], such as cutting the femur head, breaking the armor plate, or displacement fractures. Many clinical studies have indicated that DHS is adapted to stable fractures, but is not the ideal method for treating unstable intertrochanteric fractures [23-26].
PFNA is a new generation of intramedullary internal fixation systems; it was developed on the basis of PFN by the AO committee. The screw blade replaced two screws to increase pressure and counter rotation action [27-29]. Compared with DHS, PFNA has its advantages; firstly, the bearing axis of PFNA is closer to the hip joint, and the arm of force is significantly shorter. Thus, it can directly pass load to the femoral shaft, increase constant intensity, and improve the stability of mechanical repairment. Secondly, PFNA is a minimally invasive fixed system that does not remove the fractured bone ends or soft tissues, and thus protects the biological environment around the fracture. Relative to DHS, PFNA is an intramedullary device with a helical blade rather than with a screw; this allows a better purchase in the femoral head to limit cut-outs due to various deviation and rotation. In terms of reoperation, present results show that PFNA had evidence of superiority to DHS. PFNA represented the core of bone operation and minimally invasive surgery, and was favoured for fracture recovery. PFNA was designed to minimize the risk of these implant-related complications, and preliminary results suggested that this goal might have been achieved. Additionally, PFNA has other advantages, such as easy operation, short exposure time, and it does not involve reaming, thereby avoiding the occurrence of internal blood loss and maintaining low operative risk. Thirdly, the design of the screw blade locked technique is suitable for elderly patients with osteoporosis. The cross screw blade can be rotated into bone and sclerotic tissue. The pointed connecting section and sclerotic tissue form a composition of forces that strongly fixes the head of the femur; furthermore, the special shape between the blade and the major screw can limit the rotation of the screw blade, so as to achieve better support. Additionally, implantation of the screw blade is not necessary to ream the marrow in patients, which avoids bone loss. Postoperative follow-up revealed that there were fewer complications in the PFNA group than in the DHS group. Fourthly, the design of the gamma nail is hollow, and a small incision is needed to place a guide pin into the marrow cavity. Moreover, the gamma nail was designed as an eversion angle at 6 degrees, which allows it to insert conveniently at the top of the greater trochanter of the femur. The end-point locked hole is locked dynamically or statically. Finally, the extended sharp end and socket design of the gamma nail allows it to be inserted conveniently during surgery and avoids gathering forces in one position so as to reduce the incidence of broken nails and refracture with pointed nails.
Although PFNA has many advantages, some complications have occurred with the widespread use of PFNA, such as coxa vara and delayed fracture healing [28,30,31]. Therefore, we should pay attention to the following points: firstly, preoperative preparation should be complete. The femoral myelocavity must be measured accurately and the intramedullary nail should be chosen properly. If the main nail is too thin, it might move within the marrow cavity and cut the femur, causing re-fracture; if the main nail is too thick, it will fail to insert into bone. Secondly, during surgery, a traction table was used to adequately reduce the fractures under the assistance of a C-arm instrument, which was convenient when performing minimally invasive operations. It reduced trauma and shortened the operation times. Thirdly, the incisions should be cut accurately. When inserting the pin, generally choose a position internally, on the right side of the trochanteric fixation points, and avoid placing it within the sinus piriformis. In addition, the intramedullary nail should be placed precisely. If placed in the left side or too medially, the intramedullary nail could cause fracture of the calcar femorale; if the intramedullary nail is inserted externally, it could cause cortical fracture. Fourthly, the screw blade was located in the middlelower one-third portion of the femur, and the side position was located 5-10 mm below the femoral head facet, which had high bone density. This increased the holding force of the blade to reduce postoperative complications. Finally, the screw blade was screwed down to apply pressure on the fracture end. If the fracture end is larger, the length of the screw blade should be shortened. Furthermore, the screw blade should be inserted into the bone at one time in order to avoid replacement and reduced stability.
In sum, the design of PFNA is more reasonable than that of DHS, and PFNA represents BO and minimally invasive surgery. Moreover, PFNA has many advantages, such as little exposure of the fracture position, a protective blood supply, easy operation, a small wound, and few complications, which allows for the benefit of early return to function and exercise. PFNA should be a priority choice for treatment of intertrochanteric fractures with minimal rate of fixation failure, less blood loss and shorter length of hospital stay. PFNA is an ideal method to treat intertrochanteric fractures in the elderly.
Conflicts of Interest
All of the authors declare that they have no conflicts of interest regarding this paper
References
- Herman A, Landau Y, Gutman G, Ougortsin V, Chechick A. Radiological evaluation of intertrochanteric fracture fixation by the proximal femoral nail. Injury 2012; 43: 856-863.
- Koval KJ, Zuckerman JD. Hip fractures are an increasingly important public health problem. Clin Orthop Relat Res 1998; 2.
- Fan L, Dang X, Wang K. Comparison between Bipolar Hemiarthroplasty and Total Hip Arthroplasty for Unstable Intertrochanteric Fractures in Elderly Osteoporotic Patients. PLoS One 2012; 7: e39531.
- Soucanye de Landevoisin E, Bertani A, Candoni P, Charpail C, Demortiere E. Proximal femoral nail antirotation (PFN-ATM) fixation of extra-capsular proximal femoral fractures in the elderly: retrospective study in 102 patients. Orthop Traumatol Surg Res 2012; 98: 288-295.
- Siavashi B, Aalirezaei A, Moosavi M, Golbakhsh MR, Savadkoohi D. A comparative study between multiple cannulated screws and dynamic hip screw for fixation of femoral neck fracture in adults. Int Orthop 2015; 39: 2069-2071.
- Matre K, Havelin LI, Gjertsen JE, Espehaug B, Fevang JM. Intramedullary Nails Result in More Reoperations Than Sliding Hip Screws in Two-part Intertrochanteric Fractures. Clin Orthop Relat Res 2013; 471: 1379-1386.
- Garg B, Marimuthu K, Kumar V, Malhotra R, Kotwal PP. Outcome of short proximal femoral nail antirotation and dynamic hip screw for fixation of unstable trochanteric fractures. A randomised prospective comparative trial. Hip Int 2011; 21: 531-536.
- Zehir S, Zehir R, Zehir S, Azboy I, Haykir N. Proximal femoral nail antirotation against dynamic hip screw for unstable trochanteric fractures; a prospective randomized comparison. Eur J Trauma Emerg Surg 2015; 41: 393-400.
- Shen L, Zhang Y, Shen Y, Cui Z. Antirotation proximal femoral nail versus dynamic hip screw for intertrochanteric fractures: a meta-analysis of randomized controlled studies. Orthop Traumatol Surg Res 2013; 99: 377-383.
- Ma KL, Wang X, Luan FJ, Xu HT, Fang Y, Min J, Luan HX, Yang F, Zheng H, He SJ. Proximal femoral nails antirotation, Gamma nails, and dynamic hip screws for fixation of intertrochanteric fractures of femur: A meta-analysis. Orthop Traumatol Surg Res 2014; 100: 859-866.
- Xu YZ, Geng DC, Mao HQ, Zhu XS, Yang HL. A comparison of the proximal femoral nail antirotation device and dynamic hip screw in the treatment of unstable pertrochanteric fracture. J Int Med Res 2010; 38: 1266-1275.
- Fensky F, Nüchtern JV, Kolb JP, Huber S, Rupprecht M, Jauch SY, Sellenschloh K, Püschel K, Morlock MM, Rueger JM, Lehmann W. Cement augmentation of the proximal femoral nail antirotation for the treatment of osteoporotic pertrochanteric fractures--a biomechanical cadaver study. Injury 2013; 44: 802-807.
- Liu Y, Tao R, Liu F, Wang Y, Zhou Z, Cao Y, Wang H. Mid-term outcomes after intramedullary fixation of peritrochanteric femoral fractures using the new proximal femoral nail antirotation (PFNA). Injury 2010; 41: 810-817.
- Mereddy P, Kamath S, Ramakrishnan M, Malik H, Donnachie N. The AO/ASIF proximal femoral nail antirotation (PFNA): a new design for the treatment of unstable proximal femoral fractures. Injury 2009; 40: 428-432.
- Simmermacher RK, Ljungqvist J, Bail H, Hockertz T, Vochteloo AJ. The new proximal femoral nail antirotation (PFNA) in daily practice: results of a multicentre clinical study. Injury 2008; 39: 932-939.
- Inal S, Taspinar F, Gulbandilar E, Gok K. Comparison of the biomechanical effects of pertrochanteric fixator and dynamic hip screw on an intertrochanteric femoral fracture using the finite element method. Int J Med Robot 2015; 11: 95-103.
- He W, Zhang W. The curative effect comparison between prolonged third generation of gamma nail and prolonged dynamic hip screw internal fixation in treating femoral intertrochanteric fracture and the effect on infection. Cell Biochem Biophys 2015; 71: 695-699.
- Zhao W, Liu L, Zhang H, Fang Y, Pei F. Effect of dynamic hip screw on the treatment of femoral neck fracture in the elderly. Chin J Traumatol 2014; 17: 69-72.
- Zhang K, Zhang S, Yang J, Dong W, Wang S. Proximal femoral nail vs. dynamic hip screw in treatment of intertrochanteric fractures: a meta-analysis. Med Sci Monit 2014; 20: 1628-1633.
- Kazemian GH, Manafi AR, Najafi F, Najafi MA. Treatment of intertrochanteric fractures in elderly highrisk patients: dynamic hip screw vs. external fixation. Injury 2014; 45: 568-572.
- Oken OF, Soydan Z, Yildirim AO, Gulcek M, Ozlu K, Ucaner A. Performance of modified anatomic plates is comparable to proximal femoral nail, dynamic hip screw and anatomic plates: finite element and biomechanical testing. Injury 2011; 42: 1077-1083.
- Hong JY, Suh SW, Park JH, Shin YS, Yoon JR, Yang JH. Comparison of soft-tissue serum markers in stable intertrochanteric fracture: dynamic hip screw versus proximal femoral nail-A preliminary study. Injury 2011; 42: 204-208.
- Zhang L, Shen J, Yu S, Huang Q, Xie Z. Percutaneous compression plate versus dynamic hip screw for treatment of intertrochanteric Hip fractures: a meta-analyse of five randomized controlled trials. Scientific World Journal 2014; 2014: 512512.
- Wang Q, Yang X, He HZ, Dong LJ, Huang DG. Comparative study of InterTAN and Dynamic Hip Screw in treatment of femoral intertrochanteric injury and wound. Int J Clin Exp Med 2014; 7: 5578-5582.
- Upadhyay S, Raza HK. Letter to the editor: Proximal femoral locking plate versus dynamic hip screw for unstable intertrochanteric femoral fractures. J Orthop Surg (Hong Kong) 2014; 22: 130-131.
- Schwartsmann CR, Jacobus LS, Spinelli Lde F, Boschin LC, Gonçalves RZ. Dynamic hip screw for the treatment of femoral neck fractures: a prospective study with 96 patients. ISRN Orthop 2014; 2014: 257871.
- Goffin JM, Pankaj P, Simpson AH, Seil R, Gerich TG. Does bone compaction around the helical blade of a proximal femoral nail anti-rotation (PFNA) decrease the risk of cut-out?: A subject-specific computational study. Bone Joint Res 2013; 2: 79-83.
- Yaozeng X, Dechun G, Huilin Y, Guangming Z, Xianbin W. Comparative study of trochanteric fracture treated with the proximal femoral nail anti-rotation and the third generation of gamma nail. Injury 2010; 41: 1234-1238.
- Chiu CK, Chan CY, Singh VA. Is the femoral neck geometry adequate for placement of the proximal femoral nail in the Malaysian population? A review of 100 cases. Med J Malaysia 2009; 64: 22-26.
- Pu JS, Liu L, Wang GL, Fang Y, Yang TF. Results of the proximal femoral nail anti-rotation (PFNA) in elderly Chinese patients. Int Orthop 2009; 33: 1441-1444.
- Zhou F, Zhang ZS, Yang H, Tian Y, Ji HQ, Guo Y, Lv Y. Less invasive stabilization system (LISS) versus proximal femoral nail anti-rotation (PFNA) in treating proximal femoral fractures: a prospective randomized study. J Orthop Trauma 2012; 26: 155-162.